Pure Micropapillary Carcinoma of the Male Breast: Report of A Rare Case
Received: 18-May-2016 / Accepted Date: 19-Oct-2016 / Published Date: 25-Oct-2016 DOI: 10.4172/2572-4118.1000113
Abstract
Objective: Breast carcinoma in men represents 1% of all breast cancers. The micropapillary carcinoma (MPC) of the breast is a morphologically distinctive form accounting for 2.7% of ductual carcinoma in which the tumor cells are arranged in morule-like clusters. A pure MPC of the breast is very rare. This report describes a pure micro papillary carcinoma in a 36-year old man, with clinical, pathological and immunohistochemical features.
Methods: We present a case of this rare type of breast cancer diagnosed in a male patient and summarize the current literature to date. The patient presented with a painless mass measuring 1 cm in great diameter adhering to superficial and deep planes. A microbiopsy was performed and the final histopathology revealed a pure MPC of the male breast in more than 50% of tumor’s volume. On immunohistochemical investigations of the specimen, tumor’s cells stained for GCDFP15 and showed high expression of estrogen, progesterone antibodies. We had completed by lumpectomy with axillary dissection which found 14 lymph nodes including 2 metastatic lymph nodes.
Results: The MPC differs histologically from conventional papillary carcinoma of the breast, which typically exhibits a complex arborescent growth pattern within cystically dilated duct-line space. A secondary MPC of the breast must be researched as a differential diagnosis of primary MPC, especially micropapillary variant of transitional carcinoma of the bladder and MPC of the lung. Immunohistochemically, the positivity of GCDFP-15 in breast cancers and the positivity of TTF-1 in lung cancers are useful in distinguishing them.
Conclusion: MPC is a special subtype of invasive ductal carcinoma with an aggressive nature. Despite the small number of studies, MPC of the breast is undoubtedly not rare. Recognition of this relatively rare entity is important in predicting metastasis to lymph nodes and distant sites regardless of tumor size. Axillary and distant metastasis should be evaluated to determine the therapeutic strategy.
Keywords: Micropapillary carcinoma; Breast cancer; Male; Cytology; Immunohistochemistry; Pseudopapillary; Tamoxifen
35839Abbreviations
MCP: Micropapillary Carcinoma; GCDFP-15: Gross Cystic Disease Fluid Protein 15; TTF-1: Thyroid Transcription Factor 1; HER-2: Human Epidermal Growth Factor Receptor 2; MIB-1: Methylation-Inhibited Binding Protein 1
Introduction
Invasive micropapillary carcinoma (IMPC) is a rare variant of invasive ductal carcinoma of the breast first described as a distinct histologic subtype by both Petersen and Siriaunkgul in 1993 [1]. Breast carcinoma in men is a relatively rare disease with an incidence of nearly 1% of all breast cancers; it accounts for less than 1% of all cases of cancer in men. Although male breast carcinoma tends to behave more aggressively than female carcinoma, the prognosis of this neoplasm is excellent [2]. The most common histological subtype of invasive breast carcinoma is infiltrating ductual carcinoma, which accounts for about 85% of all tumors [3]. The incidence of micropapillary carcinoma (MPC) of the breast was 2.7% and 1%for the lobular carcinoma. MPC is a morphologically distinct form of ductual carcinoma in which the tumor cells are arranged in morule like clusters. A pure MPC of the breast is very rare [4]. It is associated with a high incidence of axillary lymph node metastases, local recurrence and poor prognosis [5]. This report describes a pure micropapillary carcinoma in a 36-year-old man, with clinical, pathological and immunohistochemical features.
Methods
Formalin-fixed sections from the primary tumor and contiguous tissue were available. Samples from the four quadrants, the nipple, and the sub areolar area were examined. Axillary lymph node dissection was performed. Paraffin-embedded sections were performed. The number of H and E-stained slides reviewed was 24.
The tumor grade was evaluated using the modified Bloom- Richardson scoring system. Immunohistochemically using the following primary antibodies were tested: cytokeratin AE1/AE3 (DakoPatts, Santa Barbara, CA), GCDFP-15 (Signet Laboratories, Dedham, MA), estrogen receptor (Ventana), progesterone receptor (Ventana), HER-2/neu (clone CB11, BioGenex), and MIB-1 (Ventana). Appropriate positive and negative controls were included.
Case Description and Results
A 36-year-old male presented with a painless mass in the right breast for few months. By physical examination, we noticed a hard, elastic, well-defined mass measuring 1×1 cm and adhering to both superficial and deep aponevroses. No significant lymphadenopathy was present in the cervical, supraclavicular, and axillary regions. Mammographic examination of the right breast showed astellar mass measuring 12 mm diameter, without microcalcification or axillary lymph node enlargement. These clinical and radiological features were suspicious of malignancy. An ultrasound guided core biopsy of the area was then done and revealed a pure MPC of the male breast in more than 50% of tumor’s volume.
