Research Article Open Access
Sphincterotomy Related Perforations Diagnosed by CT: Incidence, Risk Factors and Outcome
Michael Shapiro1#, Laurian Copel2#, Dov Abramowich1, Eitan Scapa1, Haim Shirin1* and Efrat Broide1
1The Kamila Gonczarowski Institute of Gastroenterology, Liver Diseases and Nutrition, Assaf Harofeh Medical Center, Sackler Faculty of Medicine, Tel Aviv University,Tel Aviv, Israel
2Department of Diagnostic Imaging, Assaf Harofeh Medical Center, Zerifin 70300, Israel
#Michael Shapiro and Laurian Copel contributed equally to this paper and should therefore be considered first authors.
- *Corresponding Author:
- Haim Shirin, MD
The Kamila Gonczarowski Institute of Institute of Gastroenterology
Liver Diseases and Nutrition
Assaf Harofeh Medical, Center, Zerifin 70300, Israel
Tel: +972-8-9779722
Fax: +972-8-9779727
E-mail: haimsh@asaf.health.gov.il
Received date: April 28, 2015; Accepted date: May 18, 2015; Published date: May 25, 2015
Citation: Shapiro M, Copel L, Abramowich D, Scapa E, Shirin H, et al. (2015) Sphincterotomy Related Perforations Diagnosed by CT: Incidence, Risk Factors and Outcome. J Gastrointest Dig Syst 5:288. doi:10.4172/2161-069X.1000288
Copyright: © 2015 Shapiro M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Duodenal perforation occurring during endoscopic retrograde cholangiopancreatography (ERCP) has been shown to cause high mortality. For assessment the incidence and risk factors of perforation after ERCP and determine the clinical outcome, an abdominal computerized tomography (CT) scan was performed in 180 patients undergoing therapeutic ERCP during three years. Demographic data, type of procedure (classical or pre-cut papillotomy), type of perforation (intra or retroperitoneal), laboratory tests, treatment, and outcome were evaluated.
Retroperitoneal perforation was detected in 21 patients (11.7%). Of these in four patients, perforation was retro and also intraperitoneal. Five patients in the perforation group died, two due to the procedure and three from unrelated causes. Patients who died were older than patients who remained alive. None of the patients with a retroperitoneal perforation underwent surgery, but one died from sepsis. Serum bilirubin levels were significantly higher in patients with perforation. Difficult or unsuccessful cannulation of the CBD and pre-cut papillotomy were found to be risk factors for perforation.
We suggest to perform an abdominal CT soon after therapeutic ERCP in elderly patients with high bilirubin levels in whom the ERCP was difficult or unsuccessful, or pre-cut papillotomy was needed. In patients with a retroperitoneal perforation, closer monitoring for signs of sepsis and/or peritonitis is required.
Keywords
Sphincterotomy; Computerized tomography
Introduction
Of all the gastrointestinal endoscopic interventional techniques, endoscopic retrograde cholangiopancreatography (ERCP) recorded the highest rate of complications with great variability. These include pancreatitis, bleeding, cholangitis and perforations [1,2]. Despite its low incidence, ranging from 0.3% to 1.3%, duodenal perforation occurring during ERCP has been shown to cause high mortality of 16–18% [2-9]. Several classifications of ERCP-related perforations have been published in the medical literature [9,10] and management guidelines based on clinical and radiological criteria have been developed [7-9]. However, the management of ERCP related perforations remains controversial: conservative versus early operative treatment [11,12].
There is no doubt that early and accurate diagnosis of perforations cannot be underestimated. It has been proposed that delayed diagnosis may result in dire outcome [3,7,9]. Abdominal computerized tomography (CT) is considered the best modality for the diagnosis of perforations [13]. In most studies, imaging was performed only in selective cases when a perforation was clinically suspected; either during the procedure or later on when clinical signs of perforation developed.
