Temperomandibular Disorder Related Causes - A Short Communication
Received: 30-Mar-2021 / Accepted Date: 23-Sep-2021 / Published Date: 30-Sep-2021
Abstract
This article aims to review the common causes associated with temporomandibular joint Disorders (TMD) by screening all the case reports published in the last 5 years. PubMed search was done and articles pertaining to etiology and treatment aspects were reviewed from 2013 to 2017. A total of 277 case reports were screened. Based on the case reports it was grouped into systemic, local and other causes.
Keywords: TMD; Ankylosis; Trauma; Syndromes
Introduction
TMD signs and symptoms were first discovered by Costen in 1934 [1]. The etiology of TMD has many aspects and can be grouped under initiating factors, predisposing factors and perpetuating factors. Okeson identified dental factors, emotional factors and parafunctional activities as main causes of TMD [2]. Signs and symptoms of TMD are divided into 6 broad groups, such as joint noises, locking, pain and muscle tenderness in head, neck and shoulders, ear complaints and psychological effects [3].
Diagnostic aids such as MRI, ultrasound, vibratography, sonography, electromyography and thermography are used to confirm TMD. Arriving at the correct diagnosis is sometimes challenging and often leads to misdiagnosis of the condition. The three main groups of TMD are categorized under myofascial pain disorder, disc displacement disorder and degenerative disorder [4]. Identifying the etiology is paramount in treatment of temporomandibular disorders. In order to understand varying etiology we carried out a short literature search of the various conditions that could be associated with TMD.
Methodology
The aim of this short communication was to reason out the various causes of TMD. Hence, the key terms temporomandibular joint disorders, Treatment, Etiology were used to search PubMed. Only case reports related to TMD from 2013-2017 were reviewed. A total of 277 articles were reviewed, out of which 57 were eliminated due to lack of clarity in regard to the etiology. 220 case reports were screened and the various etiological factors associated with TMD were segregated into local factors, systemic factors and others.
Results
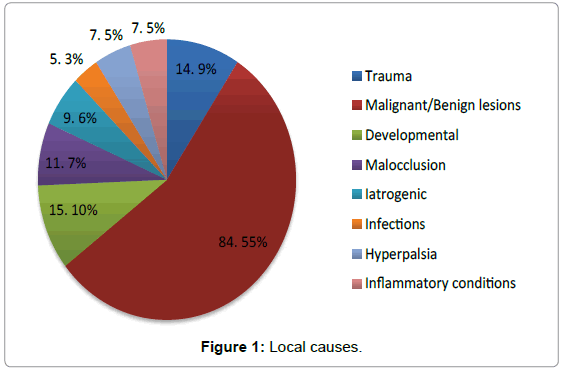
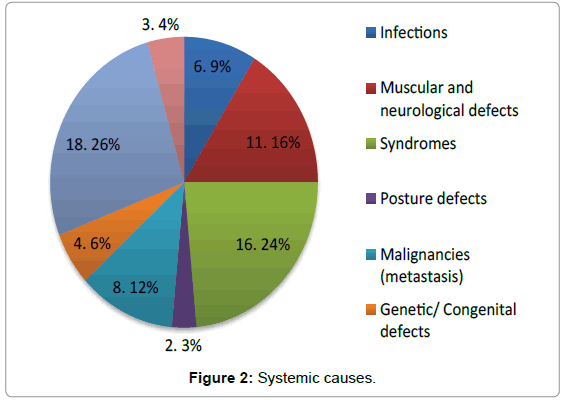
Tables 1 and 2 depict the number of cases under the various local and systemic etiological factors. Figures 1 and 2 highlights the percentages of cases under various categories. The highest numbers of cases in the local causes were observed under malignant and benign conditions, followed by developmental anomalies. Under the systemic causes, the maximum numbers of cases were observed under arthritis and other degenerative conditions, followed by syndromes and muscular and neurological defects.
| Local Causes | Cases(n) |
|---|---|
| Trauma | 14 |
| Malignant/Benign conditions | 84 |
| Developmental | 15 |
| Malocclusion | 11 |
| Iatrogenic | 9 |
| Infections | 5 |
| Hyperplasia | 7 |
| Inflammatory conditions | 7 |
Table 1: Local causes.
| Systemic Causes | Cases(n) |
|---|---|
| Infections | 6 |
| Muscular/Neurological defects | 11 |
| Syndromes | 16 |
| Posture defects | 2 |
| Malignancies (Metastasis) | 8 |
| Genetic/Congenital | 4 |
| Arthritis/Other degenerative diseases | 18 |
| Others | 3 |
Table 2: Systemic causes.
