Temporomandibular Joint Dislocation in an 36-Month-Old Child: A Rare Emergency
Received: 01-Nov-2022 / Manuscript No. nnp-22-79649 / Editor assigned: 03-Nov-2022 / PreQC No. nnp-22-79649(PQ) / Reviewed: 17-Nov-2022 / QC No. nnp-22-79649 / Revised: 23-Nov-2022 / Manuscript No. nnp-22-79649(R) / Accepted Date: 23-Nov-2022 / Published Date: 29-Nov-2022 DOI: 10.4172/2572-4983.1000269 QI No. / nnp-22-79649
Abstract
Temporomandibular joint (TMJ) dislocation in pediatric population is extremely rare. In the literature, a few pediatric cases have been reported. We describe, in these reports, a case of a 36-month-old boy who presented to the department of pediatric dentistry with inability to close his mouth and drooling of saliva. Diagnosis of temporomandibular joint dislocation can be realised based on clinical findings. No complementary studies are required if there is no history of direct mandibular trauma. The maneuver of reduction can be carried out in the field without specific equipment, just with manual reduction.
Keywords
Child; Dislocation; Temporomandibular joint
Introduction
Temporomandibular joint (TMJ) dislocation is a painful condition [1-2] that occurs when the Dislocation refers the phenomenon in which condyle is displaced out of the glenoid fossa and traverses in front of the articular eminence[3].TMJ dislocation is extremely rare in children [4]. It is caused by trauma or simply from opening the mouth during yawning, vomiting and dental treatment [5].Impressive, this pathology is very uncomfortable for the patient; pain on the masseter muscle, impossibility to chew, to speak and eat [6]. Therefore, it usually requires urgent medical attention [1].
Case Report
A previously healthy 36-month-old boy was referred to the department of pediatric dentistry, Faculty of Dental Medicine in Rabat, Morocco. Two days ago, his mother brought him to the emergency center with complaint of the child not being able to close her mouth and drooling of saliva. This had occurred after crying spells following knee injury. He was seen by the paediatric duty registrar who judged that the knee injury was not so serious. Unfortunately, the first attempt at manual reduction was doomed to failure.
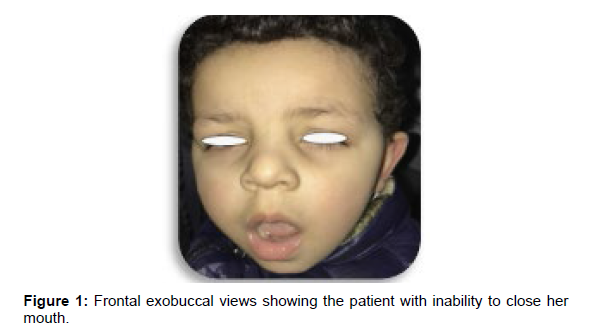
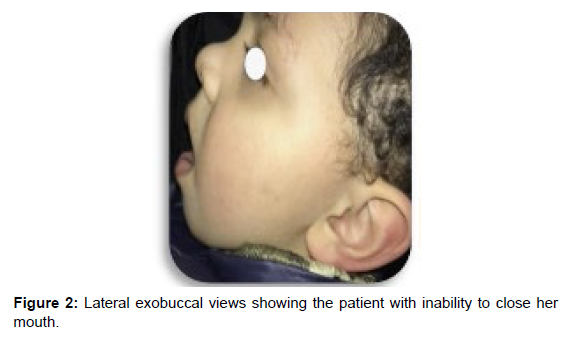
The child was transferred to our department two days later and it was still unable to close his mouth. On clinical examination, the child was tired and distressed. He was unable to occlude his teeth, to drink, to talk or eat properly. The inability to occlude teeth, pursed lip, and drooling, protruding lower jaw were also present. on palpation, both condyles were found outside their glenoid cavity. Panoramic X-ray could not be taken because of the non-cooperation of patient. The clinical signs clearly lead us to a diagnosis of bilateral TMJ dislocation. (Figures 1 and 2).
The TMJ was manually reduced via a Nelaton maneuver. At the end of the procedure, the patient was able to regain his normal dental occlusion and lower jaw mobility (Figures 3 and 4). Barton’s bandage was used to prevent a possible recurrence (Figure 5).
A soft diet was prescribed for 1 to 2 weeks. The adjunct prescription combines analgesics of level I (paracetamol) and non-steroidal antiinflammatory drugs. The patient was informed of a possible recurrence.
Indeed, a similar episode had occurred two days later with spontaneous resolution during sleeping on the stomach. At 1 week follow up, our patient was in bon condition (Figure 6).
Discussion
The TMJ is a synovial joint that can perform rotational and sliding movements. Dislocation of the TMJ is defined as a displacement of the condyle out of the glenoid fossa [7]. The highest incidence is observed among young women in the age ranged between 21 and 30 years. However, no studies report the incidence of TMJ dislocation in children [8].