Our current knowledge regarding the incidence of ERCP related perforations remains scarce. Only two small series reported the results of routine CT examination after therapeutic ERCP. De Vries et al. [14] reported an incidence of 13% ERCP-related perforations (in three out of 24 patients), and Genzlinger et al. [15] reported an incidence of 29% (in six out of 21 patients). Despite the fact that most patients with routine CT-detected perforations had an uneventful course, these two studies with small number of cases do not provide us with any conclusive results for the appropriate management.
The objective of this study was to prospectively evaluate the incidence and risk factors of perforation in all patients undergoing therapeutic ERCP with a low-radiation abdominal CT and to assess the clinical outcome of these patients.
Patients and Methods
Between June 2005 and November 2008, 212 patients were recruited for the study. One hundred and eighty of them, mean age 63.7 years ± 17.7, 100 female, underwent classical or precut papillotomy. Patients younger than18 years of age, pregnant women and patients who were unable or unwilling to provide informed consent were excluded from the study.
Demographic characteristics, co-morbidities, history of upper gastrointestinal (GI) surgery or previous ERCP procedures were collected from all participants. Indications for ERCP and radiological reports were checked and all patients were closely followed until discharged from the hospital. The study was approved by the local ethics committee at our institution.
ERCP
ERCP was performed by four experienced gastroenterologists, with a Pentax Duodenoscope (Tokyo, Japan). Vital signs were checked before, during and after each procedure. In all cases, cannulation of the common bile duct (CBD) was the preferred maneuver and when there was an indication for sphincterotomy, this was done after biliary cannulation and using a guide-wire technique. In those patients where cannulation of the CBD failed, a needle-knife pre-cut papillotomy was performed.
After the procedure was completed, the endoscopist graded the difficulty of the cannulation (grade 1 – easy, grade 2 – moderate and grade 3 – difficult). Access to the biliary tree was documented and clinical suspicion of perforation was recorded.
Diagnostic CT
