Roux en Y Gastric Bypass after Failed Primary Restrictive Procedures in Morbidly Obese Patients
Received: 01-Sep-2020 / Accepted Date: 07-Oct-2020 / Published Date: 14-Oct-2020 DOI: 10.4172/2165-7904.1000410
Abstract
Background: Worldwide prevalent over the past several decades, Obesity morbidities and health related adverse effects has been an increasing concern that lead to revolutionary advancements in the field of bariatric surgery. The long-term outcomes of the different techniques in have gained popularity in the last years. Although sleeve gastrectomy is being performed with increasing frequency as well as other restrictive procedures, failure or inadequate satisfactory outcome of these procedures became interestingly evident and thoroughly studied ranging from regaining of the preliminary lost weight, insufficient weight loss, GERD, and various other complications all of which determine a failure of the primary procedure.
Methods: In this prospective study 40 patients were included who underwent a revisional Roux-en-Y gastric bypass after failure of a different primary restrictive procedures (17 patients underwent sleeve gastrectomy, 21 patients underwent VBG and 2 patients underwent adjustable gastric banding) from January 2018 till January 2019 with a follow up period of one year till January 2020.
Results: Each patient had different indication for the revisional Roux en y gastric bypass conversion: 18 patients (45%) due to weight regain after 1ry weight loss, 14 patients (35%) due to insufficient weight loss, and 8 patients (20%) due to GERD. Roux en y gastric bypass was performed with significant reduction of both mean weight of the patients from 113.50 ± 9.92 kg to 98.65 ± 9.93 and 89.18 ± 9.84 after 6, and 12 months respectively and mean BMI from 39.06 ± 4.91 before the conversion to 33.93 ± 4.44 and 30.65 ± 4.11 at 6 and 12 months respectively. Moreover, co-morbidities such as Diabetes and Hypertension were markedly improved in addition to the lipid profile of most of the patients.
Conclusion: Roux en y gastric bypass is a safe surgical procedure with satisfactory outcomes and can be proposed as first line management choice to revise failed primary restrictive bariatric procedures.
Keywords: Laparoscopic sleeve gastrectomy; Roux-en-Y gastric bypass; Restrictive procedures; VBG; Adjustable gastric banding; Treatment failure; Revisional surgery
Introduction
Morbid obesity poses one of the major public health concerns in the world today [1-3]. National Center for Health Statistics (NCHS) reported an increase in obesity prevalence from 4.7% to 9.2% from the period between (2000 – 2018) (CDC, 2020). The National Institute of Health (NIH) proposed the following criteria to classify an individual as morbidly obese:
• >100 pounds above ideal body weight,
• Body Mass Index (BMI) > 40 kg/m2
• BMI > 35 kg/m2 and one or more co-morbid conditions.
Bariatric surgeries are commonly recognized interventions in achieving long term weight loss [4]. Some of the most widely used bariatric surgical techniques are Roux-en-Y Gastric, Sleeve Gastrectomy, Adjustable Gastric Band and Biliopancreatic Diversion with Duodenal Switch (BPD/DS) [5]. Long term treatment failure has been reported. Failure determinants can be regaining the lost weight, inadequate weight loss, GERD and other metabolic & nutritional complications can occur, requiring a revisional surgery that can address these determinants and securing a satisfactory outcome [6].
Revision of the primary restrictive approach by another to correct it has not been that immensely reported. Leaving the question of which operation is superior to the other in terms of correcting the failed primary procedure.
Methods
This prospective study included 40 patients who underwent a revision bariatric surgery in the form of Roux-en-y gastric bypass after failure of different bariatric restrictive procedures (17 patients underwent sleeve gastrectomy, 21 patients underwent VBG and 2 patients underwent adjustable gastric banding) at Ain Shams University Hospital in the period from January 2018 till January 2019 with a follow up period up to one year till January 2020.
Data collection & Selection of patients
Inclusion criteria
Patients with weight regain, failure of weight loss or development of complications following the primary restrictive procedure between es of 18 to 60 years old, with a body mass index of 35 or more.
Exclusion criteria
Patients younger than 18 or older than 60 years old, unfit for general anesthesia, refuse to share in the study, unable to participate in prolonged follow up and who have history of psychiatric illness, drug or alcohol addiction, severe debilitating diseases, nutritional deficiency or advanced malignancy were all excluded from the study.
Data collection
Preoperative, operative, and postoperative details were documented and collected from patients’ files, medical records and patient follow up visits. The outcome of surgery then was evaluated.
All cases before revision were subjected to extensive preoperative assessment that included:
Full history taking regarding the personal history, dietary history, eating habits, history of previous operations especially bariatric procedures, history of any associated comorbidities, medications history and full review of other systems.
