Research Article Open Access
Risk Factors for Maternal Vitamin D Deficiency within the United Arab Emirates
Hussein Izzeldin1, Zainab Taha2, Tewfik Ihab3, Badawi Salah4, Siddieg Hisham5, Adegoye Amanda6 and McGrady Kyle6*
1Institute of Brain Chemistry and Human Nutrition, UK
2Zayed University College of Natural and Health Sciences, Abu Dhabi, UAE
3Department of Human and Health Sciences, University of Westminster, UAE
4National Project for control of Diabetes Coordinator, National IDD Control Program, Ministry of Health, UAE
5Rashid Centre for Diabetes and Research, Ministry of Health, UAE
6Faculty of Science and Technology, Department of Life Sciences Human Food, Nutrition and Public Health Division, University of Westminster, London, UK
- *Corresponding Author:
- McGrady Kyle
Faculty of Science and Technology
Department of Life Sciences Human Food, Nutrition and Public Health Division
University of Westminster, London, UK
Tel: 19788182002
E-mail: Kyle.jd.mcg@gmail.com
Received Date: August 31, 2016; Accepted Date: September 26, 2016; Published Date: September 30, 2016
Citation: Izzeldin H, Taha Z, Ihab T, Salah B, Hisham S, et al. (2016) Risk Factors for Maternal Vitamin D Deficiency within the United Arab Emirates. J Preg Child Health 3: 276. doi:10.4172/2376-127X.1000276
Copyright: © 2016 Izzeldin H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Pregnancy and Child Health
Abstract
Introduction: Vitamin D deficiency during pregnancy is a public health problem and it has been associated with negative pregnancy outcomes for both mothers and infants. Aim: To estimate the prevalence of vitamin D deficiency in pregnant women in the United Arab Emirates (UAE) and to identify the contribution of risk factors to the 25(OH)D levels. Methods: It is a cross-sectional study in which vitamin D levels of 1088 adult pregnant women were assessed. Information on vitamin D intake was available in a sub-sample of 266 women. Results: The mean serum 25(OH)D was 26.2 nmol/L (95% CI 25.2-27.1 range 5-129.1 nmol/L) with 69% of women being vitamin D deficient (<30 nmol/L). In the bivariate analysis, showed that no predictors could have been indicated as no values exceeded significance (p<0.2). Stepwise multiple linear regression analysis could not be applied to identify predictors of vitamin D levels as no values exceeded p=0.2. Conclusion: Due to the high prevalence of vitamin deficiency in UAE, there is an urge for interventions focusing on supplementation, fortification and diet diversity for preventing health consequences during a critical period of development.
Keywords
Vitamin D; Pregnancy; United Arab Emirates; Crosssectional study
Introduction
Vitamin D deficiency is a worldwide public health problem [1]. Sunlight exposure is the primary source of vitamin D for most people, as UVB radiation (wavelength 290-320 nm) or artificial UVB light produce vitamin D3 in the skin [2]. Only 10% of vitamin D is obtained from the diet. Unfortunately, vitamin D deficiency is a prevalent condition even in tropical and subtropical countries [1]. Emirati women are usually restricted to stay indoors [3]. Regardless of cultural restrictions, the weather in the United Arab Emirates (UAE) can get extremely hot, reaching temperatures of 45°C (117°F), forcing people to spend a majority of the day indoors within air conditioned buildings, especially between June and September, which is the hottest period of the year. Those who spend time indoors are not able to produce any cholecalciferol from 7-dehydrocholesterol due to the altered UVB light through the window pane [4]. This lack of availability to the outside environment may inhibit women’s exposure to UVB light, which is required for the formation of the inactive form of vitamin D [5]. Furthermore, women are required to wear either a burka or head scarf once they have reached puberty, which limits the amount of sunlight that can reach the skin.
As the UAE became prosperous, a Westernized diet soon followed. Obesity is on the rise in the UAE with 33.5% of the population defined as obese (body mass index (BMI)>30 kg/m2) [6]. With its high general prevalence, obesity is also common among pregnant women, which can be of great concern as vitamin D could be sequestered out of the blood and into adipose tissue mass of obese subjects because of its hydrophobic properties [7]. Little is known about the longitudinal changes of 25(OH)D during the course of gestation, but there is evidence that 25(OH)D serum concentration seem to decrease as the pregnancy continues as a more recent study showed that 31% of mother to be, were at serum concentrations of adequate at the antenatal visit, 23% after birth of the child and 17% at 6 months postpartum [8].
