Results of Ankle Arthrodesis with Talarlock®-Plate in High Risk Patients
Received: 27-Apr-2019 / Accepted Date: 10-May-2019 / Published Date: 17-May-2019
Abstract
Background: The tibiotalar arthrodesis is an established salvage procedure in case of contraindications for ankle replacement. The plate fixation compared to the screw or nail fixation has been more stable in former biomechanical studies. The open or arthroscopic screw arthrodesis and ankle arthrodesis with anterior plates does not lead to advantages for the postoperative treatment. Limitations result out of the immobilization of the lower leg in a plaster in high risk patients.
Methods: In a retrospective study 58 consecutive patients with posterolateral plate arthrodesis of the ankle were included. Clinical and radiological assessments were performed preoperatively, six weeks, three months and one year postoperatively. Patients were prescribed an arthrodesis boot to wear for six weeks and were allowed full weight bearing.
Results: 50% of the patients had a neuromuscular disorder and belonged to a high risk group. AOFAS score improved significantly postoperative. The hind foot axis was corrected to physiological values. No pseudarthrosis occurred in the study. In one patient delayed bone healing was registered without any symptoms. Two patients (3.4%) required revision surgery because of wound healing problems and in two patients a hardware removal was necessary. In three patients a lesion of N. suralis was occurred.
Conclusion: The high rate of patients with neuromuscular disease and polyneuropathy (50%) with postoperaive mobilisation with full weight bearing did not lead to higher complication rate including nonunion.
Keywords: Ankle arthrosis; Osteoarthrosis; Hind foot deformity; Neuromuscular disease; Arthrodesis; Tibiotalar arthrodesis; Hind foot arthrodesis
Level of Evidence
Level III (USPSTF).
Introduction
The tibiotalar arthrodesis is an established salvage procedure for number of indications, especially in patients with contraindications for ankle replacement. Various methods for osteosynthesis and approaches have been described previously [1-6]. The diversity of techniques with variable results and complications confirm that a universal method is not established. The plate fixation compared to the screw or nail fixation has been more stable in former biomechanical studies [7-9]. The main limitation of ventral plate fixation for ankle arthrodesis with double plate systems and additional lag screws is the morbidity due to the extended anterior approach [6,9-12]. The positioning of two anterior plates is challenging in small ankles, so that occasionally additional screws or thinner plates have to be used. Summing up, no significant advantages for the postoperative treatment has been reported in the literature. The authors suggested the immobilization of the lower leg in a plaster for eight weeks [12]. No further results of the posterolateral plate arthrodesis could be shown up in the literature review. The objective of this work was to analyse the clinical results of the ankle arthrodesis with posterolateral Talarlock®-plate (Intercus GmbH, Zu den Pfarreichen 5, 07422 Bad Blankenburg, Germany).