General and local Examination was done. Laboratory work up done in the form of complete blood picture, coagulation profile, liver function tests, arterial blood gases, kidney function tests, lipid profile, thyroid profile & hemoglobin A1C.
All patients preoperatively were subjected to 3D reconstruction CT Gastroscopy for good anatomical assessment and delineation, Pelviabdominal ultrasound & upper gastrointestinal endoscopy to detect any esophagitis before the surgery. Respiratory function tests, chest X-ray, ECG and echo also were done.
Weight regain after initial weight loss, weight loss failure, and GERD -whether it is presented before the primary restrictive procedure and not corrected or de-novo development after it- were the main indications for the revision and subsequently the conversion to Rouxen- Y gastric bypass. The presence and resolution of obesity-related co-morbid conditions like diabetes, hypertension, dyslipidemia, or sleep apnea were detected according to the use and discontinuation of medication postoperatively.
Patient was described as diabetic if HbA1c preoperatively is above 6.5%. The remission of diabetes detected with follow up of HbA1c and the reduction of used medications (insulin or oral hypoglycemic drugs). Remission of hypertension detected with blood pressure systolic and diastolic measurements with reduction of use of antihypertensive medications. The presence of preoperative sleep apnea syndrome was quantified by sleep studies and postoperative resolution by discontinued use of continuous positive airway pressure masks. Different components of lipid profile were followed up postoperatively to document the improvement of dyslipidemia.
The Results of Roux en-y-gastric bypasses were assessed as a revisional surgery regarding the following endpoints: weight loss, remission of metabolic disorders and development of any complication during the period of follow up.
Surgical technique
Patients were under general anesthesia and placed in anti- Trendelenburg position. Nasogastric tube inserted to empty the stomach before the initiation of procedure. Laparoscopic technique was used in all cases, but conversion to open method was done in 3 cases due to the presence of marked adhesions with the same steps.
In cases of gastric banding, the band was deflated 4 weeks before the revisional surgery.
The access to the abdominal cavity in most cases was obtained under vision using 12 mm visiport 2 fingers breadth above umbilicus in left paramedian line. Pneumoperitoneum then established and intraabdominal pressure was maintained. A 12 mm left-subcostal port is placed for the surgeon’s right hand, and a 12 mm right paramedian port is used for the surgeon’s left hand. A 5 mm port in the left mid axillary line for the assistant. A 5 mm incision in the subxiphoid region for hook liver retractor to elevate the left lobe of liver.
Adhesolysis then began with scissors and ultrasonic shears with lysis of all adhesions between stomach, Omentum, Liver and abdominal wall (Figure 1).
The dissection of right and left crus of diaphragm was done with identification of angle of Hiss.
Dissection between lesser omentum and lesser curvature of stomach was done with gain access to the lesser sac then dissection between posterior wall of stomach and pancreas.
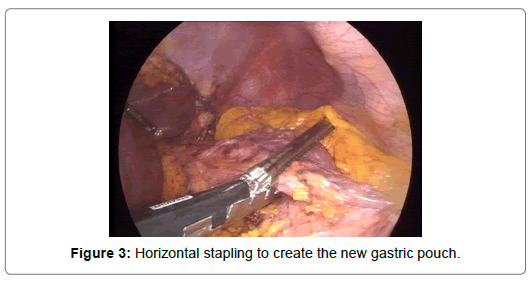
The neo gastric pouch was created by firing horizontal staplers Figures 2 and 3 using 60 mm Endopath linear stapler with green cartilage and then preceded vertically to angle of Hiss. In Case of revision after VBG, some cases had prolene mesh around the gastric pouch, the mesh was removed and the horizontal stapling started away from the mesh site, the old vertical staple line was identified and care was taken to avoid approaching it. The new gastric pouch was about 30 to 40 ml (Figure 4).
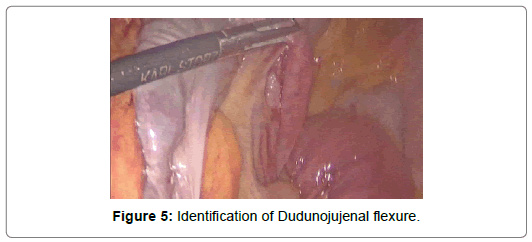
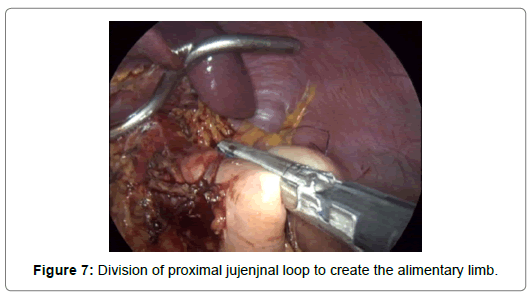
Treitz ligament was identified and then 50 cm distal to it a jejunal loop is brought up in ante colic manner and end to side gastrojejunostomy was performed using 60 mm Endopath stapler with blue cartilage and the anterior layer of the anastomosis was hand sewn with v lock suture 2/0, then using another liner stapler we cut the jejunal loop proximally to the anastomosis and make with it side to side Enteroenterostomy about 120 to 150 cm distal to the gastrojejunostomy (Figures 5-7).