Vitamin D is vital to the developing foetus and maternal vitamin D deficiency has been associated with a number of negative pregnancy outcomes, such as: low birth-weight, preterm birth, preeclampsia and surgical delivery [9-12]. In the UAE, a 3rd of the nation's resources are spent on pregnancy complications that are associated with preeclampsia, Page 3_ of _22 preterm birth, low birth-weight and caesarean section due to a flat pelvis and poor growth of the placenta [13]. It is estimated that 6.1% of births in the UAE are reported to be of low birth-weight (<2.5 kg) [14].
Pregnancy is a period of severe physiological changes in maternal organ systems and adaptations in the metabolism of vitamin D to ensure calcium requirements for fetal bone mineralization [15]. However, proposed cut offs of serum 25(OH)D concentrations for optimal, deficiency and insufficient levels are still controversial. The Institute of Medicine [16] suggested the following values of <30 nmol/L (12 ng/mL), 30-50 nmol/L (12-20 ng/mL) and ≥ 50 nmol/L (≥ 20 ng/mL) for deficiency, insufficiency and Adequate, respectively. While the new clinical guidelines from the Endocrine Society recommended maintaining a serum 25(OH)D concentration ≥ 75 nmol/L (≥30 ng/mL) to maintain bone health. In the UK, the current guidelines suggest a serum concentration >25 nmol/L (12 ng/mL) as this is the current threshold used to define increased risk of rickets [17].
Although vitamin D deficiency in the UAE is not a recent discovery, there is a lack of nationally representative data to provide an accurate picture of the problem. Previous studies have shown that in 1997, 25% of pregnant women in the UAE had 25(OH)D Concentrations lower than 10 nmol/L [18]. Previous studies with modest sample sizes had estimated that the average 25(OH)D concentrations ranges from 17.6 nmol/L [19] to 20.5 nmol/L [20]. Therefore, this study aims at estimating the prevalence of vitamin D deficiency in pregnant women in the UAE and to identify risk factors for low 25(OH)D levels in a nationally representative sample with the intention to build the foundation for a successful intervention strategy in the future.
Methods
This is a cross-sectional study conducted from 15th of February 2014 to the 11th of August 2014. Participants were recruited on the criteria that they were pregnant, willing to provide blood, and not reporting any medical conditions. There was no restriction regarding the gestational age at recruitment. Participants were recruited from their respective primary health care centres within 12 districts: Riga, Riffa, Umm Al-Quwain (UAQ), Ras Al Khaimah (RAK), Garain, Sabka, Fuj, Riqqa, Musheriff, Wasit, Hamidyia and North Hamidyia. Nurse members of the research team in each health centre invited women to participate in the study. The study was conducted according the guidelines proposed by the Helsinki Declaration. The study was approved by the Corniche Hospital Research Ethics Committee. All participants were informed about the study with a complete discussion of its purpose, benefits, and potential risks and provided written informed consent. Blood specimens were collected from participants who had not used any regular medications, or had any chronic medical conditions that might affect fetal growth. Five millilitre venous blood samples were obtained from the participants by qualified nurses. The blood samples were sent to Rashid Centre for Diabetes Laboratory in Ajman within two hours of collection and stored at -80 until analyzed. The blood specimens were analysed using the gold-standard liquid chromatography tandem mass spectrometry (LCMS/ MS) method for measurement of 25(OH)D3 status or using Liaison 25 OH vitamin D TOTAL Assay (310600) as an alternative analytical technique in Rashid centre for Diabetes- UAE. The intra-assay and inter- assay coefficients of variation were 8.3% and 3.2%, respectively. Participants with a serum 25(OH)D concentration less than 30 nmol/L (12 ng/mL) were considered to have deficiency; between 30 and 50 nmol/L as vitamin D of inadequate status and those with serum results over 50 nmol to be of adequate status [16]. All blood samples were taken in the early morning between 8 and 11 AM.
The date of recruitment was used to identify the season in which the blood sample was taken. The summer comprises the months of May to September and winter comprises the months of October to March. Even during the winter the average daytime temperature is 25°C (77°F). June to September is the hottest period of the year and it is expected that the inhabitants would avoid outdoor activities as temperatures could peak Page 5_ of _22 to 44°C (111.2°F). Therefore, for the purposes of analysis the seasons were classified into two groups: winter (from October to March) and summer (from April and August).
Due to time and resource restraints, 266 (26%) of the women were chosen randomly and followed up with either a phone call or questionnaire. The questionnaire was developed to obtain relevant information related to age (in years), Nationality (Emirate, Arabic, African, Asian, American, British or other), education level of the mother and the father, employment status, religion (Muslim, Christian, Hindu, Buddhist or other), marital status (married or divorced), whether this was the first pregnancy (primipara: yes/no), intake of dietary supplements including vitamin D, physical activity, lifestyle, and sun exposure. Sun exposure was measured by asking the participants about their outside habitual routines. The questionnaire asked participants if they exercised outside, do the participants ever walk outside and if so, how many hours do they spend walking outside during the day. Gestational age was estimated via ultrasound performed typically around the 18-20 weeks. If this data was not available, the gestational age was calculated based on the reported date of the last menstrual period.
