Stage II/A Flatfoot Correction Using Triple Combination
DOI: 10.4172/2329-910X.1000321
Abstract
Background: To The aim of this study is to assess the correction of adult Stage II/A flexible flatfoot deformity using a combination of gastrocnemius aponeurosis lengthening, arthroereisis and percutaneous medializing calcaneal osteotomy.
Methods: From 2014 to 2018, data were collected on 35 feet over 31 patients, with 4 bilateral cases, who underwent this combination technique. The average age of the patients was 37 years. Inclusion criteria were Stage II/A flexible flatfoot, whereas the exclusion criteria were other Stages of flatfoot, rigid flatfoot, synostoses and flatfoot with congenital and neurological malformation. We used the lateral and anteroposterior talocalcaneal angles as well as medial arch angle and talo-first metatarsal angle measurements to assess efficacy of our technique. All data were analyzed statistically with Student’s t test.
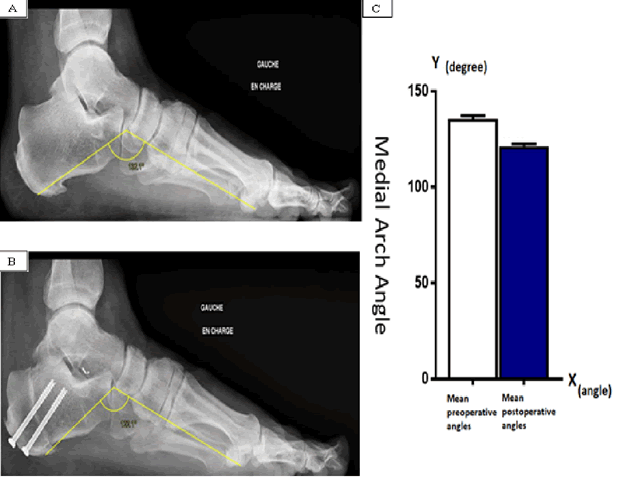
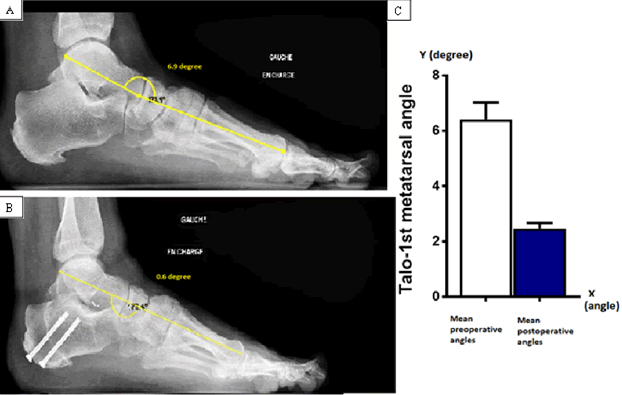
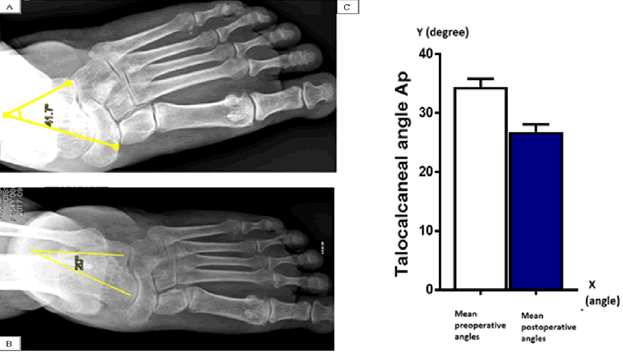
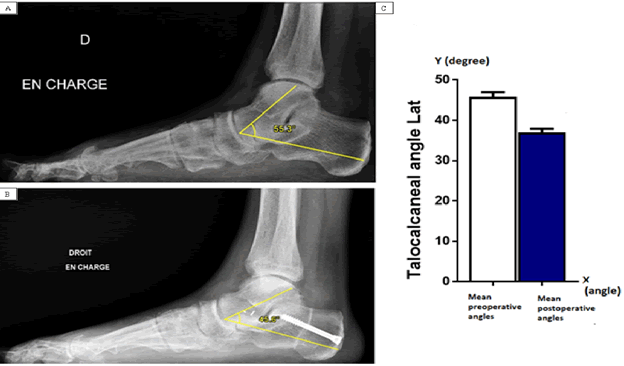
Results: The mean values of the preoperative and postoperative weightbearing radiographic angles are 137° vs 123° for the Medial Arch Angle, 8° vs 3° for the Talo-first metatarsal angle, 34° vs 27° for the anteroposterior Talocalcaneal divergence angle and 42° vs 39° for the lateral Talocalcaneal divergence angle (p<0.001). In 33 of 35 feet (94%) the results we observed show the improvement of radiographic measurements as well as normal foot function at 6 months. Mean follow up time was 37 months. American Orthopedic Foot and Ankle Society (AOFAS) scores were calculated for all patients, and based on final results; it showed improvement on the 3 scales of pain, function and alignment.