The mesenteric defects (jejuno-jejunal mesenteric defect, transmesocolic space and retro alimentary space) were closed using non-absorbable prolene suture 2/0 to avoid internal herniation of intestinal loops.
Leak test was done using methylene blue injection through the bougie and stapler line was inspected for any leakage or bleeding with application of any hemostat clip if needed. Tube drain size 20 was inserted.
Postoperatively the nasogastric tube was removed and the patients were “nil by mouth” until performing water soluble gastrografine study on the 3rd postoperative day if there was no leakage they discharged from hospital between the 4th and 6th postoperative day and the patients started to take clear oral fluids for one week to be followed by blended soft diet on the next week then protein rich soft diet on third week.
Patients were followed up once every two weeks for the first month and then every 6 months for one year to monitor their postoperative outcome as regards general health condition, anthropometric measures, BMI, and development of any complications.
Data management and analysis
The collected data was revised, coded, tabulated, and introduced to a computerized system using Statistical package for Social Science. Data was presented, and suitable analysis was done according to the type of data obtained for each parameter.
Outcome measures
The comparison before and after Roux en y gastric bypass regarding the following endpoints after 3, 6, 9 and 12 months: weight loss (EWL% & BMI), metabolic outcome (D.M, hypertension control & Sleep apnea), Lipid profile & HbA1c.
Descriptive statistics
Mean, Standard deviation (± SD), Minimum and maximum values (range) for numerical data, frequency and percentage of nonnumerical data.
Statistical analysis
We performed Repeated measure Anova Test to assess the statistical significance of the difference before and after the conversion and to compare means across one or more variables that are based on repeated observations, Chi square test to determine whether there is a statistically significant difference between the expected frequencies and the observed frequencies in one or more categories of a contingency table, and Paired t-test to assess the statistical significance of the difference between two means of one quantitative variable measured twice for the same study group. With P- Value as indicator for level of significance where P>0.05: Non-significant (NS), P<0.05: Significant (S), and P<0.01: Highly significant (HS). Data were graphically represented using Power Point program.
Results
Among the patients included 28 were females (70%) and 12 were Males (30%) with a mean age of 47.20 ± 7.05. The patients done different primary restrictive procedures before the conversion to Roux-en-y gastric bypass: 21 patients (52.5%) VBG, 17 patients (42.5%) SG and 2 patients (5%) AGB.
All the demographic criteria of the patients are showed in Table 1.
| Variables | Demographic data |
|---|---|
| Patients number | 40 |
| Gender M: F | 12 (30%): 28 (70%) |
| Age (years) | |
| Mean ± SD | 47.20 ± 7.05 |
| Range | 37-60 |
| Type of 1ry restrictive procedure (laparoscopic: open) | 31:9 |
| Time from 1ry operation till conversion (months) | |
| Mean ± SD | 79.98 ± 44.59 |
| Range | 34-180 |
| Height (cm) | |
| Mean ±SD | 170.98 ± 7.95 |
| Range | 155-190 |
| Weight (Before 1ry operation)/kg | |
| Mean ± SD | 132.25 ± 11.60 |
| Range | 110-155 |
| BMI (Before 1ry operation) | |
| Mean ± SD | 45.35 ± 4.24 |
| Range | 37.2-54.7 |
| Weight (BC)/Kg | |
| Mean ± SD | 113.50 ± 9.92 |
| Range | 98-135 |
| BMI (BC)/kg | |
| Mean ± SD | 39.06 ± 4.91 |
| Range | 30.5-48.8 |
| EBW (BC)/Kg | |
| Mean ± SD | 40.49 ± 12.08 |
| Range | 19-62 |
| EWL % (BC) | |
| Mean ± SD | 30.88 ± 17.80 |
| Range | 6.25-74.3 |
Table 1: Preoperative demographic criteria.
Each patient had different indication for the required Roux en y gastric bypass conversion. 18 patients (45%) due to weight regain after 1ry weight loss, 14 patients (35%) due to insufficient weight loss and 8 patients (20%) due to GERD. 5 patients out from the 8 were suffering from De-novo GERD that was established after their primary restrictive procedure.