The UAE is located at 24.4667°N, 54.3667°E and most days during the year are sunny, this could potentially either increase the production of 25(OH)D synthesized in the body or force more people indoors to avoid such an intense heat. Understanding the participant’s outside regime is vital if a possible intervention strategy is going to be developed.
Statistical Analysis
The characteristics of the sample were described using means and confident intervals (95%) for continuous and normally distributed variables. Categorical variables were presented as absolute (n) and relative frequencies (%). ANOVA analysis compared the 25(OH)D serums between groups and for significance.
All available covariates/predictors that could influence serum 25(OH)D concentrations according to the previous literature were explored, such as: education, age, gestational age, religion, nationality, primipara and participation in physical activity.
These predictors were considered to be included in the model when they were associated with the dependent variables (serum 25(OH)D concentrations) in the bivariate analysis if found significant (p ≤ 0.2).
Results
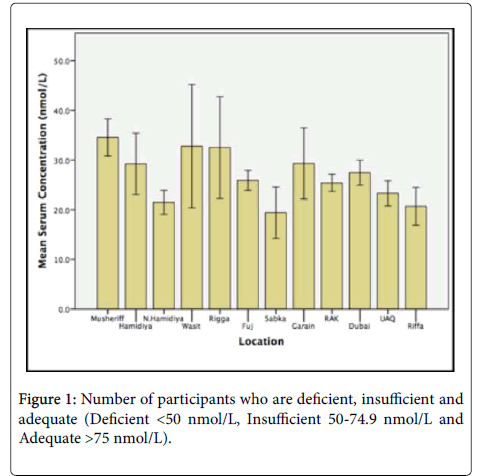
A total of 1088 women were recruited from 12 districts within the UAE. The majority of women (n=754; 69%) had vitamin D deficiency (<30 nmol/L), while a small minority (n=246; 22.6%) had vitamin D of insufficiency status (30-50 nmol/L), with 88 (8%) subjects with vitamin D status of adequate status (>50 nmol/L) (Figure 1).
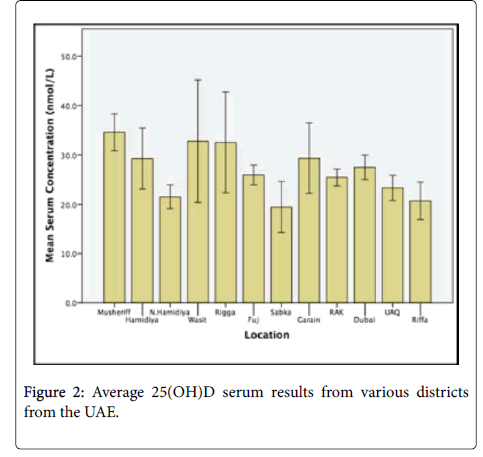
The average serum concentration for the whole cohort was 26.2 nmol/l (95% CI: 25.6-27.0 nmol/L). Out of the 12 districts included in the study, women from Subka had the lowest serum 25(OH)D concentration with an average of 19.4 nmol/L (95% CI: 15.1-23.9 nmol/L). Women from the district of Musheriff was found to have the highest serum 25(OH)D concentration with 34.6 nmol/L (95% CI: 31.1-38.2 nmol/L) (Figure 2).
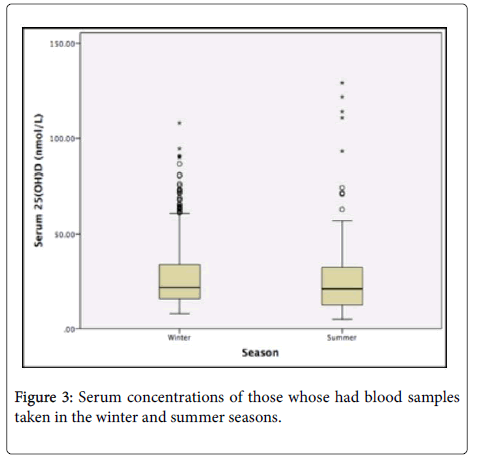
936 (86%) of the blood samples were obtained in the winter months while the rest were obtained in the summer months (n=152 14%).Figure 3 shows box plots comparing summer sample withdrawals to winter sample withdrawals. There was no significance between samples taken in the winter months (26.2 nmol/L) compared to samples obtained in the summer (26.2 nmol/L) both visually (Figure 3) and statistically (p=0.991).