Conclusion: Based on the literature and on our statistical results we find that combining gastrocnemius aponeurosis lengthening with arthroereisis and percutaneous medializing calcaneal osteotomy is an optimal surgery for the correction of Stage II/A flexible flatfoot.
Keywords: Arthroereisis; Percutaneous; Calcaneal Osteotomy; Gastrocnemius lengthening
Abbreviations
American Orthopedic Foot and Ankle Society (AOFAS); Anteroposterior (AP); Flexor Digitorum Longus (FDL); Posterior Tibial Tendon Deficiency (PTTD)
Introduction
Adult flexible flatfoot is defined as a weight bearing flattening of the medial arch of the foot in addition to plantar flexion of the talus [1]. The posterior tibial tendon dysfunction is the most common factor leading to development of flatfoot [2]. The pull of the Achilles tendon falls lateral to the axis of the subtalar joint creating excessive hindfoot valgus [2]. Over time, static stabilizers of the medial foot like spring ligament becomes attenuated [3].
Stage I PTTD consists of a painful synovitis but no deformity as the tendon has a normal function. Stage II/A describes progressive failure of the tendon with a flexible flatfoot deformity, which is correctable passively, with mild sinus tarsi pain whereas in Stage II/B talonavicular uncoverage is >40% in addition to the presence of forefoot abduction. In Stage III, the deformity is rigid with degenerative changes in the midfoot and hindfoot [4]. Finally, stage IV describes valgus tilting of the talus within the ankle mortise with associated deltoid insufficiency, with or without tibiotalar arthritis [5].
We performed physical exam to determine flexibility and deformity of Stage II/A and assess any deficits of posterior tibial tendon or spring ligament [1]. In Flexible Flatfoot we will encounter inversion loss or eversion caused by subtalar or Chopart’s joint dysfunction or PTTD [6]. The posterior tibial tendon is involved when the foot is everted; reduced active inversion may suggest spring ligament lesion [6]. The too many toes sign is a result of forefoot abduction and is included in Stage II/B deformity; Hallux Valgus is an associated finding in Flatfoot deformity [3]. Flatfoot is considered pathological when it is symptomatic; Pain is often located medially along the course of the posterior tibial tendon or at the plantar aspect that suggests attrition over the spring ligament. Lateral pain might be due to severe tibiotalar valgus deformity causing fibulocalcaneal impingement.
Many combination surgeries are used to address flexible flatfoot with debates over the years about the efficacy and longevity and limited recurrence of each including lateral column procedures which carry the risk of arthritis at the calcaneocuboid joint and flexor digitorum longus tendon transfer which can fail and lead to recurrence [7]. The percutaneous medializing calcaneal osteotomy corrects the hindfoot valgus by translating the calcaneal tuberosity medially realigning the Achilles tendon and reduces skin complications [8]. Medializing calcaneal osteotomy after 5 years of follow up, showed 91% of patient satisfaction [9].
Arthroereisis or sinus tarsi implant is used to reduce talonavicular divergence and correct hindfoot valgus by applying a conical implant in between the anterior apophysis of the calcaneus and the reduced lateral process of the talus [10]. Gastrocnemius muscle retraction is also an associated factor leading to hindfoot valgus; thus, gastrocnemius aponeurosis lengthening is an added technique to further realign the hindfoot [11]. We reviewed the literature and we opted to combine percutaneous medializing calcaneal osteotomy, arthroereisis and gastrocnemius aponeurosis lengthening to deal with stage II/A flatfoot addressing its deformities with minimal complications and without medial soft tissue repair.
