Radiological Assessment by Digital Tomosynthesis with Metal Artifact Reduction Technology for Total Hip Arthroplasty
Received: 11-Jul-2020 / Accepted Date: 17-Aug-2020 / Published Date: 24-Aug-2020 DOI: 10.4172/2167-7964.1000329
Abstract
Objective: To evaluate the advantages of digital tomosynthesis over radiography in the assessment of total hip arthroplasty (THA) in clinical settings.
Patients and Methods: (1) In the prospective study, 90 THAs of 150 primary cemented THAs performed with bulk bone grafting for dysplastic hips were assessed postoperatively for up to 5 years. (2) In the retrospective study, radiography and digital tomosynthesis were performed on 832 consecutive hips that underwent THA and were referred for valuation of bone structure, bone reactions around prostheses, and remodeling of grafted bones. The tomosynthesis images were compared with anterior-posterior radiographs with regard to demarcation (radiolucent zone, RLZ).
Results: (1) In the radiographic assessment of 90 hips with acetabular bone graft reconstruction, bridging trabeculation, remodeling, and reorientation were observed at 4.6 ± 2.3, 9.0 ± 3.7, and 16.1 ± 5.8 postoperative months, respectively. In contrast, these bone reactions were observed on tomosynthesis at 9.8 ± 2.7, 17.4 ± 4.9, and 27.3 ± 6.7 months, respectively (p < 0.05). (2) In the evaluation of THAs in this study, digital tomosynthesis was found to provide better visualization of bone reactions structures around prostheses, and demarcations between prostheses and bones than radiography. In the evaluation of 804 cemented socket cases, the RLZ in zone 1 was identified in 118 cases on radiography and in 197 cases on tomosynthesis (p < 0.05).
Conclusions: In the evaluation of THA, digital tomosynthesis provided better visualization of bone reactions, structures around prostheses, and demarcations between cemented or cementless prostheses and bones than radiography.
Keywords: Digital tomosynthesis; Metal artifact reduction technology; Radiological assessment; Total hip arthroplasty
Introduction
Hip joints have routinely been evaluated after total hip arthroplasty (THA) using plain radiography and plain computed tomography (CT). However, radiographic evaluations and CT assessments are limited by overlapping structures and metal artifacts, respectively. There have been advancements in X-ray assessments such as the possibility of taking radiographs in standing position and the introduction of the digital filmless style that uses high-quality monitors [1]. CT systems do not allow for scans to be performed in the standing position and as Xray radiography only produces 2-dimensional representations, detailed 3-dimensional evaluation of inner hip structures cannot be performed by X-ray radiography. CT produces high-resolution scans in the transverse plane, but not in the frontal or sagittal planes. Earlier X-ray tomography systems produced images that were of too poor a resolution to be clinically relevant and were discontinued in most medical institutions due to low image quality. In contrast, X-ray digital tomosynthesis, which was recently developed and produces image resolutions of high quality, is now used for clinical assessment. We have been using tomosynthesis for primary evaluation after THA for about 5 years and have compared it with radiography.
Conventional radiographs [2] have routinely been used for the assessment of cement fractures and radiolucent zones (RLZs) along the cement-bone or cement-prosthesis interface in THAs. The acetabular cup may be evaluated according to DeLee and Charnley’s classification [3] or the study by Hodgkinson et al. [4] and the femoral stem according to the Gruen scale [5] or the Barrack grading system [6]. Due to its tomographic nature, CT is superior to radiography in the evaluation of RLZs, bone structures, and osteolysis [7]. However, difficulties are experienced with both radiological methods when evaluating the prosthesis-bone or prosthesis-cement interface because of metal artifacts. These difficulties persist even with the creation of artifact-reducing image reconstruction algorithms [8].
