Role of Pediatric Airway Expert and Videolaryngoscope in Perioperative Airway Management of an Anticipated Difficult Pediatric Airway - We Fail, We Learn, We Evolve
Received: 24-Jan-2022 / Manuscript No. nnp-22-52275 / Editor assigned: 27-Jan-2022 / PreQC No. nnp-22-52275(PQ) / Reviewed: 11-Feb-2022 / QC No. nnp-22- 52275 / Revised: 15-Feb-2022 / Manuscript No. nnp-22-52275(R) / Accepted Date: 22-Feb-2022 / Published Date: 22-Feb-2022 DOI: 10.4172/2572-4983.1000225
Abstract
The difficult airway associated with Pierre Robin Sequence (PRS) is a known challenge for anaesthesiologists. These challenges increase manifold in redo surgeries. A 44 days old infant with PRS underwent glossopexy, the airway was secured using videolaryngoscope and external laryngeal manipulation. When the child was extubated in the Pediatric intensive care unit on the third postop day, the sutures from primary surgery got loosened causing the tongue to fall and obstruct the airway. The child was posted for the same surgery in a short time because of eventful extubation offering us an even more challenging airway. We are reporting the perioperative role of a pediatric airway expert in this case of anticipated airway difficulty.
Conclusion: We suggest that the day-to-day practice can be altered and improved based on bad past experiences. A multidisciplinary approach including a pediatric airway expert and a videolaryngoscope can be a game-changer in case of extubation of a difficult airway patient.
We emphasize the presence of a pediatric airway expert and videolaryngoscope in the pediatric/neonatal intensive care unit during the management of the anticipated pediatric difficult airway.
Keywords: cleft, videolaryngoscope, multidisciplinary
Introduction
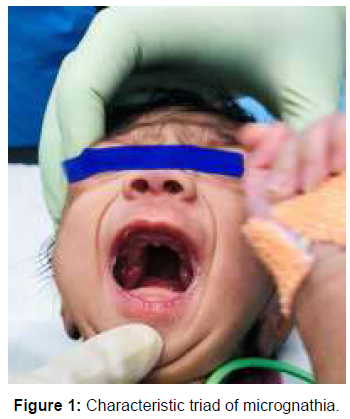
Pierre Robin Sequence (PRS) occurring in 1 in 8,500 to 14,000 births, is characterized by the classic triad of micrognathia, glossoptosis and cleft palate [1]. This congenital syndrome is associated with upper airway obstruction and feeding difficulties. The incidence of difficult intubation in pediatric patients with syndromes like PRS or facial anomalies is 0.18% [2]. In children with PRS, airway management is always a challenge even for an experienced anaesthesiologist and these challenges multiply manifold with redo surgeries. We report the successful use of videolaryngoscope in perioperative airway management of an infant with PRS undergoing redo-glossopexy along with a multidisciplinary team approach.
Case Report
A 44-day old boy weighing 2270 gm, was born at 37 gestational week by normal vaginal delivery. He was diagnosed to have Pierre Robin sequence (PRS) and posted for glossopexy (adhesion of tongue with lower lip). The child had a characteristic triad of PRS which is micrognathia, glossptosis and cleft palate (Figure 1 and 2). He also had a tracheal tug with substernal retractions. Screening two-dimensional echocardiography and investigations were normal. The child was posted for glossopexy under general anaesthesia. The airway was secured with a micro-cuff Endo Tracheal Tube (ETT) size 3.0 mm, using a C-MAC videolaryngoscope the percentage of glottic opening (POGO) of 0% was seen. With the help of a bougie and external laryngeal manipulation, the child was intubated in the first attempt. Post-surgery, considering airway oedema, the child was shifted to the Pediatric Intensive Care Unit (PICU). After a short course of steroids, he was extubated on a third postop day by a PICU resident on duty. While extubating the sutures placed for glossopexy got loosened and the tongue fell back causing airway obstruction. A decision was taken to post the child for redo-glossopexy as an emergency. Meanwhile, the child was monitored in PICU and his head was kept extended and tilted to one side.
Problems faced during the second time were- dependent oedema on the face, oxygen saturation (SpO2)-95% on nasal prongs, edematous tongue falling in the airway requiring nasopharyngeal airway for mask ventilation, on laryngoscopy with C-MAC blade 2- oedema around the inter arytenoid notch made it impossible to introduce ETT or bougie. On the 3rd attempt, a bougie guided intubation was done with size 3.0 micro-cuff ETT intubation was possible using C-MAC videolaryngoscope blade size 2 with external laryngeal manipulation by the senior anesthesiologist. The desaturation (SpO2-85-80%) with each attempt was managed with BMV using 100% oxygen. Postoperatively, the child was shifted to PICU, intubated.