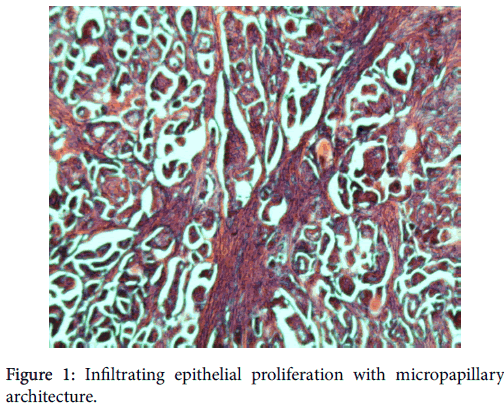
On microscopic examination, the tumor showed a highly distinctive architecture characterized by tufts of cells arranged in pseudopapillary structures devoid of fibrovascular cores and surrounded by empty, clear spaces lined by delicate strands of fibro collagenous stroma (Figure 1).
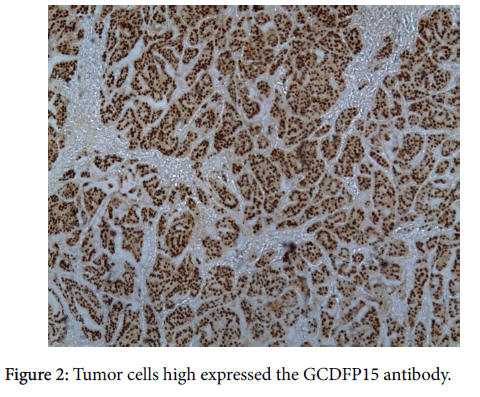
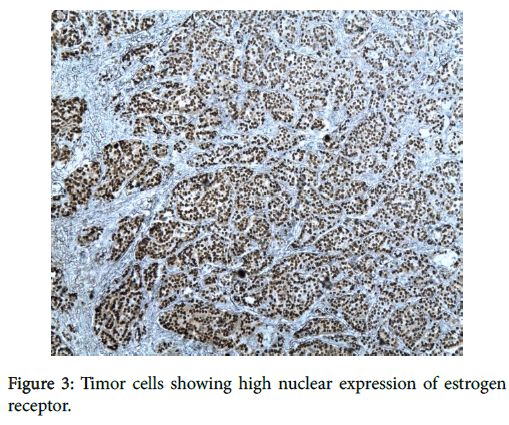
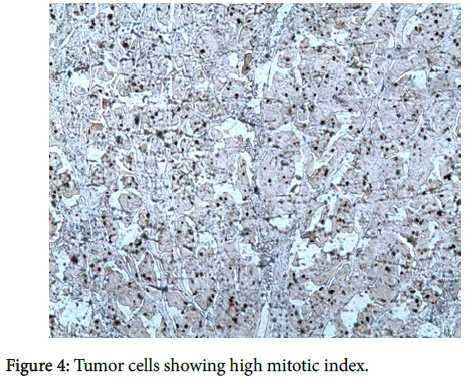
Tumor cells were moderately atypical with a high mitotic index (10 mitoses/10 large fields). There was no vessel invasion. Using the modified Scarf-Bloom-Richardson scoring system, we graded the tumor as moderately differentiated (stage II).On immunohistochemical investigations, tumor’s cells stained for GCDFP15 (Figure 2) and for estrogen (ER) (Figure 3) and progesteron receptor (PR) while Thyroid transcriptase factor-1 (TTF-1) was negative.
The expression of HER2 oncogen was strongly positive (score 3+). The proliferation index (Mib-1) was evaluated to 60% (Figure 4). The patient underwent enlarged lumpectomy with sentinel node biopsy. It was completed by a total mastectomy with axillary dissection. Fourteen lymph nodes were examined; 2 nodes were metastatic. The patient started adjuvant chemotherapy with paclitaxel followed by doxorubicin and cyclophosphamide. He also received adjuvant radiotherapy. However, he had metastases to the liver 12 months later. The patient died two years later having aseptic shock.
Discussion
Invasive micropapillary carcinoma of the breast is an uncommon, aggressive and distinct histological type of invasive ductal carcinoma. Review of the literature on invasive micropapillary breast carcinoma revealed 27 retrospective cohort studies and case series. The overall incidence of invasive micropapillary carcinoma among the retrospective cohort studies was found to be 1297 out of 331,486 cases (0.4%) of invasive breast cancer. This corresponds to 3-6% IMPC incidence rate. Excluding the study by Chen et al. and using the National Cancer Institute’s Surveillance, Epidemiology, and End Results (NCI SEER) database, the reported incidence rises to 537 out of 27,876 cases (1.93%) of newly diagnosed invasive breast cancer. This difference may reflect a degree of bias related to the retrospective nature of the cohort studies published to date on this rare tumor phenotype.
The male breast cancers might result from autosomal dominant mutations, primarily BRCA1 or BRCA2 mutations in 4% to 40% [6]. The MPC touched old men with a medium age of 63 years old [7], which is different from our case where the patient was younger (36 years old).