Methods
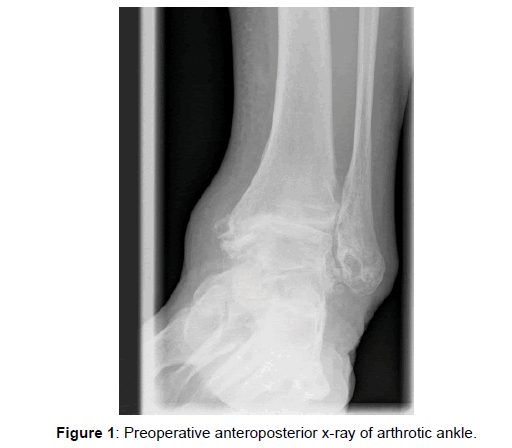
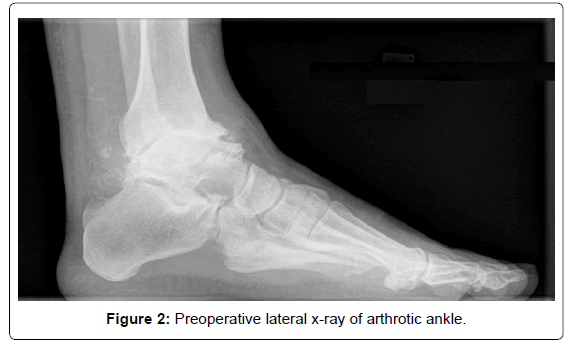
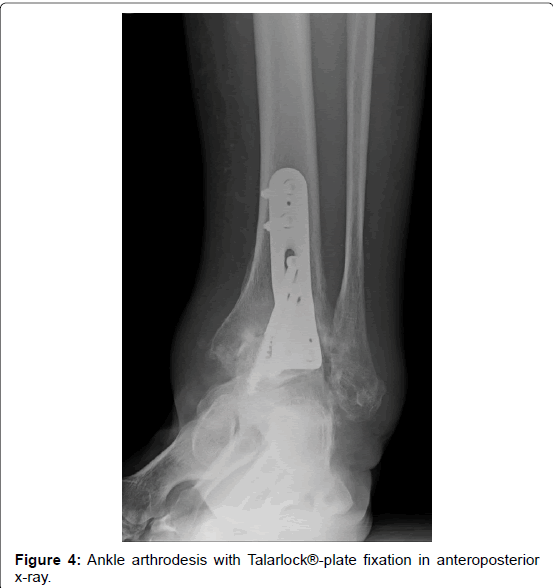
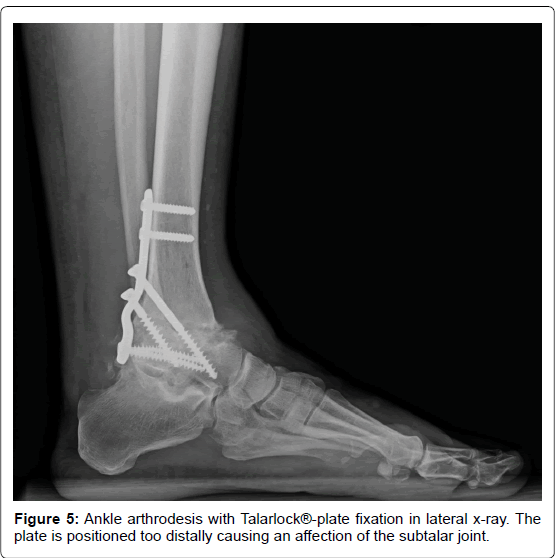
In a retrospective study 58 consecutive patients (59 ankles) with posterolateral plate arthrodesis of the ankle were included (Figures 1-3). Two experienced foot and ankle surgeons performed the operations at two different hospitals. One patient with Charcot-Marie-Tooth disease received an ankle arthrodesis on both sides. The Talarlock®- plate was used as a standard implant since 2011 at our clinic (Figures 4-6). Patient data are summarized in Tables 1-3.
| n | Women/men | Age (years) | BMI (kg/m2) |
|---|---|---|---|
| 59 | 32/26 | 64 (54 -72) | 31.4 (27.2-34.6) |
Table 1: Patient data (HF=Hind Foot; RA=Rheumatoid Artritis).
| Neurological disorder | Diabetes mellitus | Posttraumatic | RA | smoker | HF-Varus | HF-Valgus |
|---|---|---|---|---|---|---|
| 29 | 14 | 21 | 8 | 14 | 28 | 30 |
Table 2: Risk factors.
| n | CMT | Neurofibromatosis | Polyneuropathy | Critical illness |
|---|---|---|---|---|
| 29 | 13 | 1 | 14 | 1 |
Table 3: Classification of neurological disorders (CMT=Charcot-Marie-Tooth).
Fourteen patients claimed preoperatively of sensory deficit in the affected foot. In 11 the symptoms were attributed to neuropathy. Three patients had postraumatic arthritis and previous surgery of the ankle.
The surgery is performed with patient in prone position and the leg slightly inverted. An aproximatly 10-12 cm skin incision is required between the fibula and the Achilles tendon. Due to variable location a careful preparation of the Nervus suralis and often attendant Vena saphena parva was succeeded. After the incision of the faszia cruris and the mobilization of the musculus flexor hallucis longus and musculus tibialis posterior the capsula of the ankle was resected and the ankle joint exposed. Using a joint distractor the cartilage of the talus, tibia, malleolus medialis and lateralis was removed and the required preparation with multiple drilling of the arthrodesis surfaces performed. An osteotomy osteotomy of the fibula was performed through the approach if required. The ankle was set in plantigrade position and pinned with k-wire. The proper position of the Talarlock®-plate was proved via fluoroscopy. First the two proximal locking screws were inserted. The proximal lag screw was put into the corpus tali und the distal lag screw was targeting the collum tali. Finally, the two distal locking screws were inserted into talus. A 10 mm redon was used for drainage before the softtissue and skin were closed [8].
