Review Article Open Access
Role of the Medial Gastrocnemius Muscle Flap in Soft Tissue Defect Reconstruction of the Leg in Children: About Two Cases
François-Fiquet C, Binet A*, Swennen C, Ludot H, Belouadah M, Poli-Merol ML and Bourelle S
Pediatric Surgery Department, American Memorial Hospital, 43, Rue Cognacq Jay, 51092 REIMS, France
- *Corresponding Author:
- Binet A
Pediatric Surgery Department, American Memorial Hospital
43, Rue Cognacq Jay, 51092 REIMS, France
Tel: 06-32-73-08-22
Fax: 03 26 78 43 18
E-mail: aurelien.binet1@gmail.com
Received Date: November 25, 2015 Accepted Date: December 03, 2015 Published Date: December 11, 2015
Citation: François-Fiquet C, Binet A, Swennen C, Ludot H, Belouadah M, et al. (2015) Role of the Medial Gastrocnemius Muscle Flap in Soft Tissue Defect Reconstruction of the Leg in Children: About Two Cases. J Child Adolesc Behav 3:261. doi:10.4172/2375-4494.1000261
Copyright: © 2015 François-Fiquet et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
Use of medial gastrocnemius flap is part of the therapeutic array in soft tissue defect reconstruction for the upperthird part of the leg in adults. Indications for this type of flap remain quite rare in children. We will report our experience through two clinical cases and discuss the role of this type of flap in the treatment of soft tissue defect in children.
Keywords
Flap; Gastrocnemius; Medial gastrocnemius; Soft tissue defect; Pediatric plastic surgery
Cases
A 10-year-old boy suffered soft tissue defect following a crush injury on his left leg with compound and Type 3B open fracture (Gustillo classification) of the upper extremity of the tibia, which had not healed 1 month after the accident. A 14-year-old girl presented with soft tissue defect secondary to surgical resection of an osteosarcoma of the diaphysis of the tibia using the one-step Masquelet technique. For these two patients, we used a medial gastrocnemius muscle flap with upper pedicle for thin skin graft reconstruction (one-stage surgery, graft harvested from the opposite limb) in order to cover the soft tissue defect on the anterior side of the upper third part of the leg. In both cases this simple technique completely covered the soft tissue defect, furthermore the healing was quick and cosmetic and functional outcomes at 18 months post-surgery were very good. In children, plastic surgery is very conservative promoting simple management techniques; however, teams should be aware of the medial gastrocnemius flap in order to propose it without delay in specific indications of traumatic or malignant soft tissue defects (open fracture, material exposure) of the upper third part of the leg.
Introduction
This medial gastrocnemius flap technique was first published in the seventies [1]. This muscle flap with proximal pedicle is characterized by its reliability, sturdiness and lack of functional impairments. Surgical indications are well standardized [2,3].
Soft tissue defect cover of the upper third part of the leg, anterior or medial side of the knee
Filling a deep anatomic defect
Bone (fracture) or osteosynthesis cover
Even if this muscle flap is an integrant part of the therapeutic array for soft tissue reconstruction in adults its indication is quite confidential in children. In fact with pediatric plastic surgery treatments are as conservative as possible due to the specific nature of children with increased wound-healing capacities and skin laxity. However, for specific indications this muscle flap can be proposed in pediatric cases. We report our experience through two clinical cases.
Case 1
A 10-year-old boy, victim of a traffic accident, presented with soft tissue defect following a crush injury on the upper third of his left right leg with a compound open fracture (Gustillo Type 3B) of the upper extremity of the tibia and proximal dislocation of the fibula.