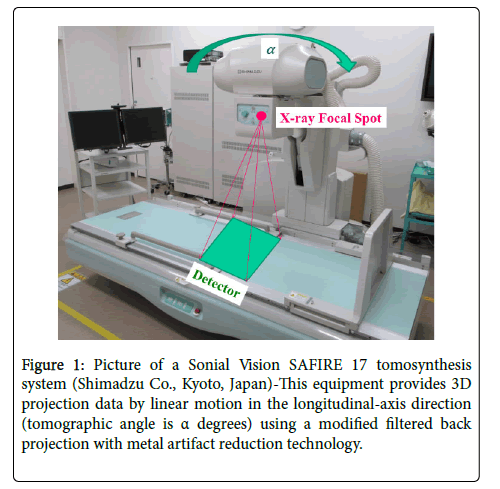
This study was aimed at evaluating the clinical application of digital linear tomosynthesis in the imaging of total hip prostheses and the surrounding bones using a new tomosynthesis technology with metal artifact reduction from Shimadzu Sonial Vision Safire Tomosynthesis Shimadzu Metal Artifact Reduction Technology, T-SMART) (Figure 1). In the evaluation of THA cases, the tomosynthesis images were compared with radiographic images. The purpose of this study was to evaluate the additional diagnostic usefulness of tomosynthesis in the assessment of THAs.
Figure 1: Picture of a Sonial Vision SAFIRE 17 tomosynthesis system (Shimadzu Co., Kyoto, Japan)-This equipment provides 3D projection data by linear motion in the longitudinal-axis direction (tomographic angle is α degrees) using a modified filtered back projection with metal artifact reduction technology.
Patients and Methods
Digital linear tomosynthesis was introduced to our institution on August 29, 2013. This study was approved by the institutional ethical committee in October, 2013. The study was conducted using 2 groups. Deceased patients and patients who were unable to visit the outpatient clinic for postoperative follow-up due to serious illness unrelated to the surgery were excluded from this study.
Study group -1 (for the assessment of grafted bones in THAs): This group consisted of 70 patients who underwent 90 THAs of 150 primary cemented THAs performed with bulk bone grafting for dysplastic osteoarthritic hips between November 2013 and October 2015 (prospective study). All the cemented components were manufactured by KYOCERA Medical Corporation, Osaka, Japan, a company known as Japan Medical Materials Corporation between September 2004 and March 2012. Clinical follow-up was performed semiannually using radiography and tomosynthesis. Graft incorporation and healing were evaluated in a time-dependent pattern for the 90 THAs performed with bulk bone grafting [9]. Furthermore, based on the criteria proposed by Knight et al. [10] we assessed bridging, graft remodeling, and trabeculation using tomosynthesis and radiography.
Study group -2 (for the assessment of bone reactions in THAs): This group consisted of patients who underwent THA and were examined in an outpatient clinic between November 2015 and October 2018 and referred for evaluation of bone structure, bone reactions around prostheses, and remodeling of grafted bones using radiography and digital tomosynthesis (retrospective study). The THAs consisted of 768 primary THAs and 64 revision THAs performed at our hospital between January 1997 and October 2015 on patients with osteoarthritis, avascular necrosis, and rheumatoid arthritis. The patient demographics are shown in Table 1. Most of the patients were diagnosed as osteoarthritis and cemented cup were used for majority cases. Tomosynthesis images were also compared to anterior-posterior (AP) radiographs regarding demarcation (RLZ), extent of demineralization (stress shielding), and osteolysis. The acetabular components consisted of 804 cemented sockets and 28 cementless shells, and the femoral components consisted of 450 cemented stems and 382 cementless double- tapered stems. All of the cemented acetabular sockets and the cemented femoral stems, and 354 cementless femoral stems were manufactured by KYOCERA Medical Corporation. The 28 cementless acetabular components and the remainder of the cementless femoral components were manufactured by PETER BREHM GmbH, Weisendorf, Germany. There were no simultaneous bilateral hip replacement cases in the patient groups.
| Primary OA | Dysplastic OA | Traumatic OA | RA | AVN | RDC | Neuro-pathic | Ankylosis | Revision | Total | |
|---|---|---|---|---|---|---|---|---|---|---|
| Cement Cup | 53 | 655 | 10 | 7 | 8 | 8 | 2 | 1 | 60 | 804 |
| Metal Shell | 8 | 4 | 4 | 1 | 7 | 0 | 0 | 0 | 4 | 28 |
OA: Osteoarthritis, RA: Rheumatoid arthritis, AVN: Avascular necrosis, RDC: Rapidly destructive coxarthrosis
Table 1: Patient demographics.
A senior surgeon and junior surgeon independently evaluated these radiographic images using uniform criteria. The radiographic and tomosynthesis images were examined according to DeLee and Charnley’s classification 3 for the sockets and Gruen’s classification 5 for the stems within the scope of the retrospective cohort study for study group-2.