All patients underwent a low-radiation abdominal CT after a median time of 48 minutes (range: 27 to 360 minutes) post ERCP. All scans were performed with a multi-detector CT (kVP 120, mAs 100) either Philips Brilliance 4 slices with slice thickness of 5.5 mm and slice interval of 5.0 mm (n=73) or 64 slices with slice thickness of 3.0 mm and slice interval of 3.0 mm (n=107) (Philips Medical Systems, MA, USA). No oral or intravenous contrast materials were administered.
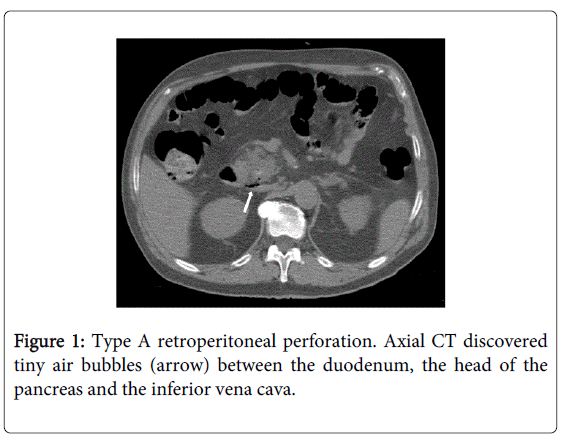
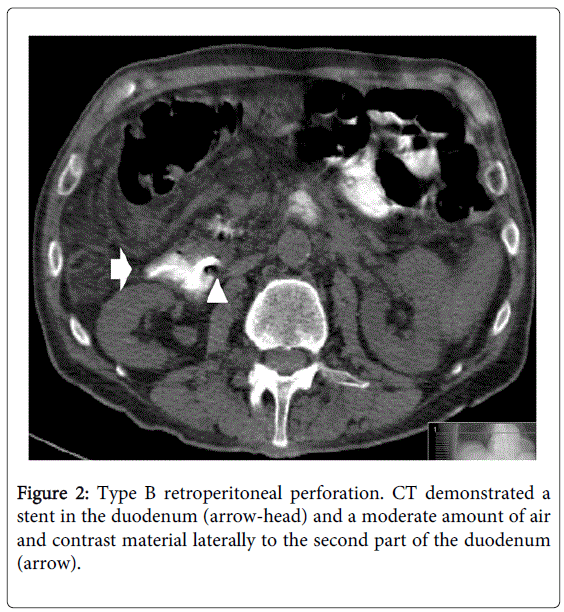
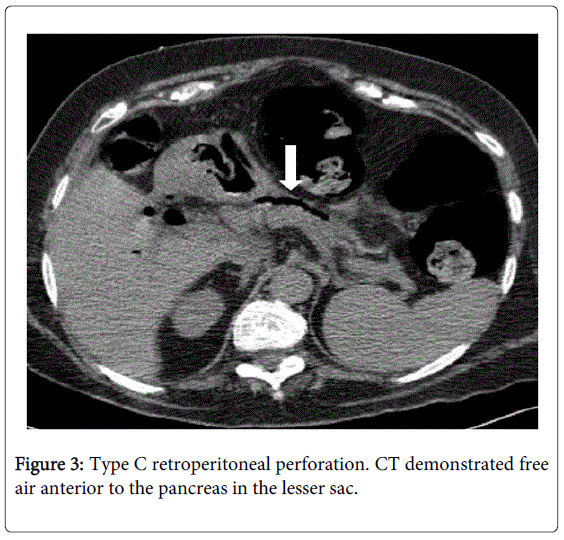
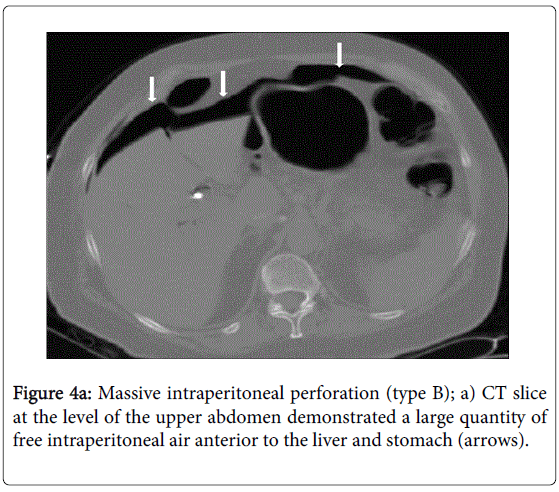
Radiologic definition of perforation was as follows: any leakage of air or contrast material that was injected during the ERCP, regardless of the amount. Types of perforation as diagnosed by CT were classified as retroperitoneal(RPP), intraperitoneal (IPP) or combined. Our classification of RPP was based on a three-point scale: A) the mildest- with ≤5 small air bubbles in close proximity to the duodenum; B) air (>6 air bubbles) or contrast material around the duodenum and C) the most severe- large quantity of air (>6 air bubbles) or contrast material in the retroperitoneum, part of it noted remotely from the duodenum. IPP was classified on a two-point scale: A) ≤3 air bubbles noted in the peritoneal cavity and B) massive air noted in the peritoneal cavity.
Statistical Analysis
Numerical measurements are expressed using means±SD, with medians and ranges. Categorical measurements are expressed using percentages. Comparisons of sub-groups of patients with and without perforations included: 1) an independent t-test and the non-parametric Mann-Whitney test for the numerical data and 2) the chi-square test or Fisher's exact test for the categorical data. A multivariate logistic regression model was used in order to find out factors influencing perforation. A stepwise logistic regression analysis was conducted. All analyses were done using SPSS 14.01 statistical software (SPSS Inc., IBM Corp., NY, USA) A P value <0.05 was considered statistically significant.
Results
A perforation was diagnosed by CT in 21 patients (11.66%): 17 patients (9.44%) had a RPP and four (2.22%) had a combined intra and RPP. No statistically significant differences between patients with or without a perforation were found regarding the indications for ERCP (Table 1), associated co-morbidities, cholelithiasis, previous cholecystectomy or other upper GI operations (Table 2). Approximately 50% of the patients underwent therapeutical ERCP for CBD stones and 24% for unexplained dilated CBD. Although not significantly a duodenal diverticulum tended to be more frequent in patients with a perforation than in those without (23.8% vs. 15.7%, respectively).