Methods
Data collection
Between 2014 and 2018, data on 31 non-athlete patients were collected (4 patients treated bilaterally) 18 women and 13 men, with mean BMI of 27.2 kg/m2 who underwent percutaneous correction of flexible adult flatfoot at the Hôpitaux Civils de Colmar France using a combination of three procedures: Gastrocnemius aponeurosis lengthening, arthroereisis and percutaneous medializing calcaneal osteotomy. The inclusion criteria of this study were adult flexible flatfoot Stage II/A. In this study we used 4 angles to assess the flatfoot deformity preoperatively and postoperatively, the lateral and AP angles of the Talocalcaneal divergence which refers to the angle between lines drawn down the long axis of the talus and calcaneus measured on a weight bearing AP and lateral foot radiography, Lateral (normal values between 30°-50°) and AP (normal values between 20°-30°), along with Talo-first metatarsal Angle comprising the angle between the longitudinal axis of talus and that of first metatarsal bone on weight bearing lateral foot radiography (Normal Values Between 0°-4°) and Medial Arch Angle that is formed by three specific points in the standing patient: the lower point of the calcaneus, the lower point of the talus-navicular joint and the impact point of the medial sesamoid bone (normal values between 120°-130°) at a lateral foot radiography [1,2,7] . This is a retrospective single centre study that was conducted on a total of 35 feet in 31 patients between the ages of 29 years and 55 years with an average length of follow up to 37 months. All patients have the clinical diagnosis of adult flexible flatfoot Stage II/A; we excluded patients with rigid flatfoot, tarsal coalitions, congenital or neurological malformation. At our medical institution, the clinical assessment of a patient with flatfoot consists of a medical examination of the foot and radiography measurements and AOFAS ankle-Hindfoot score.
Surgical technique
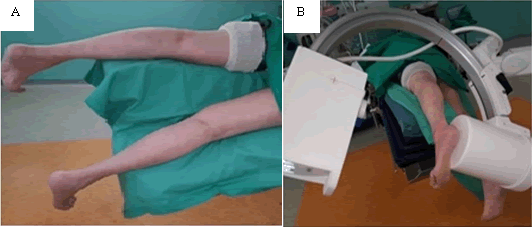
Patient lied in prone position with the foot free. Tourniquet placed at the thigh inflated at 100 mmHg above the systolic blood pressure. C arm placed properly to obtain true AP and lateral views and wrapped with sterile plastic coverage (Figure 1).
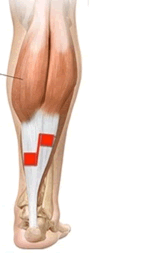
Sterile prepping and draping of the foot. Next, a 3 cm midline incision was performed over the posterior aspect at the middle third of the leg and a Z plasty of the gastrocnemius aponeurosis to induce lengthening (Figure 2).
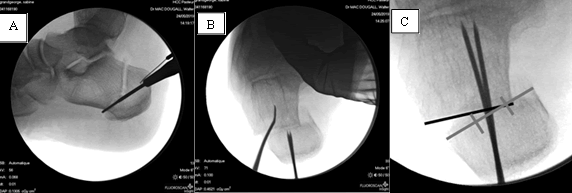
Then we performed medializing calcaneal osteotomy via a percutaneous chevron osteotomy (Figure 3A).
Additionally, we performed a slight medial rotation of the posterior calcaneal fragment and medial translation of not more than one third of calcaneal width for further correction about 10 mm (Figures 3B and 3C). We fixed it with 2 short threaded 6.5 mm cannulated screws.
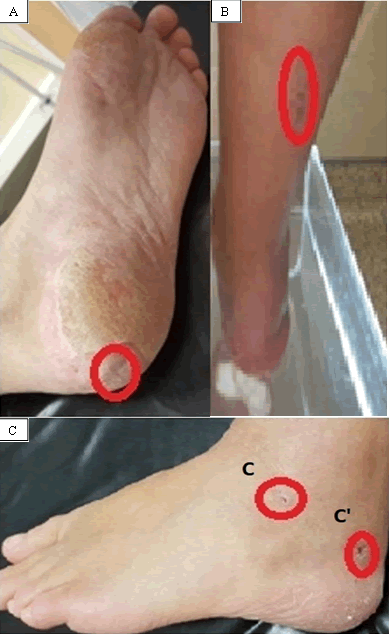
At last, we performed arthroereisis via a lateral percutaneous approach under radiographic guidance, the size of sinus tarsi implant is chosen according to the fit of the implant inside the sinus tarsi joint, the implant being conical in shape and lock the talocalcaneal joint in a reduced state and furthermore aids in talonavicular coverage (Figure 4).