Different causes were investigated regarding the weight regain and insufficient weight loss failure and presented in Table 2.
| Causes of weight regain /insufficient weight loss | Number of patients | Percentage of total (40 patients) |
|---|---|---|
| Pouch dilatation | 12 | 30% |
| Sweet eaters | 6 | 15% |
| Staple line disruption | 5 | 12.5% |
| Band migration | 1 | 2.5% |
| Unknown | 8 | 20% |
Table 2: Causes of weight regain & insufficient weight loss.
While different indications for conversion are showed in Table 3.
| Indication of conversion | Operation before conversion | |||||
|---|---|---|---|---|---|---|
| VBG (52.5%) | Sleeve gastrectomy (42.5%) | Gastric Band (5%) | ||||
| No. | % | No. | % | No. | % | |
| GERD (20%) | 3 | 14.30% | 5 | 29.40% | 0 | 0.00% |
| Weight regain (45%) | 12 | 57.10% | 5 | 29.40% | 1 | 50.00% |
| Insufficient weight loss (35%) | 6 | 28.60% | 7 | 41.20% | 1 | 50.00% |
Table 3: Number and Percentage of patients with different indications for conversion to Roux en Y gastric bypass.
Among the 40 patients: 3 patients were converted intraoperatively from laparoscopic to open approach due to extensive adhesions presented from previous operations. (Rate of conversion=7.5%)
Moreover, 12 patients (30%) performed concomitant cholecystectomy during the Roux-en-Y gastric bypass due to the preoperative presence of gall stones.
The mean time for the operation was 148.75 ± 30.38 minute and the mean time for hospital stay was 4.58 ± 1.71 day with a range of 2 to 9 days.
Post-operatively one patient complained from severe abdominal tenderness with signs of peritonitis, tachycardia and tachypnea on postoperative day 7, and Pelvi-abdominal Ct scan with contrast was done and it showed leakage at the gastrojejunostomy anastomosis. Exploration was done with revisioning of the anastomosis and suturing of the defect with peritoneal toilet and drainage. The patient discharged postoperatively in ICU but unfortunately died 4 days later from sever sepsis (Mortality rate 2.5%). One patient developed DVT and was managed conservatively with therapeutic anticoagulants and 2 patients developed wound infection and managed also conservatively during the follow up period.
The follow up of Weight and BMI after the conversion over one year show significant reduction: Mean weight of the patients before conversion was 113.50 ± 9.92 kg, 109.70 ± 9.86 after one month, 104.25 ± 9.98 after 3 months, 98.65 ± 9.93 after 6 months, 93.88 ± 9.99 after 9 months and became 89.18 ± 9.84 after 12 months (Figure 8).
The mean BMI significantly decrease from 39.06 ± 4.91 before the conversion to 33.93 ± 4.44 and 30.65 ± 4.11 at 6 and 12 months respectively. P value of BMI was highly significant after 12 months (<0.001) (Figure 9).
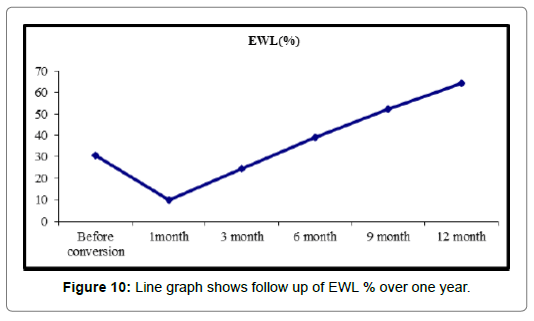
EWL% mean was markedly increased from 30.88 ± 17.80% before conversion to 39.18 ± 14.71% at 6 months and 64.47 ± 19.58% at 12 months as showed in Figure 10.
All the 8 patients in the study presented with GERD show improvement after the conversion to Roux en y bypass with relieve of the reflux symptoms and discontinuation of PPIs.
From total of 40 patients: 13 patient (32.5%) were diabetic: 7 (17.5%) from them were on oral therapy, and 6 (15%) were on Insulin; at 6 months 8 patients (20%) need no treatment and only 5 patients were diabetic of which 3 (7.5%) on insulin and 2 (5%) on oral therapy: at 12 months 11 patients (27%) need no treatment and just 2 (5%) patients were diabetic one (2.5%) on oral therapy and other (2.5%) on insulin (P-value=0.002). The mean HbA1c is markedly reduced from 7.74 ± 0.70 before conversion to be 6.05 ± 0.43 and 5.14 ± 0.23 at 6 & 12 months respectively (P-value=<0.001).
The number of patients with HTN before the conversion was 23 (57.5%) and became 10 (25%) at 6 months follow up and only 6 (15%) at one year (P- value=<0.001).
Patients with sleep apnea were 12 (30%) before conversion and became 5 (12.5%) at 6 months and finally 2 (5%) at 12 months (P-value=0.007).