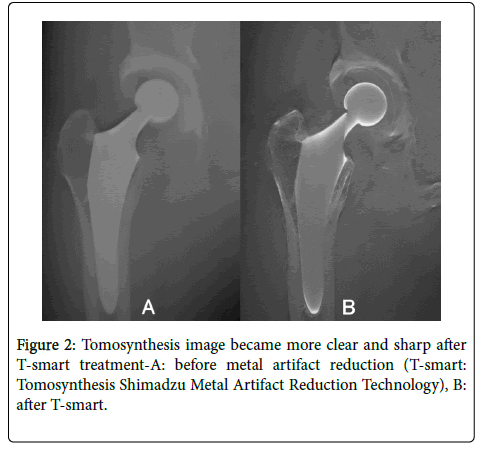
Tomosynthesis images were obtained using a digital radiography/ fluoroscopy system (SonialVisions Safire 17; Shimadzu Corporation, Kyoto, Japan) (Figure 2). This system consisted of an X-ray tube (0.7 and 1.2 mm focal spots) and a 432×432 mm digital flat- panel detector (2,880×2,880 pixels, amorphous selenium) with pixel size of 150 μm. The tomosynthesis imaging mode was the 2×2 pixel-binning mode, and the pixel size of the tomosynthesis was 300 μm. The X-ray tube and detector moved synchronously in opposite directions while acquiring images at a tomographic angle of 40ᵒ for 74 projections. The X-ray tube had a voltage of 80 kV and a current of 400 mA at 6.3 ms per projection. An anti-scatter grid was used. The X-ray source-todetector distance was 1,100 mm and the projected image was automatically transferred to a dedicated workstation for tomosynthesis image reconstruction (Figure 1) [11].
Statistical analysis
We used the 2010 version of the software (SSRI® Inc., Tokyo, Japan) to conduct statistical analysis and Microsoft Excel® (Microsoft Corp., Redmond, WA, USA) for descriptive statistics. The probability of progression and change of the RLZs were analyzed using the Mantel- Haenszel test. Paired t-tests were used to compare the radiographic parameters of bone graft incorporation. Statistical significance was defined as p values less than 0.05 in all the analyses.
Results
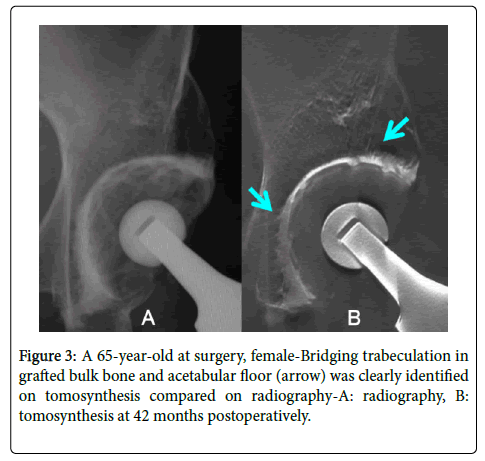
In the 90 hips with acetabular bone graft reconstruction, cemented sockets were rigidly fixed by incorporating the bulk bone graft and the impacted autologous morselized bone and there was no radiographic evidence of resorption of the impacted bone graft over 3 to 5 years of follow-up in any of the cases. The gaps between the bulk bone graft and the acetabular roof reduced in size over time and stable fixation of the graft was maintained in all cases. We observed that additional structural bulk bone grafting had a time-dependent incorporation pattern. In some cases with bulk bone grafting, partial incorporation of the graft was seen on tomosynthesis even though full incorporation of the bone graft was visualized on radiography (Figure 3).