| Variables | All patients | Without perforation | With perforation, | P value |
|---|---|---|---|---|
| n=180 | n=159 (88.3%) | n=21 (11.7%) | ||
| Indications | ||||
| Common bile duct stones | 94 (52.2) | 84 (52.8) | 10 (47.6) | 0.095 |
| Pancreatitis | 7 (3.9) | 7 (4.4) | 0 (0) | |
| Ca of pancreas/papilla | 14 (7.8) | 11 (7.0) | 3 (14.3) | |
| Dilated common bile duct | 44 (24.4) | 38 (23.9) | 6 (28.6) | |
| Cholangitis | 14 (7.8) | 13 (8.2) | 1 (4.8) | |
| Cholangiocarcinoma | 1 (0.6) | 0 | 1 (4.8) | |
| Common bile duct leak | 6 (3.3) | 6 (3.8) | 0 (0) | |
| Papillotomy | 125 (69.4) | 119 (74.8) | 6 (28.6) | <0.001 |
| Pre-cut | 55 (30.6) | 40 (25.2) | 15 (71.4) | |
| Stentingyes | 55(30.6) | 48 (30.2) | 7 (33.3) | 0.803 |
| no | 125 (69.4) | 111 (69.8) | 14 (66.7) | |
| Accessyes | 153 (85) | 141 (88.7) | 12 (57.1) | 0.001 |
| no | 27 (15) | 18 (11.3) | 9 (42.9) | |
| Difficulty | ||||
| Easy | 78 (43.3) | 74 (46.5) | 4 (19.0) | |
| Moderate | 47 (26.1) | 42 (26.4) | 5 (23.8) | 0.004 |
| Difficult | 25 (13.9) | 17 (10.7) | 8 (38.1) | |
| Impressionyes | 8 (4.4) | 3 (1.9) | 5 (23.8) | <0.001 |
| no | 140 (77.8) | 128 (80.5) | 12 (57.1) | |
| Diverticulum yes | 30 (16.7) | 25 (15.7) | 5 (23.8 ) | 0.355 |
Table 1: ERCP variables, results are shown as: n (%).
| Comorbidities, n (%) | All patients n=180 |
Without perforation n=159 |
With perforation n=21 |
P value |
|---|---|---|---|---|
| IHD | 44 (24.4 ) | 38 (23.9 ) | 6 (28.6) | 0.600 |
| COPD | 9 (5.0) | 8 (5.0) | 1 (4.8) | 1.000 |
| Other* | 46 (25.6) | 41 (25.8) | 5 (23.8) | 1.000 |
| Cholelithiasis | 99 (55 0) | 90 (56.6) | 9 (42.9) | 0.252 |
| Cholecystectomy | 55 (36 0) | 50 (31.4) | 5 (23.8) | 0.617 |
| Previous ERCP | 39 (21.7) | 34 (21.4) | 5 (23.8) | 0.782 |
| Previous papillotomy | 24 (13.3) | 22 (13.8) | 2 (9.5) | 0.743 |
Table 2: Patient characteristics, IHD, ischemic heart disease; COPD, chronic obstructive pulmonary disease, *Diabetes mellitus, chronic renal failure, malignancy.
We found that the pre-cut technique was associated with a significantly higher rate of RPP compared to classical papillotomy (P < 0.001). Fifteen out of 21 patients (71.4%) with a perforation underwent pre-cut papillotomy in contrast to 40 out of 159 patients (25.2%) without a perforation. In patients with a perforation, no biliary access was achieved in 42.9% and in 38.1% the procedure was graded as difficult in comparison to 11.3% (P=0.001) and 10.7% ( P=0.004) respectively in patients without perforations.
In addition, in the group of patients with a perforation, 23.8% of the perforations were suspected by the gastroenterologist during the procedure, versus only 1.9% in the group of patients without perforations (P<0.001). No significant difference was found in the rate of perforations among the four endoscopists that took part in this study.
Imaging Findings
There was no case where a perforation was not detected in the initial CT study but diagnosed during the follow-up CT study. Among 17 patients with RPP, the findings were as follows: six patients (35.3%) had a type A (Figure 1), six patients (35.3%) a type B (Figure 2), and five patients (29.4%) had a type C perforation (Figure 3).