As previously discussed, the improvement of co-morbidities associated with roux en y gastric bypass from diabetes, hypertension, and sleep apnea as compared to previous restrictive procedures each patient undergoes. The Remission of associated comorbidities is shown in Table 4.
| Before conversion | 3 month | 6 month | 9 month | 12 month | Test value* | P-value | Sig. | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | No. | % | No. | % | ||||
| DM | |||||||||||||
| No | 27 | 67.5% | 32 | 80.0% | 35 | 87.5% | 38 | 95.0% | 38 | 95.0% | 16.863 | 0.002 | HS |
| DM | 13 | 32.5% | 8 | 20.0% | 5 | 12.5% | 2 | 5.0% | 2 | 5.0% | |||
| Chi-square test | -- | 1.614 | 4.588 | 9.928 | 9.928 | ||||||||
| P-value | -- | 0.204 (NS) | 0.032 (HS) | 0.002 (HS) | 0.002 (HS) | ||||||||
| HTN | |||||||||||||
| No | 17 | 42.5% | 25 | 62.5% | 30 | 75.0% | 33 | 82.5% | 34 | 85.0% | 21.646 | <0.001 | HS |
| HTN | 23 | 57.5% | 15 | 37.5% | 10 | 25.0% | 7 | 17.5% | 6 | 15.0% | |||
| Chi-square test | -- | 3.208 | 8.717 | 13.653 | 15.632 | ||||||||
| P-value | -- | 0.073 (NS) | 0.003 (HS) | <0.001 (HS) | <0.001 (HS) | ||||||||
| Sleep apnea | |||||||||||||
| No | 28 | 70.0% | 29 | 72.5% | 35 | 87.5% | 36 | 90.0% | 38 | 95.0% | 13.962 | 0.007 | HS |
| Sleep apnea | 12 | 30.0% | 11 | 27.5% | 5 | 12.5% | 4 | 10.0% | 2 | 5.0% | |||
| Chi-square test | -- | 0.061 | 3.660 | 5.000 | 8.658 | ||||||||
| P-value | -- | 0.805 (NS) | 0.056 (NS) | 0.025 (S) | 0.003 (HS) | ||||||||
Table 4: Number and Percentage of patients with different comorbidities and follow up over one year.
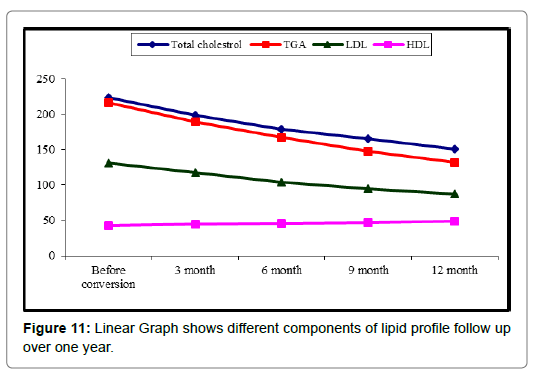
Regarding the lipid profile of the patients, Roux en Y gastric bypass markedly improve the TGA and Cholesterol levels with significant reduction also of LDL and increase of HDL.
The mean level of cholesterol before conversion was 223.43 ± 27.95 and reduced to 179.15 ± 20.17 and 151.28 ± 15.82 at 6 and 12 months respectively. TAG markedly decreased from 216.88 ± 20.81 before conversion to 132.70 ± 15.01 after one year (P-value=<0.001) (Figure 11).
Discussion
Sleeve Gastrectomy, Adjustable Gastric Band and VBG all follow the gastric restricting technique; weight regain, or weight loss failure are the most commonly encountered causes of failure [7]. These are causes can arise either due to possible physiological changes or dilation of residual stomach. Other less common causes are complications including GERD that are directly attributable to the used technique. According to Golomb et al, postoperative follow ups reported significant excess weight loss (EWL) in the first year (76.8%). EWL declined excessively in consecutive years after with a decline from the previous loss to 69.7% after 3 years and 56.1% after 5 years. Roux-en-Y gastric bypass is considered an important choice as a provisional surgery to achieve substantial long-term weight loss as it combines both the principles of restriction and malabsorption technique to achieve long term excess weight loss [8] and as a revisional surgery after failure of a primary restrictive technique [9,10]. The superiority of one revisional technique over the other is still under study and a gold standard choice hasn’t yet been reported. Many failures have been reported from the sleeve gastrectomy: Weight regain which can be due to many theories some go to the lack of physical activity, lack of follow up, or lack of change of the nutritional behavior, thus the importance of proper nutritional counseling has been supported by the literature [11]. In addition to the craving for sweet eating which tends to increase interestingly from sleeve gastrectomy [12], High calorie food – junk food- will be instantly absorbed leading to potential obvious weight gain as sleeve gastrectomy is not a malabsorptive procedure. Other theory supports the endocrine evidence behind weight gain stating that in SG part of gastric fundus is removed which is responsible for producing Ghrelin, hunger hormone, which will be reflected as decrease in appetite due to maintained reduced ghrelin levels for only one year following the procedure. A recent systematic review by Anderson et al. reported that ghrelin levels were significantly reduced at 3, 6 and 12 months after laparoscopic SG [13]; however, 46.7% of the patients only lost the feeling of hunger after 3 years which is significantly dropped from 75% of SG patients which were reported after one year of follow up due to compensatory increase in the plasma level of ghrelin [12,13]. Still, the evidence about the effect of ghrelin following bariatric surgery and its implications on weight loss or gain remains unclear in literature.
