Serum Hepcidin Level and Human Factors Engineering (HFE) C282Y Mutation in Egyptian Children with Beta-Thalassemia
Received: 27-Jul-2017 / Accepted Date: 26-Aug-2017 / Published Date: 04-Sep-2017 DOI: 10.4172/2168-9652.1000223
Abstract
Objective: Thalassemia is an important hematological disorder. The possibility of iron overload development may be increase by Interaction between thalassemia and HFE gene mutations. This study aim to investigate the possible association between serum hepcidin level as indicator of iron concentration and the presence of HFE gene mutations.
Methods: The study contains two groups, group I: include seventy six children with beta thalassemia, group II include 51 apparently healthy gender and age matched children served as controls. Children was passed through full history taking, clinical examination. Complete blood picture, iron, ferritin, hepcidin, renal and liver functions were measured. HFE gene C282Y mutation was assayed by SNP real time PCR.
Results: Frequency of the A genotype and A allele of HFE gene C282Y mutation shows a significant increase in beta thalassemia group in comparison controls. Also, serum Iron and ferritin levels were significantly increase with decrease in hepcidin level in AA when compared to AG and GG genotypes. The splenectomy percent was significantly increased among AA genotype in the patient group. The number and % of patients with ferritin level equal or more than 2500 ng/ml and decrease in hepcidin level as an index of iron overload was significantly increase in patients with AA and AG genotypes.
Conclusion: There were significant negative associations between serum hepcidin levels as indication of iron toxicity and HFE C282Y mutation in Egyptian Beta thalassemia children.
Keywords: TM; Hepcidin; HFE; Mutation
Introduction
Thalassemias are inherited autosomal recessive disorders due to a defect in α or β-globin chain synthesis characterized by reducing the rate of hemoglobin synthesis [1].
Regular blood transfusion therapy in thalassemic children leads to increased risk of iron overload with its related complications [2].
It can result in progressive organ damage in a condition called hemosiderosis leads to growth retardation and delay of sexual maturation in children [3].
So, it is critical to maintain normal iron levels in those children. As in human, iron is unable to be eliminated by the excretory route; iron will be regulated only by intestinal absorption [4].
Mutations in genes involved in the regulation of systemic iron homeostasis may cause an autosomal recessive disorder called hereditary hemochromatosis [5].
Patients with hemochromatosis exhibit increased expression of iron transporters that result in hyper-absorption of iron from the diet with lacking a regulated mode of iron excretion results in systemic iron overload [6].
The hepatocytes secret a hormone called hepcidin, regulates iron level in the plasma. Persistent increase of hepcidin causes ironrestricted anemia, whereas hepcidin deficiency results in iron excess with precipitation of iron in the liver and other parenchyma [7,8].
A useful method for diagnose the patients at higher risk of iron toxicity may be the determination of hepcidin concentrations [9].
A mutation in the Human Factors Engineering (HFE) gene was identified as the cause for around 65% of the cases of classic hemochromatosis in the Mediterranean region [10].
HFE gene located on chromosome 6p [11]. The mutation most responsible for iron overload in the HFE protein is an amino acid substitution of tyrosine for cysteine at position 282 [12].
This study aim to detect the HFE gene C282Y mutation and its relationship with iron excess and hepcidin levels in Beta-thalassemia children.
Subjects and methods
Subjects: The study conducted on 76 children with β-thalassemia consists of 36 girls and 40 boys on regular packed red cell transfusion came to Menoufia University Hospital, Egypt at Pediatric Hematology Clinic, their age was 7.55 ± 4.24 years.
Excluded criteria include serological evidence of hepatitis B or C, diabetes mellitus thyroid and renal dysfunctions.
29 boys and 22 girls apparently healthy children age and gender matched served as a control group. Their age was 8.31 ± 4.19 years.
Ethical clearance from Faculty of Medicine, Menoufia University ethical committee was obtained and Informed consent was taken from the legal guardians of the included children before participation.