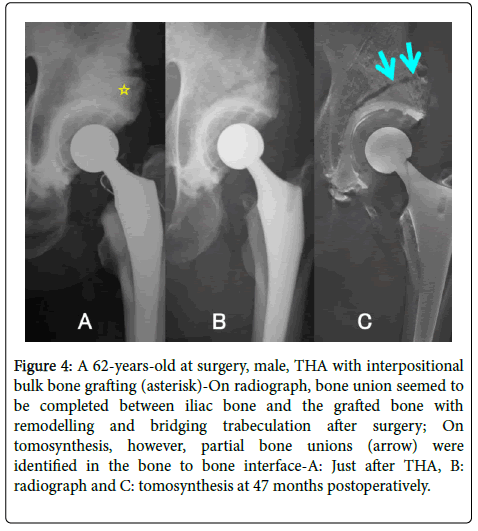
Postoperative radiographic assessment revealed bridging trabeculation at 4.6 ± 2.3 (mean ± standard deviation, SD) months (range, 2-12 months), remodeling at 9.0 ± 3.7 months (range, 2–30 months), and reorientation at 16.1 ± 5.8 months (range, 6–42 months). In contrast, postoperative tomosynthesis assessment revealed bridging trabeculation at 9.8 ± 2.7 (mean ± SD) months (range, 6-18 months), remodeling at 17.4 ± 4.9 months (range, 12-36 months), and reorientation at 27.3 ± 6.7 months (range, 18-48 months) (Table 2). In cemented socket cases, bridging trabeculation in additional or interpositional bulk grafted bone and acetabular floor was commonly more clearly identified on tomosynthesis than on radiography (Figure 4).
| (n = 80) | Cement Cup | ||
|---|---|---|---|
| Status | Radiograph | Tomosynthesis | Paired t-test |
| Bridging trabeculation | 4.6 ± 2.3 | 9.8 ± 2.7 | p < 0.05 |
| Remodeling | 9.0 ± 3.7 | 17.4 ± 4.9 | p < 0.05 |
| Reorientation | 16.1 ± 5.8 | 27.3 ± 6.7 | p < 0.05 |
Table 2: Comparison of postoperative periods (months) of grafted bulk bone status in the cemented cup between radiography and tomosynthesis.
Figure 4: A 62-years-old at surgery, male, THA with interpositional bulk bone grafting (asterisk)-On radiograph, bone union seemed to be completed between iliac bone and the grafted bone with remodelling and bridging trabeculation after surgery; On tomosynthesis, however, partial bone unions (arrow) were identified in the bone to bone interface-A: Just after THA, B: radiograph and C: tomosynthesis at 47 months postoperatively.
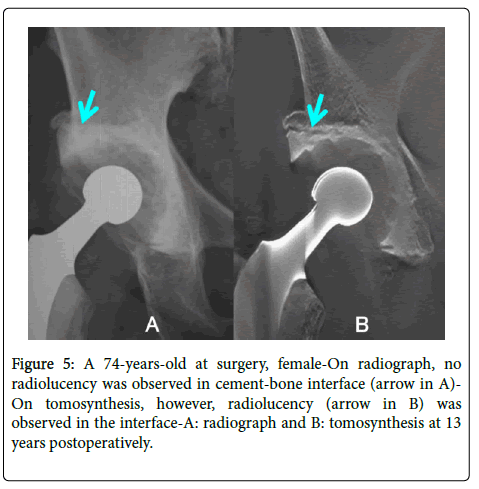
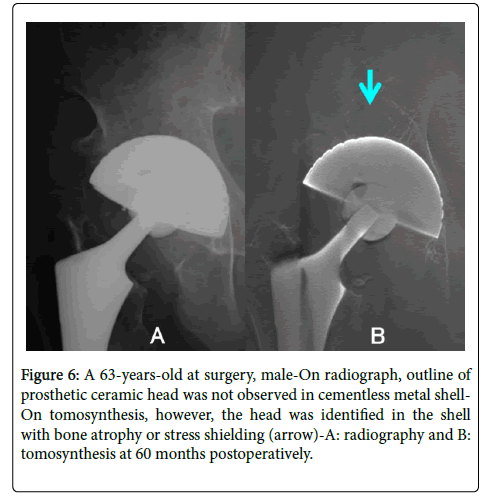
In the radiographic evaluation of the cemented socket cases, RLZ was observed in zone 1 in 118 cases. In the assessment of the tomosynthesis images of the same series, RLZ was observed in the same zone in 197 cases (Figure 5). There were significant differences between radiography and tomosynthesis in the occurrence of RLZ in the cemented socket (p < 0.05) (Table 3). In contrast, there were no significant differences in the cementless metal shell (Table 4). Stress shielding around the pole area was observed on tomosynthesis imaging in 3 cases of cementless THAs (Figure 6).