Other failure that might precede the SG is GERD. GERD has been one of the main co-morbidities that happened with SG which has been reported after 3, 5 years of follow up and has been the most frequent reason for reoperation after SG [14]. Both patients with preoperative GERD got worsen symptoms after the SG and patients who reported no symptoms preoperative had de novo GERD postoperative [15,16]. Several pathophysiological and anatomical changes that encounter the lower esophageal sphincter are the causes of GERD postoperative. The most important mechanism for the development of GERD after LSG is associated with intragastric high pressure after resection of the fundus [17]. Some Authors demonstrated by means of High Resolution Mometry (HRM) and combined 24-h pH and Multichannel Intra- Luminal Impedance (MII-pH) how the increased in post prandial reflux can be caused by increase of intra-gastric pressure caused by the tubulization of stomach. The second mechanism is related to the destruction of LES by LSG. It is possible that LSG may damage the sling fiber around Esophago-Cardiac (EC) junction and impair the LES [18- 20]. Also adding to weight of its opposing side, sleeve gastrectomy has a lot of metabolic effects on the long run which may predispose to many dangerous chronic illness [21].
Although many skeptical thoughts that roux en y gastric bypass is more invasive and may exposed the patients to wide of concerns related to surgery and postoperative long list of medical requirements, roux en y gastric bypass showed a better success rates rather than any other procedure leaving postoperatively minimal or nearly no probability of failure and without complications compared to other techniques [22,23]. Out weighting the benefit and removing the burden of surgical procedure, Laparoscopic Roux-en- y gastric bypass offers benefits likewise other laparoscopic procedures including reducing post-operative hospital stay, pain, complications and ensuring a fast recovery. In particular high risk morbidly obese patients with multiple co-morbidities benefits a lot from such less invasive approach as decreasing the risk of cardiopulmonary manifestation and related complication that they are vulnerable to [24]. Moreover, laparoscopic roux en y gastric bypass achieves unpreceded success rates as weight loss averages 65% for most patients with over 85% of patients losing and maintaining 50% initial excess weight loss. Contemporary series have documented mortality rates of approximately 0.1% and serious early complication rates of 5%. Long-term issues with fat malabsorption, protein-energy malnutrition and micronutrient deficiencies are relatively uncommon and can usually be managed with oral supplementation [25].
Roux en y gastric bypass as revisional strategy after failed primary restrictive surgeries, Marti-Fernandez et, al. [26] used same approach as ours, and compared same co-morbidities we selected: DM, HTN, dyslipidemia. He enrolled 60 patients, and performed an observational, retrospective study including patients initially operated on for morbid obesity with restrictive techniques (vertical-banded gastroplasty [VBG], adjustable gastric band [AGB], and sleeve gastrectomy) and re-operated with RYGB to investigate the value of Roux-en-Y gastric bypass (RYGB) as a revisional procedure after restrictive surgery. His study showed that VBG was the most frequent initial procedure (n=33), and the average initial weight was 143.53 ± 28.6 kg. Weight loss was achieved in all groups, with a median excess weight loss of 58% after the first surgery and 40.3% after gastric bypass. In terms of weight loss, the best results after the second surgery were obtained when the first surgery was AGB, with statistically significant differences. A decrease in the prevalence of the comorbidities was observed: 38.7% for type 2 DM, 35.5% for arterial hypertension, 27.4% for dyslipidemia, and 22.6% for COPD prior to the first surgery, which became 25.8, 32.3, 25.8, and 19.4% after the first intervention, and 16.1, 25, 14.3, and 17.9% after the second intervention, respectively. Although Marti-Fernandez enrolled a large number of patient, stating data about COPD as a co-morbidity, and showing the occurrence of postoperative complications which were a head from our study, we provided more follow up data at before conversion, 3, 6, 9, 12 months and a detailed description about the co-morbidities with the need and no need of treatment for diabetic patients and the type of treatment used, and we also presented sleep apnea as co-morbidity which was not presented before in related literature.