Included patients were passed through detailed history taking and clinical examination. For each participant, body weight and height were measured by the standard methods with estimation of body mass index (BMI=weight in kg/height in m2).
Blood sampling: 7 mL of venous blood were withdrawn from each subject and divided as follows: 3 mL in a vacutainer plain test tube and was left to clot and then centrifuged at 3000 rpm for 10 min, serum was then separated and stored at -80°C until used for measurement of Iron, ferritin, hepcidin, Renal and liver functions. 4 mL of venous blood were delivered in a two vacutainer EDTA-containing tube one for complete blood picture estimation and the other for detection of HFE gene C282Y mutation.
Assay methods: Complete blood picture was measured with Pentra-80 automated blood counter (ABX–France–Rue du Caducee- Paris Euromedecine-BP-7290.34184 Montpellier-Cedex 4.)
Liver enzymes (ALT, AST), Renal function tests (serum creatinine and blood urea) and alkaline phosphatase were analyzed on autoanalyzer (SYNCHRON CX5) from Beckman (Beckman, instrument Inc., Scientific Instrument Division, Fullerton, CA92634 - 3100). Quantitative colorimetric measurement of Iron was done [13].
Serum ferritin and hepcidin were determined using commercial ELISA kits (Immunodiagnostic Systems Limited, Bolden, UK) and EIAab® Human Hepcidin prohormone ELISA kit, China, respectively [14]. HFE gene (C282Y) rs1800562 mutation.
Genomic DNA was extracted from whole blood using the Whole Blood Genomic DNA extraction Kit (Thermo Scientific, Vilnius, Lithuania). HFE gene (C282Y) rs1800562 mutation was detected using the TaqMan allelic discrimination Assay technique that detects variants of a single nucleic acid sequence. The actual quantity of target sequence is not determined. The allelic discrimination assay classifies unknown samples as follows: Homozygotes samples with only allele 1 or allele 2 or Heterozygotes samples with both alleles 1 and 2. Using the universal taqMan Master Mix from Thermo scientific, the primers and Taqman probes were designed by Applied Biosystems (Foster City, CA, USA) Life Technologies. The reaction mixture was prepared by mixing 10 ul of master mix, 1.25 μl of 20x SNP assay kit contain primers and probes and 3.75 μl of DNAse-free water. For each unknown reaction, 5 μl of genomic DNA template was added and for the negative control reaction, 5 μl of DNAse-free water was added.
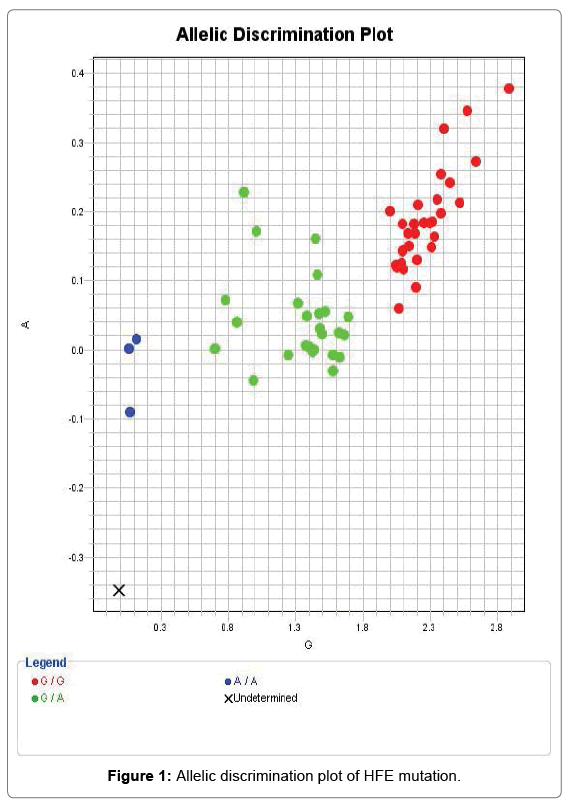
The cycling condition were set as follows: 50°C for 1 min Pre-PCR read, then 95°C for 10 min and 45 cycles of 95°C for 15 s, 60°C for 1 min (cycling) and 60°C for 1 min (Post-PCR).using the 7500 Real-time PCR system (Applied Biosystems, Foster City, CA, USA). The mutation appears in allelic discrimination plot (Figure 1).