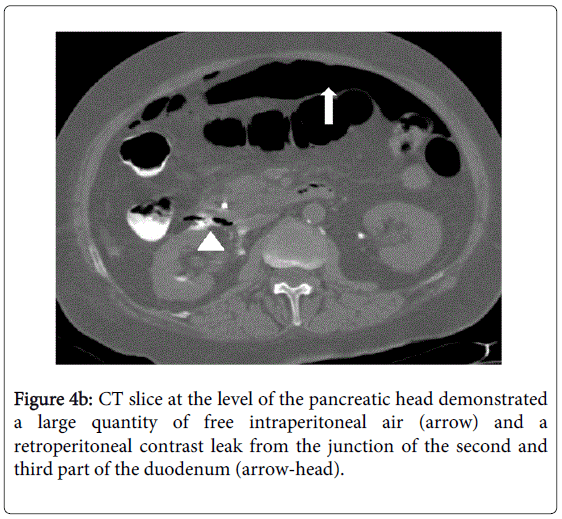
In four patients, an intra and extraperitoneal perforation was found. Three of them had type B IPP with massive intraperitoneal air (Figures 4a and 4b) and in one patient only a minimal quantity of air was found in the intraperitoneal cavity defined as type A IPP perforation. All patients with IPP also had a large quantity of retroperitoneal air (type C RPP).
Laboratory Findings
There were no significant differences between the two groups except in the levels of bilirubin. Total and direct bilirubin before ERCP were significantly higher in patients with post ERCP perforation [total bilirubin 5.4 ± 5.5 4 mg/dL (4.0; 0.3-37.8); direct 4.4 ± 4.14 mg/dL (3.3; 0-23) in patients without perforation compared to 9.9 ± 7.54 mg/dL (14.4; 0.4-23.2) and 8.3 ± 5.84 mg/dL (6.9; 0-17) in those with perforation (P=0.001). The total bilirubin level decreased 24 hours after ERCP from 5.4 mg/dL to 4.6 mg/dL in patients without perforations, and increased from 9.9 mg/dL to 10.4 mg/dL in those with perforations (P=0.027).
Clinical Management and Mortality
Blood pressure, heart rate and oxygen saturation were not significantly different between patients with or without perforation, before and after papillotomy. All patients with a perforation were treated conservatively by fasting and the administration of nasogastric tube, IV fluids and antibiotics. Worsening abdominal pain, leukocytosis or sepsis led to surgery. None of the patients with a RPP underwent surgery, regardless of the type of perforation. Two out of four patients with an IPP underwent surgery due to signs of peritonitis.
One patient out of 159 patients without perforations died from post ERCP pancreatitis. Overall, in the group of patients with perforations, five patients died. Of these two patients died from direct ERCP-related causes, and three from indirect ERCP related complications. Three of the patients had RPP and two patients had combined IPP and RPP (Table 3). One the patients developed sepsis with no abdominal tenderness on the fifth day after the ERCP. A second CT scan (this time with IV contrast material administration) demonstrated a retroperitoneal abscess. She was treated conservatively, but died from sepsis 20 days later. Two other patients died from causes unrelated directly to the perforation such as MI and pancreatic cancer. Two out of four patients with combined perforation died, one after surgery and the other, who was treated conservatively, due to pulmonary edema.
| Patient | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| Age | 80 | 87 | 74 | 88 | 84 |
| Type of perforation | RPP | RPP | RPP | Combined | Combined |
| Treatment | Conservative | Conservative | Conservative | Surgery | Conservative |
| Cause of death | ERCP | MI | PC | ERCP | CHF |
Table 3: Deceased patients in the perforation group. RPP; retroperitoneal perforation, IPP; intraperitoneal perforation, CHF: Congestive heart failure; MI :myocardial infarction, PC: pancreatic cancer.