Figure 4: A) Axial A Postero-Inferior Incision for Calcaneal Osteosyntesis. B) Incision for Gastrocnemius Aponeurosis Lengthening at the Posterior Distal Third of the Leg. C) Laternal Incision at the Level of Sinus Tarsi for Arthroereisis. 2-C’ Laternal Incision for the Percutaneous Calcaneal Osteotomy.
Postoperative management involved protected non-weight bearing in a cast in a neutral position for 2 weeks. Emphasis was placed on postoperative elevation of the limb to minimize the inevitable swelling that results after surgery. Touchdown weight bearing in a cast continues for an additional 4 weeks. Weight bearing radiographs were obtained at 8 weeks postoperatively to assess correction and alignment. The patient was encouraged to begin regular shoe wear after 12 postoperative weeks.
Statistical analysis
Experimental data were analyzed using “GraphPad Prism 6“(La Jolla, CA, USA). Data were presented as mean ± SEM. All groups of the data were firstly assessed for normal distribution (using the Kolmogorov– Smirnov test) with outliers excluded. Comparison between two groups was performed using a two tailed unpaired t-test for normal distributed data or a” Mann–Whitney U-test “for nonparametric data. All data sets were significant with p value < 0.0001 . All data were analyzed statistically with “Student’s t test”.
Results
In order to assess the correction of flexible adult flatfoot deformity, we measured the mean values of the preoperative and postoperative weight bearing radiography angles as well as the AOFAS scores.
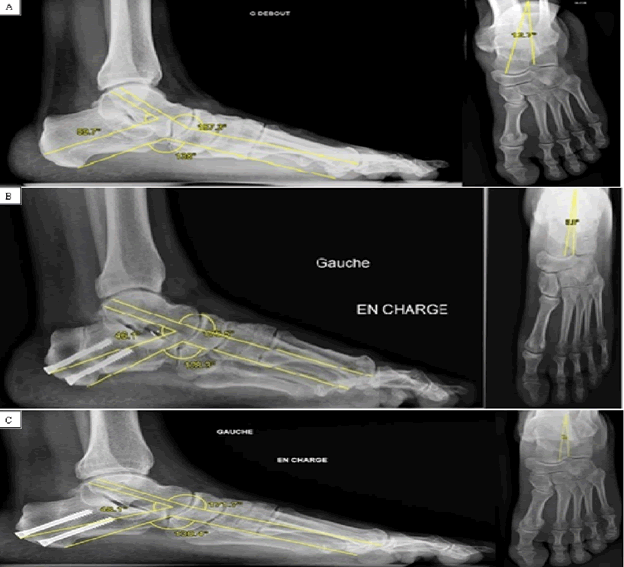
The medial arch angle was reduced postoperatively with measured values seen in (Figure 5). A significant decrease was observed for the talofirst metatarsal angle (Figure 6). The AP talocalcaneal divergence angle was also reduced (Figure 7). Finally, a significant statistical difference between the preoperative and postoperative lateral Talocalcaneal divergence angle (p<0.001) (Figure 8). In all of the studied cases, the results were back within normal radiographic ranges (Table 1) as well as normal postoperative foot function; pain and alignment according to the AOFAS hind foot score (Table 2).
Figure 6: A) Preoperative Tarso-1st Metatarsal Angle Measurement on a Laternal Ankle Plain Radiograph. B) Postoperative Tarso-1st Metatarsal Angle Measurement on a Laternal Ankle Plain Radiograph. C) Results of the Mean Distribution of the Tarso-1st Metatarsal Angle Preoperatively and Postoperatively.
Figure 7: A) Preoperative Talocalcaneal Divergence Angle Measurement on an Anteroposterior Ankle Plain Radiograph. B) Postoperative Talocalcaneal Divergence Angle Measurement on an Anteroposterior Ankle Plain Radiograph. C) Results of the Mean Distribution of the Talocalcalneal Divergence Angle Preoperatively and Postoperatively.