Statistical Analysis
Data entry, coding and analysis were undergone using SPSS (20), IBM Corp. Released 2011. IBM SPSS Statistics for Windows, Version 20.0. Armonk, NY: IBM Corp. Data of this study was of both quantitative and qualitative types. Quantitative data were expressed in Mean (x̅) and Standard Deviation (SD), while qualitative data were expressed in frequency (number) and percent (%).Tests of significance used were: Chi square test, T student test, ANOVA (Analysis of Variance).
Results
The results of this study show a significant lower body weight, height in children with β-thalassemia compared to the controls. Also, a significant difference in number and % of children has be done splenectomy operation in patients group compared to control (Table 1).
| Group 1 (n=76) Mean ± SD |
Group 2 (n=51) Mean ± SD |
t- test | P value | |
|---|---|---|---|---|
| Age (years) | 7.55 ± 4.24 | 8.31 ± 4.19 | 0.996 | >0.05 |
| Gender Male No % Female No % |
41 53.9% 35 46.1% |
29 56.9% 22 43.1% |
χ2=0.10 | >0.05 |
| Weight in Kg | 23.93 ± 11.73 | 28.76 ± 13.25 | 2.158 | <0.05* |
| Height (cm) | 115.68 ± 25.84 | 126.15 ± 25.54 | 2.249 | <0.05* |
| BMI | 17.04 ± 2.87 | 16.93 ± 1.62 | 0.236 | >0.05 |
| Splenectomy Positive No % Negative No % |
28 36.8% 48 63.2% |
00 00% 51 100% |
χ2=24.10 | <0.001** |
Table 1: Comparison between the studied groups regarding demographic and clinical data in patient and control.
There was a significant increase in ALT, AST, alkaline phosphatase, ferritin, Iron levels, hepcidin levels, MCV, MCH, RDW values and WBCs count in β-thalassemia patients compared to control. While there was a significant decrease of hemoglobin levels, RBCs count and TIBC (Table 2).
| Group 1 (n=76) Mean ± SD |
Group 2 (n=51) Mean ± SD |
t- test | P value | |
|---|---|---|---|---|
| AST (IU/L) | 98.53 ± 100.89 | 28.07 ± 4.68 | 4.977 | <0.001** |
| ALT (IU/L) | 133.15 ± 283.20 | 28.11 ± 3.86 | 2.645 | <0.01** |
| Creatinine (mg/dl) | 0.69 ± 1.08 | 0.96 ± 1.70 | 1.064 | >0.05 |
| Urea (mg/dl) | 31.88 ± 8.52 | 30.68 ± 5.81 | 0.873 | >0.05 |
| ALP (IU/L) | 362.73 ± 85.32 | 96.01 ± 9.14 | 6.618 | <0.001** |
| Ferritin ( ng/ml) | 2334.27 ± 1779.49 | 97.78 ± 25.33 | 8.963 | <0.001** |
| Iron (ug/dl) | 195.17 ± 71.19 | 81.47 ± 10.31 | 11.311 | <0.001** |
| TIBC (ug/dl) | 144.27 ± 79.84 | 293.80 ± 25.65 | 12.919 | <0.001** |
| Hepcidin (ng/ml) | 66.90 ± 14.47 | 76.72 ± 16.53 | 18.931 | <0.001** |
| WBCs (× 103/L) | 22.83 ± 25.67 | 7.03 ± 2.36 | 4.377 | <0.001** |
| RBCs (× 106/L) | 2.83 ± 0.59 | 4.73 ± 0.34 | 17.317 | <0.001** |
| Hb (gm/dl) | 7.77 ± 1.76 | 11.72 ± 1.27 | 13.266 | <0.001** |
| Platetets count (× 103/L) | 409.17 ± 269.53 | 326.27 ± 83.94 | 2.126 | <0.05* |
| MCV (µm3) | 78.49 ± 6.5 | 74.6 ± 8.8=52 | 2.907 | <0.05* |
| MCH (pg) | 27.58 ± 3.34 | 24.87 ± 2.84 | 4.680 | <0.01** |
| RDW (%) | 35.07 ± 3.47 | 34.14 ± 0.52 | 6.166 | <0.001** |
Table 2: Comparison between the studied groups regarding laboratory data, iron related parameters in patient and control.