The general characteristics of the sub sample (n=266) study population is presented in Table 1. The mean serum concentration was higher than the overall cohort (27.1 nmol/l 95% CI; 25.5-38.9 nmol/L) however this was not significant (p>0.05).
| Characteristics | Count (n) | Mean (nmol/L) | Lower CI (nmol/L)95% (nmol/L) | Upper CI 95%(nmol/L) (nmol/L) | Significance (p<0.05) |
|---|---|---|---|---|---|
| Average 25(OH)D serum | 266 | 27.1 | 25.5 | 38.9 | |
| Age (years) | 0.512** | ||||
| 14-35 | 181 | 26.8 | 24.7 | 28.9 | |
| 36-55 | 81 | 2 | 25.3 | 31.3 | |
| Did not answer | 4 | - | - | - | |
| Gestation | 0.93*** | ||||
| 1st Trimester (1-14 weeks) | 52 | 27.8 | 23.7 | 32.2 | |
| 2nd Trimester (15-28 weeks) | 174 | 26.9 | 24.9 | 28.9 | |
| 3rd Trimester (29+ weeks) | 40 | 26.9 | 22.5 | 32.2 | |
| Primipara | 0.390** | ||||
| Yes | 68 | 25.2 | 22.9 | 29.2 | |
| No | 198 | 27.5 | 25.4 | 29.5 | |
| Marital Status | * | ||||
| Married | 263 | 27.2 | 25.4 | 29 | |
| Divorced | 1 | - | - | - | |
| Did not answer | 2 | - | - | - | |
| Nationality | 0.401*** | ||||
| Emirate | 118 | 26.7 | 23.9 | 29.3 | |
| Arabic | 60 | 25.2 | 21.6 | 28.8 | |
| Asian | 60 | 30.4 | 26.9 | 34.3 | |
| African | 6 | 22.4 | 18 | 27.4 | |
| Other Gulf States | 3 | 29.8 | 22.1 | 44 | |
| Other | 16 | 27.9 | 25.4 | 29 | |
| Did not answer | 3 | - | - | - | |
| Education | 0.868*** | ||||
| Illiterate | 8 | 30.8 | 20.4 | 42.1 | |
| Primary | 9 | 28.2 | 23.1 | 34.4 | |
| Intermediate | 19 | 23.7 | 18.8 | 28.6 | |
| Secondary | 100 | 27.1 | 24.4 | 29.7 | |
| University | 119 | 27.5 | 24.8 | 30.2 | |
| Post Grad | 11 | 25.8 | 19 | 33.3 | |
| Occupation | |||||
| Housewife | 188 | 27.3 | 25.5 | 29.2 | |
| Employee | 60 | 26 | 22.9 | 30 | |
| Business Owner | 6 | 18 | 13.5 | 23.3 | |
| Quit work for | 6 | 42.2 | 28.3 | 54.7 | |
| more than a year | |||||
| Quit work less | 5 | 27.5 | 16.9 | 41.4 | |
| than one year | |||||
| Did not answer | 3 | - | - | - | |
| Religion | 0.514*** | ||||
| Muslim | 249 | 27.1 | 25.2 | 29 | |
| Christian | 6 | 31.8 | 13.5 | 48.4 | |
| Hindu | 7 | 24.1 | 14.4 | 34.9 | |
| Buddhist | 1 | 47.1 | 47.1 | 47.1 | |
| Other | 1 | 18.7 | 18.7 | 18.7 | |
| Did not answer | 2 | - | - | - | |
| Do you take a | 0.273** | ||||
| vitamin D | |||||
| supplement | |||||
| 5ug | 32 | 24.5 | 20.4 | 28.9 | |
| 10ug | 9 | 19.9 | 13.3 | 29.1 | |
| 15ug | 7 | 24.3 | 11.7 | 44.2 | |
| 20ug | 12 | 18.7 | 14 | 24.7 | |
| No supplement | 206 | - | - | - | |
| taken | |||||
| Participants own | 0.014** | ||||
| understanding on | |||||
| the importance of | |||||
| vitamin D | |||||
| Yes | 154 | 28.3 | 25.8 | 30.7 | |
| No | 43 | 22.1 | 19 | 25.4 | |
| Did not answer | 69 | - | - | - | |
| Exercising | 0.670** | ||||
| Outside | |||||
| Yes | 31 | 26.1 | 22.6 | 29.9 | |
| No | 55 | 29.1 | 24 | 36.6 | |
| Did not answer | 180 | - | - | - | |
| Do you do any physical activity | 0.234** | ||||
| Yes | 77 | 25.2 | 22.6 | 27.9 | |
| No | 161 | 27.6 | 25.3 | 30 | |
| Did not answer | 28 | - | - | - | |
Table 1: Characteristics of sub-sample group showing mean 25(OH)D.