In our study 40 patients were included: 28 females (70%) and 12 were Males (30%) with a mean age of 47.20 ± 7.05. The patients done different primary restrictive procedures before the conversion to Rouxen- y gastric bypass: 21 patients (52.5%) VBG, 17 patients (42.5%) SG and 2 patients (5%) AGB. Each patient had different indication for the required Roux en y gastric bypass conversion. 18 patients (45%) due to weight regain after 1ry weight loss, 14 patients (35%) due to insufficient weight loss and 8 patients (20%) due to GERD. 5 patients were suffering from De-novo GERD that was established after their primary restrictive procedure. All the patients with GERD show improvement after the conversion with relieve of the reflux symptoms and discontinuation of PPIs. As a primary restrictive procedure: 9 out of 40 patients (22.5%) undergo open approach, while 31 patients (77.5%) undergo Laparoscopic approach; results of the follow up of weight and BMI after the conversion over one year show significant reduction: Mean weight of the patients before conversion was 113.50 ± 9.92 kg, 109.70 ± 9.86 after one month, 104.25 ± 9.98 after 3 months, 98.65 ± 9.93 after 6 months, 93.88 ± 9.99 after 9 months and became 89.18 ± 9.84 after 12 months. The mean BMI significantly decrease from 39.06 ± 4.91 before the conversion to 33.93 ± 4.44 and 30.65 ± 4.11 at 6 and 12 months respectively. P value of BMI was highly significant after 12 months (<0.001). EWL% mean was markedly increased from 30.88 ± 17.80% before conversion to 39.18 ± 14.71% at 6 months and 64.47 ± 19.58% at 12 months.
The common co-morbidities with bariatric surgeries like diabetes, hypertension, sleep apnea, and dyslipidemia were all improved with the performed LRYGB. Starting before conversion with 13 diabetic patients who need treatment, our study showed improvement of the diabetic profile of all patients as the mean HbA1c is markedly reduced from 7.74 ± 0.70 before conversion to be 6.05 ± 0.43 and 5.14 ± 0.23 at 6 & 12 months respectively (P-value=<0.001).
Hypertension and sleep apnea find their ways in the improvement race of the data as the number of patients with HTN before the conversion was 23 (57.5%) and became 10 (25%) at 6 months follow up and only 6 (15%) at one year (P- value=<0.001), and Patients with sleep apnea were 12 (30%) before conversion and became 5 (12.5%) at 6 months and finally 2 (5%) at 12 months (P-value=0.007). Moreover, Regarding the lipid profile of the patients, the Roux en Y gastric bypass markedly improve the TGA and Cholesterol levels with significant reduction also of LDL and increase of HDL. The mean level of cholesterol before conversion was 223.43 ± 27.95 and reduced to 179.15 ± 20.17 and 151.28 ± 15.82 at 6 and 12 months respectively. TAG markedly decreased from 216.88 ± 20.81 before conversion to 132.70 ± 15.01 after one year (P-value= <0.001).
The question of which revisional strategy after failed primary restrictive procedures requires further research with larger study populations, patient’s criteria and individual variations among patients. Roux en Y till the present and by our results makes it the possible answer for a gold standard. However, the only drawback was the number of populations selected however, individual variations and patient criteria diversity were assessed during choosing the studied population.
Conclusion
Roux en y gastric bypass is a safe surgical procedure with satisfactory outcomes and can be proposed as first line management choice to revise failed primary restrictive bariatric procedures.
References
- Ogden CL, Flegal KM, Carroll MD, Johnson CL (2002) Prevalence and trends in overweight among US children and adolescents, 1999-2000. JAMA 288: 1728-1732.
- Buchwald H, Williams SE (2004) Bariatric surgery worldwide 2003. Obesity Surgery 14: 1157-1164.
- Hruby A, Hu FB (2015) The epidemiology of obesity: A big picture. Pharmacoeconomics. 33: 673-689.
- Maggard MA, Shugarman LR, Suttorp M, Maglione M, Sugerman HJ, et al. (2005) Meta-analysis: Surgical treatment of obesity. Annals of Internal Medicine 142: 547-559.
- Perry Y, Courcoulas AP, Fernando HC, Buenaventura PO, McCaughan JS, et al. (2004) Laparoscopic Roux-en-Y gastric bypass for recalcitrant gastroesophageal reflux disease in morbidly obese patients. JSLS: Journal of the Society of Laparoendoscopic Surgeons 8: 19.
- Gagner M, Gentileschi P, de Csepel J, Kini S, Patterson E, et al. (2002) Laparoscopic reoperative bariatric surgery: Experience from 27 consecutive patients. Obesity Surgery 12: 254-260.
- Saliba C, El Rayes J, Diab S, Nicolas G, Wakim R (2018) Weight regain after sleeve gastrectomy: A look at the benefits of re-sleeve. Cureus.