There was a significantly increased frequency of the A genotype and A allele of HFE gene (C282Y) mutation in patients group compared to controls with confidence interval 95% Odd Ratio was 1.69 (1.46-1.96) between AA genotypes, 3.70 (1.53-8.94) between AG genotypes and 3.78 (1.67-8.50) between A allele in the two group (Table 3).
| Group 1 (n=76) No. % |
Group 2 (n=51) No. % |
χ2 | P value | OR (CI 95%) | |
|---|---|---|---|---|---|
| rs2228570 genotypes: A/A genotype A/G genotype G/G genotype |
3 3.9% 31 40.8% 42 55.3% |
0 0.0% 8 15.7% 43 84.3% |
12.12 | 0.002 | 1.69 (1.46-1.96). 3.70 (1.53-8.94). Reference genotype. |
| Allele frequency A allele G allele |
37 24.35% 115 75.65% |
8 7.85% 94 92.15% | 3.12 | 0.001 | 3.78 (1.67-8.50) Reference Allele |
Table 3: Comparison between the studied groups regarding genotype and allele frequency.
There was significant differences among AA, AG and GG types of HFE gene (C282Y) mutation as regard ALT, AST, urea, creatinine, alkaline phosphatase, ferritin, Iron levels and WBCs count in β-thalassemia patients with significant increase in AA genotype than both AG and GG genotypes. Also, there was significant increase in splenectomy percent among AA genotype than other two genotypes in patients group. While there was a significant decrease of hepcidin levels in AA genotype than both AG and GG genotypes (Table 4).
| A/A (n=3) Mean ± SD |
A/G (n=31) Mean ± SD |
G/G (n=42) Mean ± SD |
ANOVA | P value | |
|---|---|---|---|---|---|
| AST (IU/L) | 313.33 ± 60.28 | 99.87 ± 99.94 | 82.84 ± 86.47 | 8.883 | <0.001** |
| ALT (IU/L) | 333.33 ± 80.83 | 106.45 ± 103.32 | 87.14 ± 88.81 | 9.445 | <0.001** |
| Creatinine (mg/dl) | 0.97 ± 0.06 | 0.65 ± 0.21 | 0.58 ± 0.200 | 5.512 | <0.01** |
| Urea (mg/dl) | 44.67 ± 1.53 | 31.87 ± 8.47 | 30.98 ± 8.22 | 3.888 | <0.05* |
| ALP (IU/L) | 510.00 ± 45.83 | 369.87 ± 83.60 | 346.95 ± 78.88 | 6.001 | <0.001** |
| Ferritin (ng/mL) | 5966.67 ± 907.38 | 2486.45 ± 1683.67 | 1962.5 ± 1598.02 | 8.793 | <0.001** |
| Iron (ug/dl) | 293.33 ± 15.27 | 207.06 ± 68.9 | 179.38 ± 68.69 | 4.749 | <0.001** |
| TIBC (ug/dl) | 58.0 ± 2.65 | 135.87 ± 81.95 | 156.64 ± 77.42 | 2.525 | <0.05* |
| Hepcidin (ng/ml) | 63.45 ± 12.34 | 68.68 ± 14.32 | 97.0 ± 1.73 | 9.757 | <0.001** |
| WBCs (× 103/L) | 75.93 ± 59.20 | 26.30 ± 24.63 | 16.48 ± 18.27 | 9.876 | <0.001** |
| RBCs (× 106/L) | 3.15 ± 0.54 | 2.84 ± 0.57 | 2.82 ± 0.63 | 0.416 | >0.05 |
| Hb (gm/dl) | 7.70 ± 0.79 | 7.88 ± 1.72 | 7.71 ± 1.85 | 0.082 | >0.05 |
| Platelets count (× 103/L) | 480.67 ± 376.16 | 444.14 ± 261.47 | 378.26 ± 271.45 | 0.636 | >0.05 |
| MCV (µm3) | 78.67 ± 11.01 | 80.16 ± 6.21 | 77.24 ± 6.28 | 1.845 | >0.05 |
| MCH (pg) | 24.73 ± 2.0 | 28.09 ± 3.13 | 27.42 ± 3.49 | 1.529 | >0.05 |
| RDW (%) | 31.63 ± 2.03 | 34.79 ± 3.05 | 35.52 ± 3.73 | 1.974 | >0.05 |
| Splenectomy Positive No % Negative No % |
3 100% 0 0.0% |
14 45.2% 17 54.8% |
11 26.2% 31 73.8% |
χ2=8.11 | <0.05* |
Table 4: Comparison between rs2228570 genotypes regarding laboratory data, iron related parameter in patients group.