The mean age of the participants was 28 (± 5.5) years old and ranged from 14 to 55 years. Gestational age at the time of testing was 18 (± 8) weeks, ranging from 1 to 37 weeks. The Majority of the participants (49%) were educated to a university level and married (99.5%). In Total, 196 of the women (74%) in the study did not work at the time of testing, and the remaining participants were employed (n=72; 26%). A majority of the participants consisted of three main nationalities: Emirati (44%), Arabic (23%) and Asian (23%).
There was no significance in 25(OH)D concentration between participants who were primipara (25.2 nmol/L) and those participants who were multipara (27.4 nmol/L) (p=0.390). Ethnicity had a small effect on the 25(OH)D concentration. People of African ethnicity had the lowest 25(OH)D concentrations, with 22.4 nmol/L (95% CI; 18.0-27.4), Arabic women with 25.2 nmol/L (95% CI; 21.6-28.8) and people of Asian ethnicity had higher than average 25(OH)D with 30.4 nmol/L (95% CI; 26.9-34.3) (Table 1). ANOVA analysis showed that nationality did not affect 25(OH)D status (p=0.401). The duration of pregnancy was characterised into trimesters to determine if 25(OH)D status varied from trimester to trimester. However, duration of gestation did not show a significant effect on a participant’s 25(OH)D status (p=0.93) (Table 1). There was no significant difference between those who were taking a vitamin D supplement and those who did not take a vitamin D supplement (p=0.73).
Out of the 266 participants, only 29 (11.6%) both understood the importance of vitamin D and took a vitamin D supplement compared to those who solely understood the importance of vitamin D (n=154). There was no significance between those who did and did not exercise outside; 26.1 and 29.6 nmol/l, respectively.
The following variables were individually tested as potential predictors into the simple linear regression model (bivariate analyses): maternal age (years), gestational duration (trimester), nationality (Emiratee vs. non Emiratee), employment (employed vs. unemployed), Exercising outside (yes/no), primipara (yes/no, physical activity during pregnancy (yes/no), if the subject understood the importance of vitamin D (yes/no) and supplement intake of vitamin D (yes/no). Table 2 shows the results of the bivariate analysis. No category was found to have significance higher the P=0.2 and therefore no stepwise linear regression could be made.
| Pearson Correlation | 2-tail Significance (=0.05) | |
|---|---|---|
| Age (years) | 0.17 | 0.257 |
| Gestation (weeks) | 0.039 | 0.526 |
| Primipara | 0.053 | 0.39 |
| Marital Status* | ||
| Nationality (Emirateevs.Non-Emiratee) | 0.034 | 0.582 |
| Education (Those who went to university vs.those who did not go to university) | -0.19 | 0.757 |
| Religion (Muslim and those who are not Muslim) | -0.48 | 0.438 |
| Understanding of vitamin D | -0.174 | 0.014 |
| Participation in physical activity | 0.077 | 0.234 |
| Occupation (Housewives compared to working mothers) | -0.71 | 0.252 |
| Does the participant take a Vitamin D supplement. | -0.67 | 0.275 |
| Do you do any physical activity | 0.038 | 0.534 |
Table 2: Results of the bivariate analyse on sub sample group.
Discussion
Vitamin D deficiency is a public health problem within the UAE as highlighted by the 69% of the women who had serum 25(OH)D results lower than 30 nmol/L where the recommended level should be between 50-125 nmol/L. It was observed that there was no seasonal variation in the prevalence of vitamin D deficiency and the mean concentrations did not vary according to gestation age with similar concentrations recorded during 1st, 2nd and 3rd trimesters.
Some of the results were inconsistent with the literature [21-24]. Depending on the season, 25(OH)D has shown to vary in individuals. It may have been theorised that subjects would have adequate levels of 25(OH)D (50 nmol/L or 30 ng/L) as they live close to the equator and the sun shines for long periods, even during the winter months [25]. However, this is not seen in the present study. A factor that may have influenced women's 25(OH)D levels may be the culture within the Gulf States and their religious beliefs regarding the covering of their head and body, but also the hot environment throughout the year. Arab women located in the United States that did not follow religious procedures of head and body covering, and therefore exposed themselves to UV-B light more frequently, were found to have mean 25(OH)D of 21.25 nmol/L [26]. Although the mean 25(OH)D value of Arab American women were lower than what was presented in the current study (26.2 nmol/L) it was higher than values presented in other studies in similar population ten years ago, (17.5 nmol/L). This rise in 25(OH)D may be due to the increase in knowledge of vitamin D and the use of vitamin D supplements [19]. The average Arab American women concentration of 25(OH)D may have been lower than the presented study as those samples were obtained in Michigan in the spring as 25(OH)D concentrations would be at the lowest [27]. Compared to the UAE, only three districts had lower 25(OH)D than the average Arab American woman; North Hamidiya (21.5+13.9 nmol/L), Riffa (20.7+14.1 nmol/l) and Sabka (19.4+6.7 nmol/L).