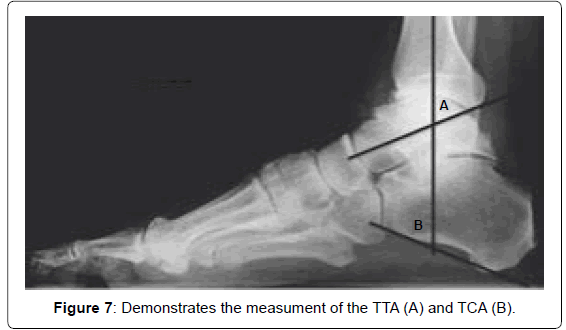
Clinical and radiological assessments were performed preoperatively, six weeks, three months and one year postoperatively. Anterior and lateral X-rays as well as long hind foot views were done whilst weight bearing. The hindfoot axis, tibiotalar (TTA) and tibiocalcaneal (TCA) angle were measured. The X-rays were analysed using the digital measuring system PACS (Picture Archiving and Communication System) (Figure 7). The equinus position of the foot was defined with the TTA <70° and TCA >70° [13-15]. AOFAS (American Orthopaedic Foot and Ankle Society) Score was evaluated preoperatively and one year postoperatively. Patients with hind foot varus and valgus deformity were divided in two groups and the results were considered separately. Additionally, results of high risk patients with neuromuscular disease were analysed.
Patients were prescribed an arthrodesis boot to wear for six weeks and were allowed full weight bearing from the beginning. One patient received a plaster and was mobilized with floor contact for six weeks because of large bone defects and required bone grafting. Presence of postoperative sensory deficit on the medial, plantar and lateral skin of the foot was registered. The t test and the χ2 test were used for statistical analysis.
Results
The AOFAS score improved significantly from 41 (± 5.1) points preoperatively to 69.9 (± 4.6) points one year postoperatively (p=0.00001). There were no significant difference between patients with varus and valgus deformity.
The Hind Foot Axis (HFA) decreased significantly from a mean 16.4° (± 8.7°) varus preoperatively to 0.6° (± 1.3°) varus one year postoperatively (p=0.000003) and 5.2° (± 3.3°) valgus preoperatively to 2.2° (± 1.1°) valgus postoperatively (p=0.0018). Further radiological results are summarized in Table 4.
| Group | HF axis pre (degree) | HF axis post (degree) | TTA pre | TTA post | TCA pre | TCA post |
|---|---|---|---|---|---|---|
| Varus | 16.4(±8.7) | 0.6 (±1.3) | 58.2 (±7.1) | 73.8 (±4.8) | 75.4 (±7.1) | 68.5 (±7.6) |
| P (pre/post) | - | 0.000003 | - | 0.0002 | - | 0.00001 |
| Valgus | 5.3 (± 3.3) | 2.2 (±1.1) | 66.2 (±7.2) | 73.1 (±2.3) | 60.3 (±8.1) | 64.4 (±7.1) |
| P (pre/post) | - | 0.0018 | - | 0.002 | - | >0.05 |
| P (varus/valgus | - | >0.05 | - | >0.05 | - | >0.05 |
Table 4: Results of radiological measurements with mean and standard deviation values.
One patient with diabetes and one with posttraumatic arthritis and several previous ankle operations required revision because of wound healing problems (6.4%). Further 3 patients had a prolonged wound healing without need for revision. One patient suffered a stair fall after surgery with periimplant fracture of the talus and distal tibia. The tibio calcaneal arthrodesis with retrograde intramedullary nail was performed as salvage procedure. A fusion was achieved 12 weeks after surgery without any other complication.
Nine patients claimed about numbness of the lateral foot postoperatively. Six of them recovered 6 weeks postoperatively and further one 12 weeks postoperatively. A sensory deficit of lateral foot remained in three patients (5%). Two of them had diabetes and one a posttraumatic artritis with several previous ankle operations and revision due to wound healing problems (Table 5).
| n | Revision | Pseudarthrosis | N. suralis injury | Hardware removal |
|---|---|---|---|---|
| 59 | 2 | 0 | 3 | 2 |
Table 5: Complications of both groups.