Patients who died were significantly older than those that stayed alive 59.9 ± 14.6 (63.5; 21-81) years vs. 82.6 ± 5.7 (84; 74-88) years and this difference was significant despite a small cohort size (Kruskal-Wallis test with a P value of 0.003). There was no difference in the rate of comorbidities, values of laboratory tests, cannulation difficulty grade, access to the biliary tree or clinical suspicion of perforation.
Multivariate Logistic Regression Analyses
Multivariate logistic regression analyses were performed using all the significant and some of the non-significant perforation factors that were received from univariate analysis (Table 4). After using the stepwise method, only three factors were found to have a significant risk effect on perforation: lower aspartate aminotransferase (AST) level before the procedure, pre-cut papillotomy and the endoscopist's impression.
| Variables in the equation | OR (95% CI) | P value | |
|---|---|---|---|
| Step 1 | Gender | 1.86 (0.13-25.98) | 0.645 |
| Age | 0.91 (0.83-1.01) | 0.067 | |
| Previous ERCP | 3.52 (0.12-105.17) | 0.468 | |
| Previous Papillotomy | 0.25 (0.00-60.07) | 0.618 | |
| Bilirubin level | 0.43 (0.17-1.06) | 0.067 | |
| AST | 0.99 (0.95-1.02 | 0.449 | |
| ALT | 1.00 (0.98-1.03 | 0.694 | |
| ALP | 1.00 (0.98-1.02 | 0.956 | |
| Dilated CBD | 0.86 (0.00-457.4) | 0.963 | |
| CBD diameter | 0.88 (0.57-1.34) | 0.537 | |
| Diverticulum | 0.72 (0.02-30.7) | 0.866 | |
| Pre-cut | 13.99 (0.36-543.5) | 0.158 | |
| Difficulty | 1.93 (0.09-42.7) | 0.677 | |
| Access | 0.53 (0.03-11.3) | 0.687 | |
| Impression | 1731.7 (7.00-428253.1) | 0.008 | |
| Endoscopist | 21.00 (0.47-942.3) | 0.116 | |
| Gender | 1.86 (0.13-25.98) | 0.645 | |
| Variables in the equation | OR (95% CI) | P value | |
| Step 20 | AST | 0.98 (0.97-0.99) | 0.009 |
| Pre-cut | 14.61 (3.15-67.77) | 0.001 | |
| Impression | 43.43 (3.10-609.06) | 0.005 | |
Table 4: Risk factors for perforation by multivariate stepwise logistic regression. ALT: alanine aminotransferase; ALP: alkaline phosphatase; AST: aspartate aminotransferase; CBD common bile duct.
Discussion
Our results, with the largest cohort of patients published until now, indicate that the actual incidence of all types of ERCP-related perforations (symptomatic, asymptomatic, RPP and IPP) is high- 11.66% (9.44% RPP and 2.22% IPP). We also identified exclusively increased RPP rate in patients who underwent pre-cut because of difficult and unsuccessful cannulation of the biliary tree and in patients with high bilirubin levels (total and direct). These results are consistent with previous reports, that also showed high (13% and 29%) post ERCP asymptomatic perforation rates [14,15] although recent meta-analysis suggests that pre-cut sphincterotomy and persistent attempts at cannulation are comparable in terms of overall complication rates [16].
Usually, a perforation is suspected by the endoscopist during or after the procedure based on leakage of contrast material from the duodenum or the biliary tree, clinical signs and symptoms such as abdominal pain, leukocytosis, or sepsis. In many centres, special attention is paid to this risk by making a plan abdominal X-ray as the last step of the procedure after sphincterotomy. Consequently, in the large majority of cases with symptomatic RPP this complication is detected during the procedure [17]. However, the clinical significance of asymptomatic perforation is not entirely clear. The consensus in the last two decades assume that type II and III injuries mostly, tend to seal spontaneously and thus lend themselves to nonsurgical management [10,18]. Moreover, Genzingler et al. hypothesized that retroperitoneal air alone (type IV) is probably related to the use of compressed air to maintain patency of a lumen [15]; as such, it is not a true perforation and thus does not require surgical intervention. Indeed only lateral or medial wall perforations (type I) that are caused by the endoscope, tend to be large and require immediate surgery [19].