For postoperative management, we formed a multidisciplinary team that included anesthesiologists, surgeons and paediatricians. This team followed up with the child and on the third postop day, the decision was taken to extubate the child in presence of the whole team. We kept all the difficult airway equipment and C-MAC videolaryngoscope handy. Moreover, the extubation was done carefully under C-MAC guidance without any complications. The child remained stable hemodynamically with SpO2-96-97% on room air.
Discussion
In PRS the presence of micrognathia, glossoptosis and cleft palate can cause airway obstruction leading to acute respiratory distress which can be life-threatening if not managed timely [1]. In a few patients, such airway obstruction can be managed conservatively by nonsurgical methods like prone positioning, nasopharyngeal airway, and placement of laryngeal mask airway or endotracheal intubation. Some children require surgical interventions like glossopexy, mandibular distraction osteogenesis or tracheostomy. Both non-surgical or surgical management of upper airway obstruction in an infant with PRS may require endotracheal intubation, which is always a challenge for the anesthesiologist. General anaesthesia can exacerbate the upper airway obstruction making airway management even more challenging and so the literature recommends awake intubation before induction of anaesthesia [3]. In our case, mask ventilation was confirmed under sevoflurane, keeping the spontaneous respiration.
Although fiberoptic intubation is considered the gold standard for the management of anticipated difficult airways, its use has several limitations, especially in neonates and infants. Availability, the requirement of significant experience and skill, time-consuming procedure and difficulty in advancing the ETT over scope are some of the limitations of the neonate fiberoptic bronchoscope. Short apnea tolerance and increased risk of airway oedema make it more challenging to use a bronchoscope in neonates and infants [4, 5]. Videolaryngoscope plays an important role in paediatrics difficult airway management, which enables the anesthesiologists to visualize the glottis and vocal cords without alignment of the various axes. An emergency redo-surgery offers even more challenges in cases of infants with PRS because of the airway oedema, which was distinctly seen in our case. In case of a difficult airway, extubation is as challenging as intubation and vigilant extubation can avoid the complications associated with reintubation or sometimes, redo surgery. The airway expertise should be present at the bedside or its immediate accessibility should be verified before extubations in this group of patients. The necessary equipment for managing pediatrics difficult airways should be readily available [6]. In our case, the first extubation was done in PICU by paediatricians. It resulted in the loosening of sutures and eventually required redo surgery. The airway difficulty was escalated due to existing airway oedema.
We constantly learn from our mistakes and experiences. Lessons were learnt from this experience and a multidisciplinary team approach involving paediatricians, anesthesiologists and surgeons, was used for extubation after redo surgery. Keeping all necessary equipment to manage a difficult airway, the child was gently extubated under C-MAC guidance to avoid trauma to the surgical site.
We suggest that the day-to-day practice can be altered and improved based on bad past experiences. A multidisciplinary approach including a pediatric airway expert and a videolaryngoscope can be a gamechanger in case of extubation of a difficult airway patient. We emphasize the presence of a pediatric airway expert and videolaryngoscope in the pediatric/neonatal intensive care unit during the management of the anticipated pediatric difficult airway.
References
- Jakobsen LP, Knudsen MA, Lespinasse J, Ayuso CG, Ramos C, et al. (2006) The genetic basis of the Pierre Robin Sequence. Cleft Palate Craniofac J 43: 155-159.
- Dobby N, Black A, Ong KB (2012) Airtraq vs Glidescope airway management of a pediatric population with a documented difficult airway; Cormack and Lehane Grade III or IV. Pediatr Anesth 22: 921.
- Asai T, Nagata A, Shingu K (2008) Awake tracheal intubation through the laryngeal mask in neonates with upper airway obstruction. Paediatr Anaesth 18: 77-80.
- Asai T, Shingu K (2004) Difficulty in advancing a tracheal tube over a fibreoptic bronchoscope: incidence, causes and solutions. Br J Anaesth 92: 870-881.
- Parotto M, Cooper RM, Behringer EC (2020) Extubation of the Challenging or Difficult Airway. Curr Anesthesiol Rep 4: 1-7.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Rathod D, Kumari K, Rao JK, Meshram T, Goyal S (2022) Role of Pediatric Airway Expert and Videolaryngoscope in Perioperative Airway Management of an Anticipated Difficult Pediatric Airway - We Fail, We Learn, We Evolve. Neonat Pediatr Med 8: 225. DOI: 10.4172/2572-4983.1000225
Copyright: © 2022 Rathod D. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2822
- [From(publication date): 0-2022 - Dec 23, 2025]
- Breakdown by view type
- HTML page views: 2200
- PDF downloads: 622