However, there was one case of delayed bone healing in patient with posttraumatic ankle arthrosis with failure of one lag screw without any further implant dislocation. The patient performed protected full weight bearing in an arthrodesis boot for 8 weeks. In CT scans the fusion was achieved 8 months postoperatively. The patient reported no pain or discomfort while full weight bearing from the beginning. He returned to work 14 weeks after surgery and started bicycling 4 months after surgery. According to the patient request an implant removal was necessary in two patients.
Discussion and Conclusion
Although a variety of surgical techniques for ankle arthrodesis have been described so far, no outstanding universal method has been established [2]. The retrograde tibiotalocalcanear nails have been often applied with different results. The compression nails could improve the fusion rate with divergent results in the literature [4,6,13,16-18]. O’Neill et al., report a fusion rate of 76% in 34 patients after ankle arthrodesis with retrograde compression nail [19]. In contrast, Nielsen et al., indicate a fusion rate of 96% [18]. The main limitations of retrograde hindfoot nails include an intact subtalar joint and pronounced axial deformity of the tibia with displaced medullary canal [20]. Isolated tibiotalar arthrodesis with antegrade compression nail with a fusion rate of 90% was described by Mückley [6,13]. An advantage of this method is the possibility of compression and isolated arthrodesis of the ankle. However, the method is technically demanding and has not been widely used [13]. The screw arthrodesis is the most commonly used technique for isolated ankle arthrodesis [1,2,5,20-23]. Different techniques with two to five screws are described with different results in biomechanical studies. Mueckley et al., showed in a biomechanical study similar stiffness of three-screw arthrodesis compared to a compression nail [4]. A number of authors postulate that screw arthrodesis provides insufficient rigidity and primary stability in severe misalignment of the ankle, poor bone quality and osteoporosis [24,25]. Postoperative plaster treatment and longer period of immobilization and partial weight bearing are recommended [1,26]. Advantages of fewer complications, shorter hospital stay, better clinical scores in the arthroscopic arthrodesis could be demonstrated in the systematic review of Peterson et al. [27]. The results stated in the review should be rated with caution due to different inclusion criteria of the studies considered in the review. Patients with higher misalignment underwent mainly open surgery, so that no final conclusions can be stated. However, a number of studies showed considerable pain reduction, improved function, faster postoperative recovery and better short term outcome of arthroscopic ankle arthrodesis [28-31]. Schmid et al., demonstrated in a retrospective study higher rate of complications and lower rate of fusion in open ankle arthrodesis compared to arthroscopic arthrodesis. A fusion rate of 98% in 50 patients was demonstrated in the arthroscopic arthrodesis versus 83% in the open arthrodesis [29]. Similar fusion results were shown in the study of Mueckley et al. [32]. However, a number of authors prefer to apply the arthroscopic arthrodesis in patients with less to moderate misalignment [12,15,23,31- 33]. Simons et al. concluded that in patients with normal tibia plafond angle and simple tilting of the talus the arthroscopic arthrodesis can be applied. Patients with major deformities of the tibia plafond require bone resection, therefore open approach is often used [13].
In the present study no pseudarthrosis occurred. In one patient we observed a delayed bone healing without any symptoms. The fusion was registered in computed tomography 8 months after surgery. Two patients (6.4%) required revision surgery because of wound healing problems and in two patients a hardware removal was necessary. The subtalarjoint was affected by the plate in one patient (Figure 5) and one patient felt discomfort and requested the removal of the plate. A CT scan proved the fusion before implant removal. In three patients a persistant lesion of Nervus suralis with postoperative numbness of the lateral foot was registered. Two of them had diabetes and one multiple surgery of the ankle in consequence of trauma. Intraoperative identification is recommended due to the variable location of Nervus suralis [8,26,34]. Functional results are comparable to the results in other studies [5,10,11,20,31,35,36]. In all patients hindfoot correction succeeded to physiological values.