Figure 8: A) Preoperative Talocalcaneal Divergence Angle Measurement on an Anteroposterior Ankle Plain Radiograph. B) Postoperative Talocalcaneal Divergence Angle Measurement on an Anteroposterior Ankle Plain Radiograph. C) Results of the Mean Distribution of the Talocalcalneal Divergence Angle Preoperatively and Postoperatively.
| Angle | Preoperative | Postoperative | Mean difference ± SEM |
|---|---|---|---|
| Medial arch angle | 135 ± 2 | 121 ± 1 | 14± 1 |
| Talo-first metatarsal Angle | 6 ± 1 | 2 | 4 |
| AP Talocalcaneal angle | 34 ±1 | 27 ± 1 | 8 ± 1 |
| lateral Talocalcaneal angle | 46 ± 1 | 37 ± 1 | 9 ± 1 |
Table 1: Mean radiographic preoperative and postoperative measured angles result with their mean difference and standard error of the mean SEM.
| Result | Preoperative | Postoperative | Mean difference ± SEM |
|---|---|---|---|
| AOFAS score | 48 ± 8 | 78 ± 6 | 29 ± 6 |
Table 2: Mean clinical preoperative and postoperative AOFAS score result with it is mean difference and standard error of the mean SEM.
Discussion
PTTD classification has evolved more details in order to clarify treatment recommendations.
There is an emphasis on the early diagnosis of Stage II/A in order to initiate treatment while the deformity is still flexible. Our work is to combine three surgical techniques in order to correct the flexible flatfoot. Surgical management combines multiple techniques to correct deformities in the hindfoot, midfoot and forefoot.
In our study we combined gastrocnemius aponeurosis lengthening along with percutaneous medializing calcaneal osteotomy and arthroereisis in 35 feet of 31 patients followed from 2014 till 2018 and gave satisfactory postoperative results with significant differences P<0.005 on Student’s t test between four preoperative and postoperative angles studied which are the AP and lateral Talocalcaneal angles, Medial Arch Angle and Talofirst metatarsal angles as well on AOFAS.
Advances in bracing and orthotics reveal a further understanding of the deforming forces present in flexible flatfoot. Approximately 80% of early PTTD (stage I and IIA/B) respond well to non-operative management [11]. The rationale behind that is to alleviate forces transmitted through the posteromedial hindfoot, thereby preventing medial collapse of the foot. Lifestyle modification such as weight lost is also encouraged.
The treatment of Stage I flexible flatfoot may include open or endoscopic tendon debridement [12,13] or tenosynovectomy [14,15]. According to a review of literature [16] nine patients with flexible flatfoot underwent tenosynovectomy with or without repair of a longitudinal tear in the posterior tibial tendon. All patients showed subjective and objective improvement. In 8 patients of 9, pain was minor or absent, and these patients were able to perform single heel-rise postoperatively; Although tenosynovectomy has good result we didn’t perform this technique because our patients were classified as stage II/A.
Operative treatment of stage II/A disease can be broadly divided into either soft tissue or bony, and the latter, into medial or lateral column procedures. There is considerable controversy with regard to which technique or combination of techniques will give the best outcome in this subgroup. Medializing calcaneal osteotomy is the most common procedure performed in the United States in stage II/A adult flexible flatfoot [17].
In stage II disease, the posterior tibial tendon becomes elongated, and the medial soft tissues become attenuated. Exploration and debridement of the posterior tibial tendon is performed, but frequently an FDL tendon transfer or side to side anastomosis is required [18]. Combined procedures, including soft tissue reconstructions to restore posterior tibial tendon function and bony procedures to correct deformity, have become popular.
In 2003 a group in the United States presented the result of a survey of 104 academic foot and ankle surgeons in the United States, 98% of whom employed a soft tissue procedure as part of their surgical treatment, with 86% preferring to augment the Posterior tibial tendon with an FDL tendon transfer, 53% of surgeons would repair the spring ligament, while 7% would repair the deltoid ligament.
Of the 70% that corrected the equinus contracture, 36% performed an Achilles tendon lengthening, 23% performed a gastrocnemius aponeurosis lengthening, and 12% performed either of these procedures depending on the clinical examination. 97% of the respondents reported that they would perform some form of bony correction. These procedures included a medializing calcaneal osteotomy in 73%, lateral column lengthening in 41%.
Proponents of the FDL tendon transfer argue that although the posterior tibial tendon is 3.5 times stronger, the function of the transferred FDL is to oppose the peroneus brevis [19,20]. It was further popularized the use of the FDL tendon transfer to augment the posterior tibial tendon [21,22]. It was concluded that while this procedure did well to relieve pain and improve inversion strength, correction of the deformity was moderate [16,20,22,23].
Due to concerns of lack of deformity correction with FDL transfer and the necessity of bony procedure to protect it, our team does not include the FDL transfer in the combination technique we describe, especially that FDL is more frequently used in Stage II/B flexible PTTD [13,23,24].