Nevertheless, by contrast to previous studies suggesting that RPP has little clinical significance [20], two patients with asymptomatic RPP in our study died from indirect causes, compared to none in the group of patients without a perforation. Three patients (1.7%) in our series died from direct ERCP-related complications: two from the perforation group and one from the "non perforation" group. Three additional patients died from indirect causes, and all three were in the perforation group. Four of the dead were octogenarians and old age was the only significant factor that differed between the patients with perforation who died and those who survived. As previously emphasized post ERCP cardiopulmonary complications are significantly higher in patients older than 65 years compared with younger than 65 [21]. Therefore we assume that the significance of perforation probably sprawls beyond local inflammation. It might be speculated that stress concerning the procedure, inflammatory mediator secretions related indirectly to the procedure and systemic complications may be involved in their death.
We believe that early diagnosis of perforations is crucial for proper treatment of patients after therapeutic ERCP. Moreover, early abdominal CT would enable early diagnosis of IPPs regardless of clinical signs. We demonstrated that CT can be performed immediately after therapeutic ERCP with no need for preparation (oral or intravenous contrast material). In our study CT diagnosed all of the ERCP-related perforations on the initial early scan with no additional diagnosis of perforation on a follow-up examination. We did not use the classification that was introduced by Stapfer and colleagues [10]. They made a diagnosis during the ERCP or performed imaging tests (usually upper GI swallowing) only in patients in whom perforation was suspected clinically. We used our own classification based on CT findings and found it to be a simple and useful tool for the clinician.
In addition, in this prospective study we evaluated the risk factors of such perforations. We knew that pre-cut papillotomy and failed CBD cannulation are both associated with an increased complication rate [1,2,4] such as bleeding, pancreatitis and symptomatic perforation. By using logistic regression multivariate analysis, pre-cut papillotomy and the endoscopist's suspicions were identified as risk factors for perforation Interestingly, a higher AST level before the procedure was found to be a protective factor.
We are aware that our study has several limitations. The rate of perforations, including clinically significant and even fatal ones, was high compared to the literature [22]. The volume of ERCP procedures during the years of the study was relatively small. Freeman et al. have already shown, that complications of ERCP, especially severe ones, are related to the volume of procedures peformed by the endoscopist [23]. This also may explain the exceedingly high rate of pre-cut papillotomy (31%) among our patients requiring sphincterotomy. Despite this, our current incidence of perforations on CT was less than those of De Vries et al. (13%) and Genzlinger et al. (29%) [14,15]. Finally, our surgeons were not blinded to the result of the CT due to ethical reasons. However, this did not alter the treatment modality or the clinical course as only conservative treatments were applied for these patients.
In conclusion, based in our findings we suggest to perform an abdominal CT soon after therapeutic ERCP in elderly patients with high bilirubin levels in whom the ERCP was difficult or unsuccessful, or pre-cut papillotomy was needed. In patients with a RPP, closer monitoring for signs of sepsis and/or peritonitis is required.
References
- ASGE Standards of Practice Committee, Anderson MA, Fisher L, Jain R, Evans JA, et al. (2012) Complications of ERCP. Gastrointest Endosc 75: 467-473.
- Glomsaker T, Hoff G, Kvaløy JT, Søreide K, Aabakken L, et al. (2013) Patterns and predictive factors of complications after endoscopic retrograde cholangiopancreatography. Br J Surg 100: 373-380.
- Mao Z, Zhu Q, Wu W, Wang M, Li J, et al. (2008) Duodenal perforations after endoscopic retrograde cholangiopancreatography: experience and management. J Laparoendosc Adv Surg Tech A 18: 691-695.
- Fatima J, Baron TH, Topazian MD, Houghton SG, Iqbal CW, et al. (2007) Pancreaticobiliary and duodenal perforations after periampullary endoscopic procedures: diagnosis and management. Arch Surg 142: 448-454.
- Enns R, Eloubeidi MA, Mergener K, Jowell PS, Branch MS, et al. (2002) ERCP-related perforations: risk factors and management. Endoscopy 34: 293-298.