The high rate of patients with neuromuscular disease and polyneuropathy (50%) did not lead to higher complication rate including nonunion. Results of arthroscopic arthrodesis with screws in comparable high risk patient group could not be found in the literature. The postoperative mobilisation of patients with neuromuscular disease and polyneuropathy with partial weight bearing, as required in screw arthrodesis or ventral plate arthrodesis, is challenging [37]. The patients in the present study were mobilized with full weight bearing in a arthrodesis boot without negative influence on the results. Regarding the small number of patients no final statements can be made. The literature review and own experience show that a high fusion rate and a significant reduction of complications can be achieved with arthroscopic arthrodesis of the ankle using screws. In severe misalignment and high risk patients a more stable osteosynthesis may be required. In a previously performed biomechanical study a significantly higher stiffness of the Talarlock®-plate was demonstrated. The advantage of the implant is the combination of locking and lag screws and the position of the implant on the tension side of the ankle. The posterolateral plate arthrodesis is established as a standard procedure in high risk patients with neurological disorders at our clinic. The main disadvantage of the study is the results were not compared with a control group and the retrospective character. The results are encouraging but do not allow final statements. Randomised studies are required to confirm our results.
Conflict of Interest
No conflict of interests.
References
- Endres T, Grass R, Rammelt S, Zwipp H (2005) Ankle arthrodesis with four cancellous lag screws. Oper Orthop Traumatol 17:345-360.
- Grass R, Zwipp H (1998) The arthrodesis of the upper ankle in the four-screw technique. Oper Orthop Traumatol 10:134-142.
- Mears DC, Gordon RG, Kann SE, Kann JN (1991) Ankle arthrodesis with an anterior tension plate. Clin Orthop Relat Res 268:70-77.
- Mueckley T, Hofmann G, Buhren V (2005) Tibiotalar arthrodesis with the tibial compression nail. Oper Orthop Traumatol 17:407-425.
- Tkachenko-Bril AL, Jagos H, Pils K, Gaudernak J, Rafolt D (2018) Proof of concept of a partial weight-bearing supporting real-time feedback system. Stud Health Inform 248:286-292.
- Mueckley T, Klos K, Drechsel T, Beimel C, Gras F, et al. (2011) Short-term outcome of retrograde tibiotalocalcaneal arthrodesis with a curved intramedullary nail. Foot Ankle Int 32:47-56.
- Gutteck N, Martin H, Hanke T, Matthies JB, Heilmann A, et al. (2018) Posterolateral plate fixation with Talarlock is more stable than screw fixation in ankle arthrodesis in a biomechanical cadaver study. Foot Ankle Surg 24:208-212.
- Park JH, Kim HJ, Suh DH, Lee JW, Kim HJ, et al. (2018) Arthroscopic versus open ankle arthrodesis: A systematic review. J Arthroscopy 34:988-997.
- Thermann H, Hufner T, Roehler A, Tscherne H (1996) Screw arthrodesis of the ankle joint. Technique and outcome. Der Orthopade 25:166-176.
- Mohamedean A, Said HG, El-Sharkawi M, El-Adly W, Said GZ (2010) Technique and short-term results of ankle arthrodesis using anterior plating. Int Orthop 34:833-837.
- Quayle J, Shafafy R, Khan MA, Ghosh K, Sakellariou, et al. (2018) Arthroscopic versus open ankle arthrodesis. Foot Ankle Surg 24:137-142.
- Wülker N, Flamme CH, Muller A, Wirth CJ (1997) 10 years follow-up of athrodeses of the hindfoot joints and upper ankle joint. Z Orthop Ihre Grenzgeb 135:509-515.
- Simons GW (1978) A standardized method for the radiographic evaluation of clubfeet. Clin Orthop Relat Res 135:107-118.
- Tarkin IS, Mormino MA, Clare MP, Haider H, Walling AK, et al. (2007) Anterior plate supplementation increases ankle arthrodesis construct rigidity. Foot Ankle Int 28:219-223.
- Winson IG, Robinson DE, Allen PE (2005) Arthroscopic ankle arthrodesis. J Bone Joint Surg Br 86:343-347.
- Jehan S, Shakeel M, Bing AJ, Hill SO (2011) The success of tibiotalocalcaneal arthrodesis with intramedullary nailing: A systematic review of the literature. Acta Orthop Belg 77:644-651.
- Mueckley TM, Eichorn S, Hoffmeier K, von Oldenburg G, Speitling A, et al. (2007) Biomechanical Evaluation of primary stiffness of tibiotalocalcaneal fusion with intramedullary nails. Foot Ankle Int 28:224-231.