Figure 6: A 63-years-old at surgery, male-On radiograph, outline of prosthetic ceramic head was not observed in cementless metal shell-On tomosynthesis, however, the head was identified in the shell with bone atrophy or stress shielding (arrow)-A: radiography and B: tomosynthesis at 60 months postoperatively.
| N=804 | Cement Cup | |
|---|---|---|
| Zone 1 | Radiography | Tomosynthesis |
| RLZ(+) | 118 | 197 |
| RLZ(-) | 686 | 607 |
p < 0.05(Mantel-Haenstzel method)
Zone 1: Proximal site of the socket (DeLee and Charnley), RLZ: radiolucent zone
Table 3: Comparison of rates of radiolucent zone occurrence in socket zone 1 (cement cup) between radiography and tomosynthesis.
| N=28 | Metal Shell | |
|---|---|---|
| Zone 1 | Radiography | Tomosynthesis |
| RLZ(+) | 1 | 4 |
| RLZ(-) | 27 | 24 |
Not Significant(Mantel-Haenstzel method)
Zone 1: Proximal site of the socket (DeLee and Charnley), RLZ: radiolucent zone
Table 4: Comparison of rates of radiolucent zone occurrence in socket zone 1 (metal shell) between radiography and tomosynthesis.
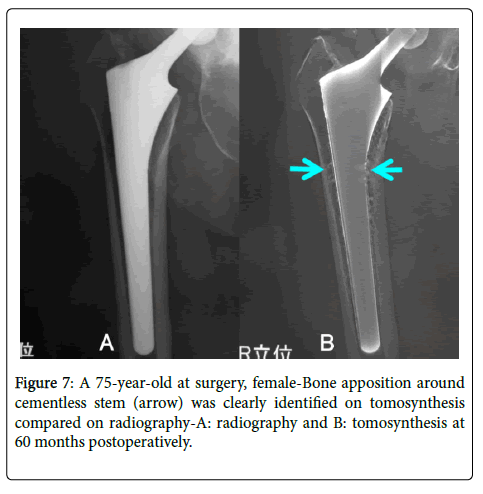
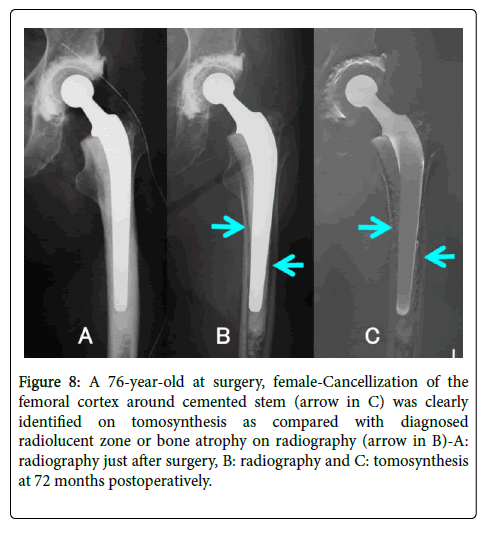
With regard to the femoral components, bone apposition around cementless stems in Gruen’ s zones 1-7 was more identifiable on tomosynthesis than on radiography (Figure 7). Cancellization of the femoral cortex around cemented stems with diagnosed RLZ or bone atrophy in Gruen’ s zones 2-7 was more frequently identified on tomosynthesis than on radiography (Figure 8).
Figure 8: A 76-year-old at surgery, female-Cancellization of the femoral cortex around cemented stem (arrow in C) was clearly identified on tomosynthesis as compared with diagnosed radiolucent zone or bone atrophy on radiography (arrow in B)-A: radiography just after surgery, B: radiography and C: tomosynthesis at 72 months postoperatively.
Discussion
Tomosynthesis as a radiological imaging tool was developed several decades ago [12]. Ziedses des Plantes [13] provided the theoretical base for tomography in the 1930s. The term “tomosynthesis” was coined by Grant [14] in 1972. Some variants of tomosynthesis, such as “ ectomography, ” created by Edholm et al., [15] and flashing tomosynthesis [16] for rapid imaging in vascular applications, emerged in the 1970s and 1980s.