Sun exposure was not associated with vitamin D levels in this study. One of the potential explanations for these findings is that sun exposure was relatively low in this population. Another reason might be due to air pollution, as it reduces vitamin D production through UVB exposure and also prevents people from wanting to exercise outside. In a previous study involving pregnant women living in Iran, air pollution was inversely associated with 25(OH)D concentrations [28]. In UEA air pollution is high with particulate matter less than 10 μm in diameter (PM10) estimated to be 140 μg/m3 in 2014 [29] but has increased to an alarming 185 ug/m3 and some days reaches highs of 348 ug/m3 [30]. This value is above the World Health Organization recommendations (<20 μg/m3 annual average or 50 μg/m3 hourly average concentrations) [31].
Skin colour is also known to affect 25(OH)D status. Vitamin D concentrations are lower in those who have darker skin pigmentation, as the amount of UV-B light that can penetrate the epidermis is reduced, and the rate at which pre-vitamin D is synthesized is decreased [32]. Unfortunately, no comparisons can be made with the presented cohort as skin colour was not asked in the questionnaire.However, ethnicity was used as a proxy measure of skin colour. People of African ethnicity who would predominately have darker skin pigmentation over people of Asian ethnicity were shown to have lower 25(OH)D concentrations.
With regards to education, 49% of women were university graduates or students. There seems to be a common trend among educated women within the UAE having 25(OH)D deficiency. In an earlier study [33], women of higher education were found to have vitamin D serums of insufficient status during the winter months 31.3 ± 12.3 nmol/L. While in the summer, 25(OH)D fell to 20.9 ± 14.9 nmol/L. According to the authors the summer season and the commitments of university might have prevented outside activity and the exposure of skin to UV-B light [34,35]. These findings were very similar to the participants that were assessed in this study who were educated to a university degree (postgrad) had average serums of 25.8 nmol/L compared to 27.2 nmol/L of those without university degree. However, this was not significantly different (p=0.757).
In the present study, time of gestation did not affect serum 25(OH)D concentration. However, an Australian study, including 466 pregnant women, showed that 25(OH)D concentrations tend to gradually decrease from the 1st trimester (75.25+19.5 nmol/L) to the 3rd trimester (44.64+22.25 nmol/L) (p<0.0001) [36,37]. Women who started the study (1st trimester) in autumn/winter had lower serum results (52.75+13 nmol/L) compared to those who started the study in the spring/summer (72.25+7 nmol/L) [35]. In the 3rd trimester of pregnancy, serum 25(OH)D results dropped further, to 42.5+25 nmol/L (p<0.0001) of those who began their pregnancy in the autumn/ winter months [36].
No epidemiological study to date has investigated the 25(OH)D serums of pregnant women within the UAE during the course of a pregnancy.
Age was not significantly associate with 25(OH)D serum concentrations. The literature states that 25(OH)D of low concentrations are more prevalent in older women; however, this trend was not seen in this study as 69% of the study population was of deficient status and the average age was 28 (± 5.5) years.
In the studied population 92% (n=1000) had serum results <50 nmol/L. According to the National Institute of Health [37]. Individuals whose serum 25(OH)D were between 25-50 mol/L were at mild risk go hypovitaminosis, those whose were found to be between 12 and 25 nmol/l are at a moderate risk and those with less than 12 nmol/l are at a severe risk of hypovitaminosis D. In the current population 32.6%, 45.9% and 13.5% are at risk of mild, moderate and severe risk of hypovitaminosis D, respectively. Hypovitaminosis is associated with insulin resistance and beta cell dysfunction [38]. Maternal 25(OH)D serums lower than <40 nmol/L have shown to be associated with low birth-weight and short stature [39]. It is possible that blood serum concentrations of 25(OH)D below 40 nmol/L are associated with poor pregnancy outcomes [40].
The main strength of the current study was the big sample size involved 1088 women from various backgrounds and ages. Another strength is that the 25(OH)D concentrations were measured using liquid chromatography tandem mass spectrometry (LC-MS/MS) and competitive protein binding assay, which is the gold standard for measuring 25(OH)D [40] and the data was not cross sectioned in order not to infer causality. However, there were some limitations to this study. Due to the time and resource limitations, only 26.6% of participants were followed up with a demographic questionnaire.