Medializing calcaneal osteotomy is indicated in patients in whom the valgus hindfoot deformity is passively correctable, and the pull of the Achilles tendon can be directed closer to the normal long axis of the calcaneus to the ground [6].
This osteotomy is also effective in relieving calcaneo-fibular impingement pain. In 2004 [9] results were reported on 129 patients treated for PTTD with medial translational calcaneal osteotomy. At a mean follow up of 5.2 years, 91% of patients were satisfied, with statistically significant improvement in radiographic parameters measured at 6 months (97%) and at final follow up (87%) which show nearly the same postoperative results as our combination technique. It has been hypothesized that medializing calcaneal osteotomy corrects flatfoot deformity by re-tensioning the plantar fascia [25]. Spring ligament reconstruction corrects the flatfoot deformity in cadaveric studies but has not been proven clinically [26].
The most common lateral column procedures are both Evans lateral column lengthening through the distal calcaneus [27-29] and calcaneocuboid distraction arthrodesis [28,30].
The aim of the lateral calcaneal lengthening is to adduct the forefoot at the talonavicular joint and correct the peritalar subluxation [29,31].
As the lateral column is lengthened, the navicular is translated medially on the talar head. This results in plantarflexion of the forefoot at the talonavicular joint and elevation of the medial longitudinal arch. Nonunion rate is quoted as 1%–5% with increased risk in smokers [28,32,33].
A criticism of lateral column lengthening is that it does not correct the deforming force of the achilles tendon and leads to inadequate correction of hindfoot valgus and is better used for correction forefoot abduction rather than hindfoot valgus [32]. Medializing calcaneal osteotomy can correct hindfoot valgus and alter the direction of pull from the Achilles tendon from eversion to a neutral axis. The development of an increase in joint pressure and calcaneocuboid arthritis as well as non-union issues are drawbacks of lateral calcaneal lengthening techniques [33,34].
Application of sinus tarsi implant or arthroereisis will reduce talonavicular divergence and correct hindfoot valgus by inducing medial translation of the calcaneus under the talus and reducing the talar head uncoverage including the talar plantarflexion and varization of the hindfoot proportional to screw size. The main drawback of this procedure is the sinus tarsi pain and the possibility of implant removal [35]. Subtalar arthroereisis has proprioceptive benefits on the contralateral foot and helps maintain the correction even after removal of the implant [36] (Figure 9).
Figure 9: A) Preoperative Studied Angles Measurement on Lateral and Anteroposterior Radiography. B) Postoperative Studied Angles Measurement on Lateral and Anteroposterior Radiography. C) Minimal Change of studied Angles Measurement on Lateral and Anteroposterior Radiography After 8 Months of Artheroeresis Implant Removal.
Percutaneous medializing calcaneal osteotomy is safe and it is performed in a chevron calcaneal osteotomy manner without significant neurovascular damage and with the benefit of soft tissue preservation [37]. Correction of any gastrocnemius tightness is paramount and its aponeurosis lengthening has been reported to cause less weakening in plantarflexion than Achilles tendon lengthening this is why we preferred to use it in our operative technique [38]. In addition to medializing calcaneal osteotomy that addresses the hindfoot valgus the benefit behind our use for arthroereisis is to further gain a greater correction of the hindfoot alignment [35].
In 2010 a combination technique was published on 14 patients with flexible flatfoot, using open double osteotomy and Achilles tenoplasty and showed radiological and functional improvement nearly similar to our results [39]. The combination technique we adopted is also supported by a study underwent and published in 2017 about percutaneous medializing calcaneal osteotomy that showed no sural nerve injuries and improvement in all angles similar to our results. Thus, the importance of percutaneous osteotomy which prevents skin complication and decreases infectious risks [17].
According to the literature and the arguments previously said, we decided to combine percutaneous medializing calcaneal osteotomy, gastrocnemius achilles lengthening and arthroereisis on our 31 patients of stage II/A flexible flatfoot deformity without the necessity to add further medial soft tissue repair or tendon transfers. The operative technique was the same in all our patients and we are the first group to perform this combination of already described techniques that we believe is effective to address the major deformities of flexible flatfoot without the aid of tendon transfer which was endorsed by the radiographic improvement of all the variables we studied. Improvements achieved in our study group were not limited to radiography results. Significant improvements in AOFAS scores were also noted. Patient pain diminished or disappeared, and they achieved better walking distance.