Discussion
The local causes of TMD observed were categorized under trauma, malignancy, developmental, dental [5-7] due to Para functional [6] or after orthodontic/multiple restorative treatments, infections and inflammatory conditions. The systemic causes observed were infections, muscular/neurological defects, Syndromes, posture defects [5], malignancies (Metastasis) [8] ,genetic/congenital, and arthritis/ other degenerative diseases [9-12]. Apart from the systemic and local factors iatrogenic causes such as extensive and faulty restorations, orthodontic procedures done in haste, cosmetic surgical corrections can cause unstable occlusion in intercuspal position initiating TMD. Any change in anterior guidance, occlusal curvature and vertical dimension can lead to TMD [13]. In yet another aspect many case reports have indicated association between altered head and cervical postures to be cause of TMD [14].
The syndromes associated with TMD from this review of past five year case reports were Harlequin syndrome (sympathetic nervous system damage), Trichorhinophalangeal syndrome type 1 (genetic) rare autosomal dominant disorder, Gardner’s syndrome (autosomal dominant), Persistent foramen tympanicum Huschke, Proteus syndrome, Red ear syndrome with tinnitus, [11] Goldenhar syndrome and pain in TMJ, Carey Fineman Ziter syndrome, Ramsay hunt syndrome(after TMJ surgery), Iou Gehrigs disease, Alice in wonderland syndrome, Eagle syndrome, Early lethal Costello syndrome HRAS associated with pulmonary vascular disease and Munch Meyers disease. It is not clear whether theses syndromes can be attributed as etiological factors for TMD. Certain syndromes associated with abnormalities of connective tissue, collagen, muscles and tendons could be considered as conditions which might give rise to TMD.
A number of malignant and benign local and systemic conditions could cause TMJ problems or simply produce TMD symptoms. There have been numerous reports suggesting the misdiagnosis of an underlying condition as a TMD. A proper detailed medical history, examination and diagnosis is essential in proper treatment and hence wellbeing of the patient.
Conclusion
A complete medical, dental and occlusal evaluation needs to be made to confirm the causes for TMD. In 3 case reports TMD was diagnosed but it was malignancy and other muscular diseases which was the underlying cause. Hence, an in depth knowledge in history taking along with clinical evaluation and diagnostic aids are essential to confirm TMD. Apart from these aspects the treatment for TMD should be evidenced based guideline with a multidisciplinary approach.
References
- Costen JB (1934) A syndrome of ear and sinus symptoms based on distributed function of the Temperomandibular. Ann Otol Rhinol Laryngol 106: 805-819.
- Okeson JP (2003) Management of Temporomandibular Disorders and Occlusion.
- Turk DC (1997) Psychosocial and behavioral assessment of patients with temporomandibular disorders: diagnostic and treatment implications. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 83: 65-71.
- Lausten LL, Glaros AG, William K (2004) Inter-examiner reliability of physical assessment methods for assessing temporomandibular disorders. Gen Dent 52: 509-513.
- Cortese S, Mondello A, Galarza R, Biondi A (2017) Postural alterations as a risk factor for temporomandibular disorders. Acta Odontol Latinoam 30: 57-61.
- Muzalev K, Visscher CM, Koutris M, Lobbezoo F (2017) Long-term variability of sleep bruxism and psychological stress in patients with jaw-muscle pain: report of two longitudinal clinical cases. J Oral Rehabil.
- Maruo IT (2017) Class II Division 2 subdivision left malocclusion associated with anterior deep overbite in an adult patient with temporomandibular disorder. Dental Press J Orthod 22: 102-112.
- Guarda-Nardini L, Stellini E, Di Fiore A, Manfredini D (2017) A Rare Case of Misdiagnosed Silent Lung Cancer with Solitary Metastasis to the Temporomandibular Joint Condyle. J Oral Facial Pain Headache 31: 180-185.
- Chebbi R, Khalifa HB, Dhidah M (2016) Temporomandibular joint disorder in systemic sclerosis: a case report. Pan Afr Med J 25: 164.
- Ayachi S, Mziou Z, Moatemri R, Khochtali H (2016) Bilateral septic arthritis of the temporo mandibular joint: case report. Pan Afr Med J 25: 100.
- Kreuzer PM, Vielsmeier V, Poeppl TB, Langguth B (2017) A Case Report on Red Ear Syndrome with Tinnitus Successfully Treated with Transcranial Random Noise Stimulation. Pain Physician 20: E199-E205.
- Gao QQ, Feng YY, Bu LX, Song K, Dai X, et al. (2016) [Pigmented villonodular synovitis of the temporomandibular joint: report of one case and review of literatures]. Shanghai Kou Qiang Yi Xue 25: 381-384.
- McNamara JA, Seligman DA, Okeson JP (1995) Occlusion, Othodontic treatment and Temperomandibular disorders; A Review. J Orofacial Pain 9: 73-89.
- Farias A, Alves V, Gandelman H (2001) Study of the relationship between dysfunction of the Temperomandibular joint and postural alterations. Revista Odontologica UNICID 12: 125-133.
Citation: Muthiah L, D’souza J, Kanwal A, George BT (2021) Temperomandibular Disorder Related Causes - A Short Communication. J Dent Sci Med 3: 124.
Copyright: © 2021 Muthiah L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2678
- [From(publication date): 0-2018 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 1863
- PDF downloads: 815