In the past 2 decades, digital tomosynthesis has been dramatically developed and investigated in breast and chest imaging. In clinical radiological evaluations, tomosynthesis uses lower X-ray dose levels and is and less expensive than CT and it also provides metal artifact reduction [12]. It can change the mode of detection and evaluation of breast cancer and pulmonary nodules [17,19]. In this study, the usefulness of digital linear tomosynthesis in assessing THAs were demonstrated particularly with regard to the structure and quality of bones around prostheses [11]. Bone remodeling, trabeculation, radiolucency, and stress shielding of metal shells and stems were routinely assessed on radiography. We re-evaluated these parameters using tomosynthesis and compared the results with those of radiography.
Although CT is ideal for the radiological evaluation of weightbearing hip joints, CT systems do not allow for scans to be performed in the standing position with weight bearing situation. CT produces images of high quality and resolution in the tomographic transverse plane, but images of low quality and resolution in the frontal (coronal) and axial (sagittal) planes. In addition, CT images of patients with metal implants such as hip prostheses have artifacts, which appear as bright and dark streaks [19] and may make correct radiological diagnosis impossible [11]. To circumvent these difficulties experienced with CT scans, the new tomosynthesis with metal artifact reduction or T-SMART was introduced for the assessment of hip arthroplasties with metallic components.
It may be possible to analyze bone reactions and structures around prostheses, such as bone apposition, remodeling, trabecular formation in grafted bones, RLZs, and stress shielding around femoral stems, cemented acetabular sockets, and cementless acetabular shells with metal artifact reduction, more accurately with tomosynthesis than with CT. Radiological assessment of THAs in standing position of patients in the frontal (coronal) plane which is not feasible with CT, can be performed using tomosynthesis.
In the current study, bone reactions and structures around prostheses were more easily identified in the AP projection with tomosynthesis than with radiography (Figures 2-8). The bone reactions and demarcation between prostheses and surrounding bones were more distinct in thin tomosynthesis sections than in projection radiographs, with no interference from overlying soft tissues. However, these changes were also fairly detectable with radiography in most cases, and tomosynthesis provided more details. As a result, tomosynthesis increased diagnostic confidence and partially changed radiographic diagnosis, such as with the evaluation of RLZs (Table 3) and healing of grafted bones (Table 2).
Metal shells without screws used in cementless THAs were fixed using spherical locking mechanisms. In half of the cases (14 shells), the metal shells were fixed without screws. Although acetabular stress shielding may not be as critical as femoral stress shielding, it was observed around the pole area in 3 cases evaluated using tomosynthesis imaging (Figure 5).
We observed in this study that tomosynthesis was advantageous in that it can be quickly and easily performed after radiography with no need to reschedule the patient, the same radiographic equipment (Xray image table) is used in the same radiography suite as for conventional radiography, and it adds only about 5 minutes to the total examination time. The effective radiation dose of hip radiography in the AP projection (not including the cross-table lateral view) was reported to generally be 0.88 mSv, with a wide range of values. 8 In this study, the effective radiation dose of the CT examination of hip joints that had undergone THA is 10 mSv, which is more than 5 times that of radiography (1.7 mSv for 2 images, such as A-P and lateral view images), while the radiation dose of a tomosynthesis scan is reported to be 3.5 mSv.
The main limitations of this study are that the cementless acetabular components were small in number and did not, therefore, allow for differentiation of results between cemented and uncemented stems. However, the objective of this study was to evaluate the additional diagnostic usefulness of tomosynthesis in THA and not to evaluate the different prosthesis types. The second limitation of this study is that, except for evaluations involving bulk bone grafting, the images were retrospectively reviewed. In all the cases, tomosynthesis provided a more detailed evaluation but did not change the radiographic diagnosis. The third limitation of this study, when only AP radiographs are used, is that the prostheses could not adequately be evaluated in the lateral radiographic view. The improved differentiation and visualization of bone reactions and structures around prostheses with tomosynthesis in the current study were only in the AP projection. Linear tomosynthesis cannot generate reconstructions like other imaging techniques, such as 3-dimensional CT. Thus, tomosynthesis cannot replace conventional radiography and CT, but it can serve as an adjunct providing more detailed information in the standing AP projection.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
In conclusion, digital tomosynthesis provided more detailed information in the evaluation of THAs in the form of improved visualization of bone reactions, structures around prostheses, and demarcations between cemented or cementless prostheses and bones in this study than radiography. Tomosynthesis can change radiographic assessment after THA.