Another limitation is that no height and weight was recorded from the participants, so BMI could not be calculated, this would have been advantageous to the study as there is evidence to suggest people with higher BMIs have lower vitamin D status [41]. Furthermore, participants could have introduced bias into their responses due to answering the questions on what they expected the interviewer to hear instead of answering truthfully [42]. There is data available on the dietary intake on Emirati women which will be used in future research and lay the foundations to future interventions with the aim to raise 25(OH)D concentrations.
To conclude, the prevalence of vitamin D deficiency in UAE is very high (69%) and average maternal serums was 27.1 nmol/L (5% CI: 25.5-38.9). The only factor that explained part of the variation in 25(OH)D concentration in this study was if the participant understood the importance of vitamin D (p<0.05). The findings from crosssectional study conducted in apparently healthy women from a sunny area highlight the importance of vitamin D sufficiency during pregnancy. Intervention strategies including supplementation, fortification and dietary diversity must be implemented to prevent the problem from escalating, targeting those who are vulnerable first and then exposed to a wider population.
Acknowledgement
This research was financed by Ministry of Health UAE and Iodine Global Network. The authors are grateful to the participants who contributed data to this study and they would like to thank the research team involved in collecting data from the participants. All data was collected by Dr Izzeldin Hussein and his team within the United Arab Emirates. Statically analysis and writing was conducted by Dr Tewfik and his team at the University of Westminster in London, England. Ethics was approved by the Corniche Hospital Research Ethics Committee, UAE.
References
- Palacios C, Gonzalez L (2014) Is vitamin D deficiency a major global public health problem? J Steroid Biochem Mol Biol 144: 138-145.
- Rivas M, Rojas E, Araya MC, Calaf GM (2015) Ultraviolet light exposure, skin cancer risk and vitamin D production.Oncol Lett 10: 2259-2264.
- (2010) International Federation of Human Rights. Women’s Rights in the United Arab Emirates. Internation federation of human rights.
- Tuchinda C, Srivannaboon S, Lim HW (2006) Photoprotection by window glass, automobile glass and sunglasses. J Am Acad Dermatol 54:845–854.
- Nair R, Maseeh A (2012) Vitamin D: The ‘sunshine’ vitamin. J Pharmacol Pharmacother 3: 118-126.
- ALNohair S (2014) Obesity in Gulf Countries. Int J Health Sci 8: 79-83.
- Martini LA, Wood RJ (2006) Vitamin D status and the metabolic syndrome. Nutr Rev 64: 479-486.
- Narchi H, Kochiyil J, Zayed R, Abdulrazzak W, Agarwal M, et al. (2010) Maternal vitamin D status throughout and after pregnancy. J Obstet Gynaecol 30: 137-142.
- Liu NQ, Kaplan AT, Lagishetty V, Ouyang YB, Ouyang Y, Simmons CF, etal. (2011) Vitamin D and the regulation of placental inflammation.J Immunol Baltim Md 186: 5968-5974.
- Wagner CL, Taylor SN, Dawodu A, Johnson DD, Hollis BW (2012) Vitamin D and its role during pregnancy in attaining optimal health of mother and fetus. Nutrients 4: 208-230.
- Ullah MI, Koch CA, Tamanna S, Rouf S, Shamsuddin L (2013) Vitamin D deficiency and the risk of preeclampsia and eclampsia in Bangladesh.Horm Metab Res Horm Stoffwech self or schung Horm Métabolisme 45: 682-687.
- Urrutia RP, Thorp JM (2012) Vitamin D in pregnancy: Current concepts. Curr Opin Obstet Gynecol 24: 57-64.
- (2014) Care pathways for the diagnosis and initial management of risk factors for cardiovascular disease. Health Authority Abu Dhabi.
- CIA (2016) The World Fact Book, United Arab Emerates.Central Intelligence Agency.
- Mahon P, Harvey N, Crozier S, Inskip H, Robinson S, et al. (2010) Low maternal vitamin D status and fetal bone development: Cohort study. J Bone Miner Res Off J Am Soc Bone Miner Res 25: 14-9.
- (2011) DRIs for calcium and Vitamin D. Institute of Medicine.
- Ashwell M, Stone EM, Stolte H, Cashman KD, Macdonald H, et al. (2010) UK food standards agency workshop report: An investigation of the relative contributions of diet and sunlight to vitamin D status. Br J Nutr 104: 603-11.
- Dawodu A, Agarwal M, Patel M (1997) Serum 25-hydroxyvitamin d and calcium homeostasis in the United Arab Emirates mothers and neonates: A preliminary report. Middle East Paediatr 29: 12.