- Nielsen KK, Linde F, Jensen NC (2008) The outcome of arthroscopic and open surgery ankle arthrodesis: A comparative retrospective study on 107 patients. Foot Ankle Surg 14:153-157.
- O'Neill PJ, Logel KJ, Parks BG, Schon LC (2008) Rigidity comparison of locking plate and intramedullary fixation for tibiotalocalcaneal arthrodesis. Foot Ankle Int 29:581-586.
- Friedman RL, Glisson RR, Nunley JA (1994) A biomechanical comparative analysis of two techniques for tibiotalar arthrodesis. Foot Ankle Int 15:301-305.
- El Idrissi M, Mechchat A, Elayoubi A, Shimi M, Elibrahimi A, et al. (2014) Ankle arthrodesis: Technic and results: About 10 cases. Pan Afr Med J 17:80.
- Kitaoka H (2013) Master techniques in orthopaedic surgery: Foot and Ankle. Wolters Kluwer Health.
- Zwipp H, Grass R (2005) Ankle arthrodesis after failed joint replacement. Oper Orthop Traumatol 17:518-533.
- Cheng YM, Chen SK, Chen JC, Wu WL, Huang PJ, et al. (2003) Revision of ankle arthrodesis. Foot Ankle Int 24:321-325.
- Collman DR, Kaas MH, Schuberth JM (2006) Arthroscopic ankle arthrodesis: Factors influencing union in 39 consecutive patients. Foot Ankle Int 27:1079-1085.
- Klaue K, Borsic D (2005) Posterolateral approach to the ankle for arthrodesis. Oper Orthop und Traumat 4:380-391.
- Peterson KS, Lee MS, Buddecke DE (2010) Arthroscopic versus open ankle arthrodesis: A retrospective cost analysis. J Foot Ankle Surg 49:242-247.
- Jones CR, Wong E, Applegate GR, Ferkel RD (2018) Arthroscopic ankle arthrodesis: A 2-15 Year follow-up study. J Arthroscopy 34:1641-1649.
- Schmid T, Krause F, Penner MJ, Veljkovic A, Younger ASE, et al. (2017) Effect of preoperative deformity on arthroscopic and open ankle fusion outcomes. Foot Ankle Int 38:1301-1310.
- Vaishya R, azizi AT, Agarwal AK, Vijay V (2017) Arthroscopic assisted ankle arthrodesis. A retrospective study of 32 cases. J Clin Orthop Trauma 8:54-58.
- Vanderwilde R, Staheli LT, Chew DE, Malagon V (1988) Measurements on radiographs of the foot in normal infants and children. J Bone Joint Surg Am 70:407-415.
- Mueckley TM, Eichorn S, von Oldenburg G, Speitling A, DiCicco JD (2006) Biomechanical evaluation of primary stiffness of tibiotalar arthrodesis with intramedullary compression nail and four other fixation devices. Foot Ankle Int 814-820.
- Wirth SH, Klammer G, Espinosa N (2013) Arthrodesis and endoprostheses of the ankle joint: Indications, techniques and pitfalls. Unfallchirurg 116:797-805.
- Gutteck N, Lebek S, Zeh A, Gradl G, Delank KS, et al. Ankle arthrodesis with an posterolateral approach using a polyaxial angle stable Talarlock® plate. Oper Orthop Traumatol 25:615-6923.
- Niinimäki TT, Klemola TM, Leppilahti JI (2007) Tibiotalocalcaneneal arthrodesis with compressive retrograde intramedullary nail: A report of 34 consecutive patients. Foot Ankle Int 28:431-434.
- Plaass C, Knupp M, Barg A, Hintermann B (2009) Anterior double plating for rigid fixation of isolated tibiotalar arthrodesis. Foot Ankle Int 30:631-639.
- Townshend D, Di Silvestro M, Kraue F, Penner M, Younger A, et al. (2013) Arthroscopic versus open ankle arthrodesis: A multicenter comparative case series. J Bone Jt Surg Am 95:98-102.
Citation: Gutteck N, Schilde S, Delank KS, Wesseler B (2019) Results of Ankle Arthrodesis with Talarlock®-Plate in High Risk Patients. Clin Res Foot Ankle 7:290.
Copyright: © 2019 Gutteck N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 4142
- [From(publication date): 0-2019 - Dec 22, 2025]
- Breakdown by view type
- HTML page views: 3229
- PDF downloads: 913