Four complications were encountered. Three sinus tarsi pain with resolved symptoms after implant removal 8 months after the procedure and one painful scar associated with the surgical approach to the calcaneus at the incision site. No reports of nerve injuries are noted. These results suggest that this combination is beneficial and provides correction of the deformity. This study is limited by the small sample size and lack of a control group but we believe that it has contributed to further understanding of the disease and its treatment modalities.
Conclusion
Overall, our Posterior tibial tendon deficiency is the most common cause of adult acquired flatfoot deformity. The main deforming forces, Achilles tendon and peroneus brevis tendons, act to promote hindfoot eversion and attenuate structures that stabilize the medial column.
Our method of correction flexible flatfoot in adults is a reproducible bone and soft tissue combination technique on 35 feet with Stage II/A, includes gastrocnemius achilles lengthening, arthroereisis and percutaneous medializing calcaneal osteotomy that corrects the hindfoot valgus, reduces the talocalcaneal divergence in both sagittal and frontal planes and restores the medial longitudinal arch.
Complications might be due to sinus tarsi syndrome after arthroereisis and patients might need to be re-operated for sinus tarsi material removal. Remains to demonstrate with greater follow up the effectiveness of this combination without the need to add a tendon transfer or medial soft tissue tensioning.
Conflict of Interest
We have no conflict of interests to disclose and the manuscript has been read and approved by all named authors.
Acknowledgement
The authors are very thankful and honored to publish this article in the respective Journal and are also very great full to the reviewers for their positive response to this article publication.
References
- Toullec E (2015) Adult flatfoot review. Orthop Traumatol Surg Res. 101:S11-S7.
- Brodsky JW (2004) Preliminary gait analysis results after posterior tibial tendon reconstruction: A prospective study. Foot Ankle Int. 25(2):96-100.
- Deland JT (2001) The adult acquired flatfoot and spring ligament complex. Pathology and implications for treatment. Foot Ankle Clin. 6(1):129-35.
- Johnson KA, Strom DE (1989). Tibialis posterior tendon dysfunction. Clin Orthop Relat Res. 23:196-206.
- Myerson MS (1997) Adult acquired flatfoot deformity: Treatment of dysfunction of the posterior tibial tendon. Instructional Course Lecture. 46:393-405.
- Tryfonidis M, Jackson W, Mansour R, Cooke PH, Teh J, et al. (2008) Acquired adult flatfoot due to isolated plantar calcaneonavicular (spring) ligament insufficiency with a normal tibialis posterior tendon . Foot Ankle Surg. 14(2):89-95.
- Wicart P, Toullec E (2010) Le pied plat idiopathique. Elsevier Masson. 157-73.
- Weinfeld SB (2001) Medial slide calcaneal osteotomy: Technique, patient selection, and results. Foot Ankle Clin. 6(1):89-94.
- Myerson MS, Badekas A, Schon LC (2004) Treatment of stage II posterior tibial tendon deficiency with flexor digitorum longus tendon transfer and calcaneal osteotomy. Foot Ankle Int. 25(7):445-50.
- De Pellegrin M , Moharamzadeh D, Strobl WM, Biedermann R (2014) Subtalar extra-articular screw arthroereisis (SESA) for the treatment of flexible flatfoot in children J Child Orthop. 8(6):479-87.
- Barrie J (2009) Symposium on the adult flat foot: Orthotic management. British orthopaedic foot & ankle society annual scientific meeting.
- Niek van Diek C, Kort N, Scholten PE (1997) Tendonoscopy of the posterior tibial tendon. Arthroscopy. 13(6):692-8.
- Sitler DF, Bell SJ (2003) Soft tissue procedures. Foot Ankle Clin. 8(3):503-20.
- Myerson M, Solomon G, Shereff M (1989) Posterior tibial tendon dysfunction: Its association with seronegative inflammatory disease. Foot Ankle. 9(5):219-25.
- Teasdall RD, Johnson KA (1994) Surgical treatment of stage I posterior tibial tendon dysfunction. Foot Ankle Int. 15(12):646-8.
- Funk DA, Cass JR, Johnson KA (1986) Acquired adult flatfoot secondary to posterior tibial tendon pathology. J Bone Joint Surg Am. 68(1):95-102.