- Jin YJ, Jeong S, Kim JH, Hwang JC, Yoo BM, et al. (2013) Clinical course and proposed treatment strategy for ERCP-related duodenal perforation: a multicenter analysis. Endoscopy 45: 806-812.
- Avgerinos DV, Llaguna OH, Lo AY, Voli J, Leitman IM (2009) Management of endoscopic retrograde cholangiopancreatography: related duodenal perforations. Surg Endosc 23: 833-838.
- Wu HM, Dixon E, May GR, Sutherland FR (2006) Management of perforation after endoscopic retrograde cholangiopancreatography (ERCP): a population-based review. HPB (Oxford) 8: 393-399.
- Howard TJ, Tan T, Lehman GA, Sherman S, Madura JA, et al. (1999) Classification and management of perforations complicating endoscopic sphincterotomy. Surgery 126: 658-663.
- Stapfer M, Selby RR, Stain SC, Katkhouda N, Parekh D, et al.(2000) Management of duodenal perforation after endoscopic retrograde cholangiopancreatography and sphincterotomy. Ann Surg 232: 191-198
- Sarli L, Porrini C, Costi R, Regina G, Violi V, et al. (2007) Operative treatment of periampullary retroperitoneal perforation complicating endoscopic sphincterotomy. Surgery 142: 26-32
- Booth FV, Doerr RJ, Khalafi RS, Luchette FA, Flint LM Jr (1990) Surgical management of complications of endoscopic sphincterotomy with precut papillotomy. Am J Surg 159: 132-135.
- Zissin R, Shapiro-Feinberg M, Oscadchy A, Pomeranz I, Leichtmann G, et al. (2000) Retroperitoneal perforation during endoscopic sphincterotomy: imaging findings. Abdom Imaging 25: 279-282.
- De Vries JH, Duijm LE, Dekker W (1997) CT before and after ERCP: detection of pancreatic pseudotumor, asymptomatic retroperitoneal perforation, and duodenal diverticulum. Gastrointest Endosc 45: 231-235.
- Genzlinger JL, McPhee MS, Fisher JK, Jacob KM, Helzberg JH (1999) Significance of retroperitoneal air after endoscopic retrograde cholangiopancreatography with sphincterotomy. Am J Gastroenterol 94: 1267-1270.
- Navaneethan U, Konjeti R, Venkatesh PG, Sanaka MR, Parsi MA (2014). Early precut sphincterotomy and the risk of endoscopic retrograde holangiopancreatography related complications: An updated meta-analysis. World J Gastrointest Endosc 6: 200-208.
- Li G, Chen Y, Zhou X, Lv N (2012) Early management experience of perforation after ERCP. Gastroenterol Res Pract 2012: 657418.
- Norman Oneil Machado (2012) Management of duodenal perforation post-endoscopic retrograde cholangiopancreatography. When and whom to operate and what factors determine the outcome? A review article. J Pancreas 13: 18-25.
- Kwon CI, Song SH, Hahm KB, Ko KH (2013) Unusual complications related to endoscopic retrograde cholangiopancreatography and its endoscopic treatment. Clin Endosc 46: 251-259.
- Kodali S, Mönkemüller K, Kim H, Ramesh J, Trevino J, et al. (2015) ERCP-related perforations in the new millennium: A large tertiary referral center 10-year experience. United European Gastroenterol J 3: 25-30.
- Fisher L, Fisher A, Thomson A (2006) Cardiopulmonary complications of ERCP in older patients. Gastrointest Endosc 63: 948-955.
- Morgan KA, Fontenot BB, Ruddy JM, Mickey S, Adams DB (2009) Endoscopic retrograde cholangiopancreatography gut perforations: when to wait! When to operate! Am Surg 75: 477-483.
- Freeman ML, Nelson DB, Sherman S, Haber GB, Herman ME, et al. (1996) Complications of endoscopic biliary sphincterotomy. N Engl J Med 335: 909-918.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15793
- [From(publication date):
June-2015 - Aug 02, 2025] - Breakdown by view type
- HTML page views : 11143
- PDF downloads : 4650