- Dawodu A, Kochiyil J, Altaye N (2011) Pilot study of sunlight exposure and vitamin D status in Arab women of childbearing age. East mediterr health j rev santé méditerranée orient al-majallah al-á¹£iḥḥ�?«yah li-sharq al-mutawassiá¹ 17: 570-574.
- Dawodu A, Akinbi H (2013) Vitamin D nutrition in pregnancy: Current opinion. Int J Womens Health 5: 333-343.
- Baker MR, Peacock M, Nordin BE (1980) The decline in vitamin D status with age. Age ageing 9: 249-252.
- Sherman SS, Hollis BW, Tobin JD (1990) Vitamin D status and related parameters in a healthy population: The effects of age, sex and season. J Clin Endocrinol Metab 71: 405-413.
- Jonson D, Wagner C, Hulsey T, McNeil R, Ebeling M, et al. (2011) Vitamin D deficiency and insufficiency is common during pregnancy. Am J Perinatol 28: 7-12.
- Vieth R, Ladak Y, Walfish PG (2003) Age-related changes in the 25-hydroxyvitamin d versus parathyroid hormone relationship suggest a different reason why older adults require more vitamin D. J Clin Endocrinol Metab 88: 185-191.
- Zhang RH, He DH, Zhou B, Zhu YB, Zhao D, et al. (2015) Analysis of vitaminD status in men highly exposed to sunlight. Biomed Environ Sci BES 28: 913-916.
- Hobbs RD, Habib Z, Alromaihi D, Idi L, Parikh N, et al. (2009) Severe vitamin D deficiency in Arab-American women living in Dearborn, Michigan. EndocrPract Off J Am Coll Endocrinol Am Assoc Clin Endocrinol 15: 35-40.
- Nesby-O’Dell S, Scanlon KS, Cogswell ME, Gillespie C, Hollis BW,et al. (2002) Hypovitaminosis D prevalence and determinants among African Americanand white women of reproductive age: Third national health and nutrition examination survey1988-1994.Am J Clin Nutr 76: 187-192.
- Kelishadi R, Sharifi-Ghazvini F, Poursafa P, Mehrabian F, Farajian S, Yousefy H, et al. (2013) Determinants of hypovitaminosisD in pregnant women and their new-borns in a sunny region. Int J Endocrinol.
- World Health Organization (2016) WHO’s Urban Ambient Air Pollution database.
- (2016) Air Quality Index.
- World Health Organization (2005) Air Quality Guidlines WHO.
- Sawicki CM, Van Rompay MI, Au LE, Gordon CM, Sacheck JM, et al. (2016) Sun-exposed skin color is associated with changes in serum 25-hydroxyvitamin d in racially/ethnically diverse children. J Nutr 146: 751-757.
- Al Anouti F, Thomas J, Abdel-Wareth L, Rajah J, Grant WB, et al. (2011) Vitamin D deficiency and sun avoidance among university students at Abu Dhabi, United Arab Emirates.Dermatoendocrinol 3: 235-239.
- Faghih S, Abdolahzadeh M, Mohammadi M, Hasanzadeh J (2014) Prevalence of vitamin d deficiency and its related factors among university students in Shiraz,Iran. Int J Prev Med.5:796-799.
- Fernández-Alonso AM, Dionis-Sánchez EC, Chedraui P, González-Salmerón MD, Pérez-López FR (2012) Spanish Vitamin D and Women’s Health Research Group. First-trimester maternal serum 25-hydroxyvitamin Dâ�?�? status and pregnancy outcome. Int J Gynaecol Obstet Off Organ Int Fed Gynaecol Obstet 116: 6-9.
- Bodnar LM, Catov JM, Zmuda JM, Cooper ME, Parrott MS, et al. (2010) Maternal serum 25-hydroxyvitamin D concentrations are associated with small-for- gestational age births in white women.J Nutr 140: 999-1006.
- National Institute of Health - Vitamin D.
- Chiu KC, Chu A, Go VLW, Saad MF (2004) Hypovitaminosis D is associated with insulin resistance and β cell dysfunction. Am J Clin Nutr 79: 820-825.
- Litonjua AA (2009) Childhood asthma may be a consequence of vitamin D deficiency. Curr Opin Allergy Clin Immunol 9: 202-207.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, Gordon CM, Hanley DA, et al. (2011) Evaluation, treatment and prevention of vitamin D deficiency: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96: 1911-1930.
- Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF (2000) Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr 72: 690-693.
- Thea M (2016) Faking it: Social desirability response bias in self-report research. Aust J AdvNurs. 25: 40-48.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 12778
- [From(publication date):
October-2016 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 11791
- PDF downloads : 987