Morphologically, compared to invasive ductal breast carcinoma (IDC), MPC is characterized by cells arranged in pseudopapillary structures that are composed of cell clusters with inverted polarity and surrounded by clear empty spaces lined by delicate strands of fibrocollagenous stroma [8].
The MPC differs histologically from conventional papillary carcinoma of the breast [9], which typically exhibits a complex arborescent growth pattern within cystically dilated duct-line space. A secondary MPC of the breast must be researched as a differential diagnosis of primary MPC, especially micropapillary variant of transitional carcinoma of the bladder and MPC of the lung [10], both of which tumor scan exactly mimic the histological appearance of primary MPC of the breast. Immunohistochemically, the positivity of GCDFP-15 in breast cancers and the positivity of TTF-1 in lung cancers are useful in distinguishing them [7].
In our case, the presence of tubular architecture proved that the lesion was a primary breast carcinoma, GCDFP15 positivity with TTF-1negativity are additional diagnostic features. Another unique characteristic of MPC was the high percentage of ER and PR positivity, which was nearly the double of the expected percentage of HER-2 positivity [11]. Our results were in accordance with literature; however, a Turkish case [7] showed a negativity expression of estrogen and progesteron receptor (ER, PR). MPC displays an aggressive nature [12]. At diagnosis, it frequently shows extensive lymphatic-vessel invasion and the incidence of axillary node metastasis in MPC is reported to be 67-90% [13]. In our case, the patient had two metastatic lymph nodes.
Conclusions
In conclusion, MPC is a special subtype of invasive ductal carcinoma with an aggressive nature. Despite the small number of studies, MPC of the breast is undoubtedly not rare. Recognition of this relatively rare entity is important in predicting metastasis to lymph nodes and distant sites regardless of tumor size. Axillary and distant metastasis should be evaluated to determine the therapeutic strategy.
References
- Siriangkul S, Tavassoli FA (1993) Invasive micropapillary carcinoma of the breast. Mod Pathol 6: 660-662.
- Kelessis NG, Georgiou IT, Markidou S, Papadopoulos S, Coclami TE (2011) Papillary carcinoma of the male breast: Report of a case. Surgery Today 41: 537-541.
- Heller KS, Rosen PP, Schottenfeld D, Ashikari R, Kinne DW (1978) Male breast cancer: a clinicopathologic study of 97 cases. Ann Surg 188: 60-65
- Nassar H, Wallis T, Andea A, Dey I, Adsay V, et al. (2001) Clinicopathologic analysis of invasive micropapillary differentiation in breast carcinoma. Mod Pathol 14: 836-841.
- Qing Cui Z, Feng JH, Zhao YJ (2015) Clinicopathological features of invasive micropapillary carcinoma of the breast. Oncol Lett Mar 9: 1163-1166
- Fentiman IS, Fourquet A, Hortobagyi GN (2006) Male breast cancer.Review. Lancet 367: 595-604.
- Erhan Y, Erhan Y, Zekioglu O (2005) Pure invasive micropapillary carcinoma of the male breast: report of a rare case. J Can Surg 48: 2
- Liu Y, Huang X, Bi R, Yang W, Shao Z (2014) Similar Prognoses for Invasive Micropapillary Breast Carcinoma and Pure Invasive Ductal Carcinoma: A Retrospectively Matched Cohort Study in China. PLoS One 9: e106564
- Joshi N, Pande C (1998) Papillary carcinoma of the male breast diagnosed by fine needle aspiration cytology. Indian J Pathol Microbiol 41: 103-106.
- Amin MB, Ro Jy, el-Sharkawy T, Lee KM, Troncoso P,et al. (1994)Micropapillaryvariant of transitional cell carcinoma of the urinary bladder. Am J Surg Pathol 18: 1224-1232
- Luna-More S, Gonzalez B, Acedo I, Rodrigo I, Luna C (1994) Invasive micropapillary carcinoma of the breast. Pathol Res Pract 190: 668-674.
- Middleton LP, Tressera F, Sobel ME, Bryant BR, Alburquerque A, et al. (1999) Infiltrating micropapillary carcinoma of the breast. Mod Pathol 12: 499-504.
- Tsushimi T, Mori H, Harada T, Ikeda T, Ohnishi H (2013) Invasive micropapillary carcinoma of the breast in a male patient: Report of a case. Int J Surg Case Rep 4: 988-991
Citation: El Hadj OEA, Chaar I, Goucha A, Belghith M, El May A, et al. (2016) Pure Micropapillary Carcinoma of the Male Breast: Report of A Rare Case. Breast Can Curr Res 1: 113. DOI: 10.4172/2572-4118.1000113
Copyright: ©2016 El Hadj OEA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 12120
- [From(publication date): 12-2016 - Jul 30, 2025]
- Breakdown by view type
- HTML page views: 11213
- PDF downloads: 907