There was a significant association between Ferritin, Alkaline phosphatase, TIBC levels, hepcidin levels and HFE mutation by multivariance regression analysis model.
There were significant differences among AA, AG and GG types of HFE gene (C282Y) mutation as regard number and % of patients with ferritin level equal or more than 2500 ng/ml as index of iron overload group with AA and AG genotypes have significantly higher rates of iron overload than GG genotype (Table 5).
| Ferritin level (ng/ml) |
Patients Group | Total | Chi2 | P value | |||
|---|---|---|---|---|---|---|---|
| AA | AG | GG | |||||
| ≥ 2500 | Number | 3 | 14 | 12 | 29 | 7.12 | <0.05* |
| % | 100% | 45.16% | 28.57% | 38.16% | |||
| <2500 | Number | 0 | 17 | 30 | 47 | ||
| % | 0.0% | 54.84% | 71.43% | 61.84% | |||
| Total | Number | 3 | 31 | 42 | 76 | ||
| % | 100.0% | 100.0% | 100.0% | 100.0% | |||
Table 5: Comparison between SNP of HFE in patients group according to ferritin value as index of iron overload.
Discussion
Multiple transfusions can lead to the accumulation of excessive iron in the body which needs to be corrected using chelating agents to remove excess iron by excretion [15].
Transferrin is a carrier of iron to be soluble in plasma, however when (transferrin saturation. increases over 45%, new circulating iron species can appear, named non-transferrin bound iron (NTBI), which has a very special kinetics in so far as, it targets with very high affinity the parenchymal cells, especially the hepatocytes [16].
The redox potential of tissue iron as environmental modifier may be the cause of chronic liver disease in hemochromatosis [17].
The aim of this study was to evaluate the frequency of rs1800562 HFE mutation in children with beta thalassemia and the correlation between these mutations with parameters of Iron indices including hepcidin levels.
In the present study There was a significantly increased frequency of the A genotype and A allele of HFE gene (C282Y) mutation in children with beta thalassemia compared to controls.
Less commonly two additional mutations were noted other than the C282Y homozygous mutation, aspartate for histidine (H63D) and cysteine for serine (S65C) [18].
The coexistence of two iron metabolism disturbances, beta thalassemia and C282Y mutation in the present study has no explanation but it leads to an additional overload and an increase of oxidative stress in blood cells which may explain the difference of the clinical course between children with beta thalassemia [19].
In accordance to the present study Kaur et al. [20], found that 2 out of 81 patients with beta thalassemia were positive for C282Y rs1800562 mutation. While the studies of Enein et al. [21], Mellouli et al. [22] and Karimi et al. [23], found no cases of this mutation in both patients and control groups.
In the present study there was no significant difference in genotypes of C282Y rs1800562 mutation as regard gender. Matched with this, the study of Katsarou et al. [24] found no association between the HFE polymorphisms rs1800562 and gender could be established.