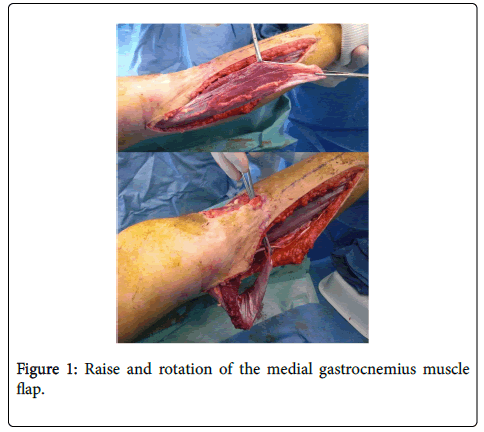
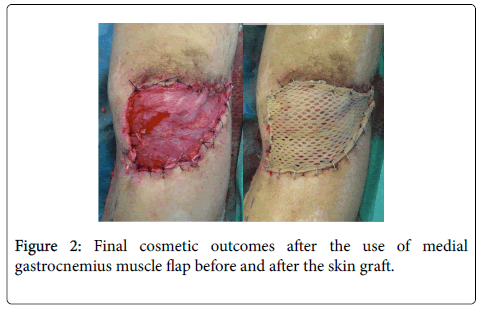
Fracture reduction and stabilization (external fixation) stopped the ischemia. There were no vascular lesions. Necrosis set in quickly on the bruised skin. After necrosectomy, a soft skin defect (10 cm in diameter) remained on the anterior side of the tibia with partial exposure of the fracture site. VAC® therapy was implemented. In the absence of appropriate bone cover, the use of medial gastrocnemius flap was indicated. The technique was the same as the one used in adults (Figures 1 and 2). One year post surgery cosmetic outcomes were excellent. However, bone consolidation was not achieved and the child underwent bone graft and osteosynthesis.
Case 2
A 14-year-old girl presented with high-grade malignant osteoblastic osteosarcoma of the upper third part of the tibial diaphysis. Following neoadjuvant chemotherapy, complete resection of the tumor was performed at the same time as the first step of the Masquelet technique [4,5]. After resection and osteosynthesis material implantation a soft tissue skin defect remained (10 cm in diameter) on the anterior side of the proximal part of the leg. According to the need for fast wound healing (postoperative chemotherapy), the use of medial gastrocnemius muscle flap was indicated. At one year post surgery, this patient was in remission from the osteosarcoma. She underwent the second step of the Masquelet technique with an allograft. She started walking again with no difficulties. Cosmetic outcomes were good for the donor and receiver sites and the patient expressed her satisfaction (Figure 3).
Discussion
Ger and Efron were the first to publish the management of soft tissue defect of the knee by use of medial gastrocnemius muscle flap [1]. Since this flap is easily harvested and can be rotated [6] it has become the technique of choice for covering soft tissue defect of the anterior and medium side of the knee as well as the upper third part of the leg [2]. Commonly seen in adults, its use remains confidential in children. Pediatric plastic surgery requires proper knowledge of healing specificities according to the child’s age and consequences on growth and development. Rapid wound healing and potential skin retractions make wound management more complicated in children. Skin laxity permits the use of one-step wound closure techniques. In spite of all the above, and in cases of soft tissue defect of the leg in children the use of medial gastrocnemius muscle flap can be the right indication for skin defect with open fracture or material exposure. In fact, in case of fractures, this option should be implemented very quickly to limit the risks of infections and non-unions. For reconstruction after tumor resection, the use of this flap has been described in adults [7]. Its indications can be extended to adolescents. In fact, this technique can promote a rapid and proper cover of the defect on surgical areas needing to heal quickly without further defects (postoperative chemotherapy).
Conclusion
The use of medial gastrocnemius muscle flap in children remains confidential. However, this flap is relevant in pediatric plastic surgery and should be recognized and use without delays in specific indications such as traumatic skin tissue defects (open fractures or material exposure) and tumor-related defects on the upper third part of the anterior side of the leg.
References
- Ger R, Efron G (1970) New operative approach in the treatment of chronic osteomyelitis of the tibial diaphysis. A preliminary report. ClinOrthopRelat Res 70: 165-169.
- Masquelet AC (2008) Reconstruction des pertes de substance osseusediaphysairesd’originetraumatique. Stratégies, recommandations, perspectives. Revue de ChirurgieOrthopédique et Traumatologique 98: 94–103.
- Masquelet AC, Gilbert A (2005) Flaps in Limb Reconstruction. Martin Dunitzedn.
- Biau DJ, Pannier S, Masquelet AC, Glorion C (2009) Case report: reconstruction of a 16cm diaphyseal defect after Ewing's resection in a child. ClinOrthopRelat Res 467: 572-577.
- Masquelet AC (2000) Reconstruction of the long bones by the induced membrane and spongy autograft. Ann ChirPlastEsthet 45:346-53.
- Dibbell DG, Edstrom LE (1980) The gastrocnemius myocutaneous flap. ClinPlastSurg 7: 45-50.
- Buchner M, Zeifang F, Bernd L (2003) Medial gastrocnemius muscle flap in limb-sparing surgery of mali gnant bone tumors of the proximal tibia: mid-term results in 25 patients. Ann PlastSurg 51: 266-272.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 14227
- [From(publication date):
December-2015 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 13072
- PDF downloads : 1155