Acknowledgments
The authors wish to thank Minoru Hasegawa, M.D., Tadashi Arai, and Akira Mita, Department of Radiology, Minaminagano Medical Center, Shinonoi General Hospital for their excellent assistance and advice.
References
- Maruyama M, Tensho K, Wakabayashi S, Hisa K (2014) Standing versus supine radiographs to evaluate femoral head penetration in the polyethylene liner after total hip arthroplasty. J Arthroplasty 29:2415-2419.
- McCaskie AW, Brown AR, Thompson JR, Gregg PJ (1996) Radiological evaluation of the interfaces after cemented total hip replacement: interobserver and intraobserver agreement. Journal of Bone and Joint Surgery B 78:191-194.
- DeLee JG, Charnley J (1976) Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res 121:20-32.
- Hodgkinson JP, Shelley P, Wroblewski BM (1988) The correlation between the roentgenographic appearance and operative findings at the bone-cement junction of the socket in Charnley low friction arthroplasties. Clinical Orthopaedics and Related Research 228:105-109.
- Gruen TA, McNeice GM, Amstutz HC (1979) ‘Modes of failure’ of cemented stem-type femoral components. A radiographic analysis of loosening. Clinical Orthopaedics and Related Research 141:17-27.
- Barrack RL, Mulroy RD, Jr., Harris WH (1992) Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty: a 12-year radiographic review. Journal of Bone and Joint Surgery B 74:385-389.
- Miller TT (2012) Imaging of hip arthroplasty. European Journal of Radiology 81:3802-3812.
- Göthlin JH, Geijer M (2013) The utility of digital linear tomosynthesis imaging of total hip joint arthroplasty with suspicion of loosening: a prospective study in 40 patients. Biomed Res Int 594631.
- Garvin KL, Bowen MK, Salvati EA, Ranawat CS (1991) Long-term results of total hip arthroplasty in congenital dislocation and dysplasia of the hip. A follow-up note. J Bone Joint Surg Am 73:1348-1354.
- Knight JL, Fujii K, Atwater R, Grothaus L (1993) Bone-grafting for acetabular deficiency during primary and revision total hip arthroplasty. A radiographic and clinical analysis. J Arthroplasty 8:371-382.
- Gomi T, Hirano H (2008) Clinical potential of digital linear tomosynthesis imaging of total joint arthroplasty. J Digit Imaging 21:312-322.
- Dobbins JT (2009) Tomosynthesis imaging: at a translational crossroads. Med Phys 36:1956-1967.
- Ziedses des Plante BG (1932) Eine neue methode zur differenzierung in der roentgenographie (planigraphie) Acta Radiol 13:182-192.
- Grant DG (1972) Tomosynthesis. A three-dimensional radiographic imaging technique. IEEE Trans Biomed Eng 19:20-28.
- Edholm P, Granlund G, Knutsson H, Petersson C (1980) Ectomography: A new radiographic method for reproducing a selected slice of varying thickness. Acta Radiol 21:433-442.
- Becher H, Schluter M, Mathey DG, Bleifeld W, Klotz E, et al. (1985) Coronary angiography with flashing tomosynthesis. Eur Heart J 6:399-408.
- Dobbins JT, McAdams HP, Song JW, Li CM, Godfrey DJ, et al. (2008) Digital tomosynthesis of the chest for lung nodule detection: Interim sensitivity results from an ongoing NIH-sponsored trial. Med Phys 35:2554-2557.
- Suryanarayanan S, Karellas A, Vedantham S, Glick SJ, D’Orsi CJ, et al. (2000) Comparison of tomosynthesis methods used with digital mammography. Acad Radiol 7:1085-1097.
- Hsieh J (1995) Image artifacts, causes, and correction. In: Goleman LW, Fowlkes JB, editors. Medical CT and ultrasound, current technology and applications. Madison: Advanced Medical Publishing 487-518.
Citation: Maruyama M, Nomura H (2020) Radiological Assessment by Digital Tomosynthesis with Metal Artifact Reduction Technology for Total Hip Arthroplasty. OMICS J Radiol 9: 1000329. DOI: 10.4172/2167-7964.1000329
Copyright: © 2020 Maruyama M, this is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3260
- [From(publication date): 0-2020 - Dec 15, 2025]
- Breakdown by view type
- HTML page views: 2424
- PDF downloads: 836