In the present study in β-thalassemia patients there was a significant increase of serum Iron and ferritin levels in AA genotype than both AG and GG genotypes. Also, there was a significant increase in the splenectomy percent among AA genotype than other two genotypes in the patient group.
A several studies stated elevated serum ferritin concentration as a sensitive indicator of body iron stores with a relationship between C282Y homozygosity and elevated body iron stores [25].
In this study in β-thalassemia patients there was a significant decrease of serum hepcidin levels in AA genotype than both AG and GG genotypes.
In accordance with this study Piperno et al. [26] found that mutations of HFE lead to hepcidin deficiency and the adult form of hereditary hemochromatosis.
In the present study there was a significant increase number and % of patients with ferritin level equal or more than 2500 ng/ml as an index of iron overload with AA and AG genotypes.
Serum ferritin levels of greater than 2500 μg/l are known to have high rates of iron overload-related complications [15]. But individuals with Cys282Tyr homozygosity might present with abnormal iron tests with or without clinical symptoms and with or without proving evidence of iron overload [27].
This can explained by a conformation change in the structure of mutated HFE protein which may prevents the deactivation of transferrin receptor by entering the hepatocyte. So, this receptor will continue to release iron, causing iron overload in the liver [28].
Perhaps liver affection may lead to failure in the production of the liver iron hormone hepcidin in hepatocytes in response to excessive iron absorption from the diet and iron deposition in tissues, causing multiple organ damage and failure [29].
This work shows that as there is a correlation between HFE mutation and hepcidin levels the presence of HFE C282Y mutation may be a predictor of susceptibility to iron overload due to deficiency of hepcidin in Egyptian Beta thalassemia children.
Acknowledgement
We acknowledge the central laboratory unit, faculty of Medicine, Menoufia University for providing us with the necessary instruments for completion of the study.
Ethical Approval
Research involving Human Participants. The study was conducted in accordance with the Declaration of Helsinki. All participants provided written informed consent, and the Ethics Committee of Faculty of Medicine, Menoufia University approved the study protocol.
References
- Chiruka S, Darbyshire P (2011) Management of thalassaemia. Paediatr Child Health 21: 353-356
- Galanello R, Origa R (2010) Beta-thalassemia. Orphanet J Rare Dis 5: 11.
- Taher A, Isma'eel H, Cappellini MD (2006) Thalassemia intermedia: Revisited. Blood Cells Mol Dis 37: 12-20.
- Darshan D, Frazer DM, Anderson GJ (2010) Molecular basis of iron-loading disorders. Expert Rev Mol Med 12: e36
- Zoller H, Koch RO, Theurl I, Koch RO, Vogel W, et al. (2001) Expression of the duodenal iron transporters divalent metal transporter 1 and ferroportin 1 in iron deficiency and iron overload. Gastroenterology 120: 1412-1419.
- Pietrangelo A (2010) Hereditary hemochromatosis: Pathogenesis, diagnosis and treatment. Gastroenterology 139: 393-408.
- Roetto A, Papanikolaou G, Politou M, Alberti F, Girelli D, et al. (2003) Mutant antimicrobial peptide hepcidin is associated with severe juvenile hemochromatosis. Nat Genet 33: 21-22.
- Nemeth E (2010) Hepcidin in beta-thalassemia. Ann N Y Acad Sci 1202: 31-35.
- Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS (2011) Diagnosis and management of hemochromatosis: 2011 practice guideline by the American Association for the Study of Liver Diseases. Hepatology54: 328-343.
- Allen KJ, Gurrin LC, Constantine CC, Osborne NJ, Delatycki MB, et al.(2008) Iron-overload-related disease in HFE hereditary hemochromatosis. N Engl J Med358: 221-230.
- Wood MJ, Skoien R, Powell LW (2009) The global burden of iron overload. Hepatol Int 3: 434-444.
- Young DS, Pestaner LC, Gibberman V (1975) Effects of drugs on clinical laboratory tests. Clin Chem 21: 1D-432D.