- Sugerman HJ, Kellum JM, DeMaria EJ (1997) Conversion of proximal to distal gastric bypass for failed gastric bypass for superobesity. J Gastrointestinal Surgery 1: 517-525.
- Soricelli E, Iossa A, Casella G, Abbatini F, Calì B, et al. (2013) Sleeve gastrectomy and crural repair in obese patients with gastroesophageal reflux disease and/or hiatal hernia. Surgery for Obesity and Related Diseases 9: 356-361.
- Gonzalez-Heredia R, Sanchez-Johnsen L, Valbuena VS, Masrur M, Murphey M, et al. (2016) Surgical management of super–super obese patients: Roux-en-Y gastric bypass versus sleeve gastrectomy. Surgical endoscopy. 30: 2097-2102.
- Lee WJ, Almalki O (2018) Gastro esophageal reflux disease after sleeve gastrectomy: a real issue and future perspectives. Am J General GI Surg 1: 1001.
- Himpens J, Dapri G, Cadière GB (2006) A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: Results after 1 and 3 years. Obesity Surgery. 16: 1450-1456.
- Anderson B, Switzer NJ, Almamar A, Shi X, Birch DW, et al. (2013) The impact of laparoscopic sleeve gastrectomy on plasma ghrelin levels: A systematic review. Obesity Surgery 23: 1476-1480.
- Peterli R, Wölnerhanssen BK, Peters T, Vetter D, Kröll D, et al. (2018) Effect of laparoscopic sleeve gastrectomy vs laparoscopic Roux-en-Y gastric bypass on weight loss in patients with morbid obesity: The SM-BOSS randomized clinical trial. Jama 319: 255-265.
- Klaus A, Weiss H (2018) Is preoperative manometry in restrictive bariatric procedures necessary? Obesity Surgery 18: 1039-1042.
- Attia SG (2017) Laparoscopic sleeve gastrectomy and crural repair as a treatment of morbid obesity associated with gastroesophageal reflux. Electronic Physician 9: 3529.
- Lee WJ, Almalki O (2018) Gastro esophageal reflux disease after sleeve gastrectomy: A real issue and future perspectives. Am J General GI Surg 1: 1001.
- Mion F, Tolone S, Garros A, Savarino E, Pelascini E, et al. (2016) High-resolution impedance manometry after sleeve gastrectomy: Increased intragastric pressure and reflux are frequent events. Obesity Surgery. 26: 2449-2456.
- Frenkel C, Telem DA, Pryor AD, Altieri MS, Shroyer KR, et al. (2016) The effect of sleeve gastrectomy on extraesophageal reflux disease. Surgery for Obesity and Related Diseases 12: 1263-1269.
- Del Genio G, Tolone S, Limongelli P, Brusciano L, D’Alessandro A, et al. (2014) Sleeve gastrectomy and development of “de novo†gastroesophageal reflux. Obesity Surgery 24: 71-77.
- Golomb I, David MB, Glass A, Kolitz T, Keidar A (2015) Long-term metabolic effects of laparoscopic sleeve gastrectomy. JAMA Surgery 150: 1051-1057.
- Sarkhosh K, Birch DW, Sharma A, Karmali S (2013) Complications associated with laparoscopic sleeve gastrectomy for morbid obesity: a surgeon’s guide. Canadian J Surgery 56: 347.
- Li J, Lai D, Wu D (2016) Laparoscopic Roux-en-Y gastric bypass versus laparoscopic sleeve gastrectomy to treat morbid obesity-related comorbidities: A systematic review and meta-analysis. Obesity Surgery 26: 429-442.
- Schauer PR, Ikramuddin S, Gourash W, Ramanathan R, Luketich J (2000) Outcomes after laparoscopic Roux-en-Y gastric bypass for morbid obesity. Annals of Surgery 232: 515.
- Madura JA, II JK (2012) Quick fix or long-term cure? Pros and cons of bariatric surgery. F1000 Medicine Reports.
- Marti-Fernandez R, Cassinello-Fernandez N, Cuenca-Ramirez MD, Lapeña-Rodriguez M, Fernandez-Moreno MC, et al. (2020) Roux-en-Y gastric bypass as an effective bariatric revisional surgery after restrictive procedures. Obesity Facts 3: 1-8.
Citation: Elgazar A, El Seidy SE, Khalil M, Elmaleh H, Mandel D (2020) Roux en Y Gastric Bypass after Failed Primary Restrictive Procedures in Morbidly Obese Patients. J Obes Weight Loss Ther 10: 410. DOI: 10.4172/2165-7904.1000410
Copyright: © 2020 Elgazar A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3106
- [From(publication date): 0-2020 - Dec 08, 2025]
- Breakdown by view type
- HTML page views: 2181
- PDF downloads: 925