- Mourkus H, Prem H (2018) Double calcaneal osteotomy with minimally invasive surgery for the treatment of severe flexible flatfeet. Int. Orthop.. 42:2123–2129
- Sizensky JA, Marks RM (2003) Medial-sided bony procedures: Why, what, and how? Foot Ankle Clin. 8(3):539-62.
- Hiller L, Pinney SJ (2003) Surgical treatment of acquired flatfoot deformity: What is the state of practice among academic foot and ankle surgeons in 2002? Foot Ankle Int. 24(9):701-5.
- Mann RA (2001) Posterior tibial tendon dysfunction: Treatment by flexor digitorum longus transfer. Foot Ankle Clin. 6(1):77-87.
- Silver RL, De La Garza J, Rang N (1985) The myth of muscle balance: a study of relative strengths and excursions of normal muscles about the foot and ankle. J Bone Joint Surg Br. 67(3):432-7.
- Mann RA, Thompson FM (1985) Rupture of the posterior tibial tendon causing flat foot. J Bone Joint Surg Am. 67(4):556-61.
- Guyton GF, Jeng C, Krieger LE, Mann RA (2001) Flexor digitorum longus transfer and medial displacement calcaneal osteotomy for posterior tibial tendon dysfunction: A middle-term clinical follow-up. Foot Ankle Int. 22(8):627-32.
- Horton GA, Myerson MS, Parks BG, Park YW (1998) Effect of calcaneal osteotomy and lateral column lengthening on the plantar fascia: A biomechanical investigation. Foot Ankle Int. 19(6):370-3.
- Deland JT, Arnoczky SP, Thompson FM (1992) Adult acquired flat foot deformity at the talonavicular joint: reconstruction of the spring ligament in an in vitro model. Foot Ankle. 13(6):327-32.
- Thordarson DB, Schmotzer H, Chon J (1995) Reconstruction with tenodesis in an adult flat foot model. J Bone Joint Surg Am. 77(10):1557-64.
- Evans D (1975) Calcaneovalgus deformity. J Bone Joint Surg Br. 57(3):270-8.
- Mosier-LaClair S, Pomeroy G, Manoli A (2001) Operative treatment of the difficult stage 2 adult acquired flat foot deformity. Foot Ankle Clin. 6(1):95-119.
- Sands AK, Tansey JP (2007) Lateral column lengthening. Foot Ankle Clin.12(2):301-8.
- Thomas RT, Wells BC, Garrison RL, Prada SA (2001) Preliminary results comparing two methods of lateral column lengthening. Foot Ankle Int. 22(2):107-19.
- Gallina J, Sands AK (2003) Lateral-sided bony procedures. Foot Ankle Clin. 8:563–567.
- Suh HD, Park JH, Lee SH, Kim HJ, Park YH, et al. (2019) Lateral column lengthening versus subtalar arthroereisis for paediatric flatfeet: A systematic review Int Orthop. 43(5):1179-1192.
- Bolt P, Coy S, Toolan B (2007) A comparison of lateral column lengthening and medial translational osteotomy of the calcaneus for the reconstruction of adult acquired flat foot. Foot Ankle Int. 28(11):1115-23.
- Neufield SK, Myerson M (2001) Complications of surgical treatments for adult flat foot deformities. Foot Ankle Clin. 6(1):179-91
- Brancheau SP, Walker KM, Northcutt DR (2012) An Analysis of Outcomes after Use of the Maxwell-Brancheau Arthroereisis Implant .The Journal of Foot & Ankle Surgery. 51:3–8.
- Saxena A, Widtfeldt A (2004) Endoscopic gastrocnemius recession: preliminary report on 18 cases. J Foot Ankle Surg. 43:302–306.
- Abigail D, Rana B, Sujit K, Kartik H, Lyndon M (2015) Minimally invasive calcaneal osteotomy: does the shannon burr endanger the neurovascular structures? A cadaveric study. The J Foot and Ankle Surgery. 54:1062–1066.
- Myerson MS, Corrigan J, Thompson F (1995) Tendontransfer combined with calcaneal osteotomy for treatment of posterior tibial tgendon insufficiency: a radiological investigation. Foot Ankle Int. 16:712–718.
- Basioni Y, El-Ganainy A, El-Hawary A (2011) Double calcaneal osteotomy and percutaneous tenoplasty for adequate arch restoration in adult flexible flat foot. Int Orthopaedics (SICOT). 35:47–51.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3143
- [From(publication date): 0-2021 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 2458
- PDF downloads: 685