- Forman DT, Parke SL (1980) The measurement and interpretation of serum Ferritin. Ann Clin Lab Sci 10: 345-350
- Belhoul KM, Bakir ML, Saned MS, Kadhim AM, Musallam KM, et al. (2012) Serum ferritin levels and endocrinopathy in medically treated patients with thalassemia major. Ann Hematol91: 1107-1114.
- Craven CM, Alexander J, Eldridge M, Kushner JP, Bernstein S, et al.(1987) Tissue distribution and clearance kinetics of non-transferrin-bound iron in the hypotransferrinemic mouse: A rodent model for hemochromatosis. Proc Natl Acad Sci U S A 84: 3457-3461.
- Zoller H, Henninger B (2016) Pathogenesis, diagnosis and treatment of hemochromatosis. Dig Dis 34: 364-373
- European Association for the Study of the Liver (2010) EASL clinical practice guidelines for HFE hemochromatosis. J Hepatol 53: 3-22.
- Fargion S, Sampietro M, Cappellini MD (2000) Thalassemias and their interactions with hemochromatosis. In: Barton JC, Edwards CQ (eds) Hemochromatosis. Cambridge: Cambridge University Press, pp: 435-441.
- Kaur D, Andersen J (2004) Does cellular iron dysregulation play a causative role in Parkinson's disease? Aging Res Rev 3: 327-334.
- Enein AA, El Dessouky NA, Mohamed KS, Botros SKA, El Gawad MFA, et al. (2016) Frequency of Hereditary hemochromatosis (HFE) gene mutations in Egyptian beta thalassemia patients and its relation to iron overload. Open Access Maced J Med Sci 4: 226-231.
- Mellouli F, El Borgi W, Kaabi H, Ben Hassen E, Sassi R, et al. (2006) HFE gene mutations in Tunisian major beta-Thalassemia and iron overload. Transfus Clin Biol 13: 353-357.
- Karimi M, Yavarian M, Delbini P, Harteveld CL, Farjadian S, et al. (2004) Spectrum and haplotypes of the HFE hemochromatosis gene in Iran: H63D in beta-thalassemia major and the first E277K homozygous. Hematol J 5: 524-527.
- Katsaroui MS, Latsi R, Papasavva M, Demertzis N, Kalogridis T,(2016) Population-based analysis of the frequency of HFE gene polymorphisms: Correlation with the susceptibility to develop hereditary hemochromatosis. Mol Med Rep 14: 630-636.
- Gurrin LC, Osborne NJ, Constantine CC, McLaren CE, English DR, et al (2008) The natural history of serum iron indices for HFE C282Y homozygosity associated with hereditary hemochromatosis. Gastroenterology 135: 1945-1952.
- Piperno A, Girelli D, Nemeth E, Trombini P, Bozzini C, et al (2007) Blunted hepcidin response to oral iron challenge in HFE-related hemochromatosis. Blood 110: 4096-4100.
- Stickel F, Buch S, Zoller H, Hultcrantz R, Gallati S, et al (2014) Evaluation of genome-wide loci of iron metabolism in hereditary hemochromatosis identifies PCSK7 as a host risk factor of liver cirrhosis. Hum Mol Genet 23: 3883.
- Ma AD, Udden MM (2007) Iron metabolism, iron overload and the porphyrias. Kahn MJ, Gregory SA. American Society of Hematology Self-Assessment Program. Washington, DC: American Society of Hematology, pp: 61-77.
- Vujic M (2014) Molecular basis of HFE-hemochromatosis. Front Pharmacol 5: 42.
Citation: Badr EAE, Assar MFA, El-Hawy MA, El-dean SRIS, El Sayed IET (2017) Serum Hepcidin Level and Human Factors Engineering (HFE) C282Y Mutation in Egyptian Children with Beta-Thalassemia. Biochem Physiol 6: 223. DOI: 10.4172/2168-9652.1000223
Copyright: © 2017 Badr EAE, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5859
- [From(publication date): 0-2017 - Dec 22, 2025]
- Breakdown by view type
- HTML page views: 4853
- PDF downloads: 1006