Temporomandibular joint (TMJ) dislocation is extremely rare in pediatric population. Few pediatric cases have been reported in the literature [9], because of the articular eminence is not fully developed in pediatric populations and the glenoid fossa is almost at flat, hence diminishing the chances of dislocation [4, 8].
Several etiologies can be associated with this pathology [8], including congenital, iatrogenic, anatomical, spontaneous, pharmacological, neurological, neuromuscular, etc [3]. The different causes of TMJ dislocation are classified in the following (Table 1).
| Trauma | When the mouth is open |
|---|---|
| Medical and surgical procedures | Dental extractions under general anaesthesia, intubation procedures, gastrointestinal endoscopy, laryngoscopy/bronchoscopy. |
| Daily activities | Laughing, yawning, biting, singing |
| Anatomical aberrations | Small condyle, poorly grooved glenoid fossa, shallow/steep articular eminence, laxity of ligaments and capsule for more prone for dislocation |
| Systemic disorders | Marfan’s syndrome, Huntington disease, multiple sclerosis, muscle dystrophies or dystonias, epileptic seizures |
| Medications | Antipsychiatric, antiemetic |
| Occlusal conditions | Edentulous posterior region |
Table 1: Etiology of TMJ dislocation [3, 8].
In our case, the TMJ dislocation was caused by screaming for a long time, out of any context of mandibular trauma.
Rowe and Killey classified the dislocation into several categories
• According to the duration of the dislocation episode, we find: cute dislocation, habitual dislocation/subluxation, chronic recurrent dislocation, long-standing/chronic protracted dislocation.
• According to the direction of displacement, there are: anterior, posterior, medial lateral, superior.
• According to the side of displacement we find: unilateral, bilateral [3].
Some authors feel that only a careful clinical examination is sufficient to make the diagnosis outside of history of direct mandibular trauma [4-7]. The typical presentation is that of inability to speak, to drink or eat and also inability to close the mouth, with drooling of saliva [6, 9].
Imaging is generally not necessary except in the context of trauma to exclude condyle fractures [9]. Nevertheless, imaging can provide additional information regarding the morphology of condyle, articular eminence, and joint space. Orthopantomogram can also show the position of the condyle in relation to the articular eminence [3]. In this case, we would have liked to take X-ray imaging to confirm the clinical diagnosis, but our patient was uncooperative.
The first choice for acute dislocations is conservative methods include symptomatic pain relief with analgesics and manual repositioning of the mandibular condyle into the glenoid fossa, it considered to be the best approach [1]. It consists to applying bimanual intraoral force on the mandibular molars of the patient in an inferior and then posterior direction. Then, the dislocated condyle back into the glenoid fossa [10].
In case of chronic recurrent dislocations, a real challenge will be posed to the treating clinician. Conservative methods are chosen first. This method includes the use of various sclerosing agents like alcohol, sodium tetradecyl sulfate, sodium psylliate, morrhuate sodium, and platelet-rich plasma that has been injected into the joint space. The application of botulinum toxin A is also another option for treatment of recurrent TMJ dislocation in pediatric population, as a conservative and reversible treatment with few adverse effects and good results. [3, 11] If we do not get the expected results, we can opt to surgical methods [11]. The patient is being kept under regular follow-up, and if the problem persists, the patient should be referred to a specialized service for possible surgical correction.
Conclusion
In spite of the fact that it is extremely rare, TMJ dislocation is not impossible in children. Pediatric dentists must have sufficient knowledge to allow immediate care of patients who suffered from this pathology, especially since it can occur at any time in the dental chair because of extended dental treatment [4, 7].
References
- Abrahamsson H, Eriksson L, Abrahamsson P (2020) Treatment of temporomandibular joint luxation: a systematic literature review. Clin Oral Invest 24: 61–70.
- Tekeli KM, Keith A (2017) Longstanding unilateral dislocation of the temporomandibular joint in a 6-year-old girl. J Surg Case Rep 10: 1–3.
- Krishnakumar Raja VB (2021) Temporomandibular Joint Dislocation. Oral & Maxillofacial Surg Clini 64: 1381-1399.
- Painatt JM, Veeraraghavan R, Puthalath U (2017) Temporomandibular joint dislocation in an 18-month-old child. Contemp Clin Dent 8: 155-157.
- Whiteman PJ, Carmel Pradel E (2020) Bilateral temporomandibular joint dislocation in a 10-month-old infant after vomiting. Pediatr Emerg Care 16: 418-419.
- Foletti JM, Guyot L, Brignol L (2010) La luxation de mandibule: diagnostic et technique de «réduction sur le terrain». Med Trop 70: 219-220.
- Cascarini L, Cameron MG (2018) Bilateral TMJ Dislocation in a 23-month-old Infant: A Case Report. Dent Update 36: 312-313.
- Atherton GJ, Peckitt SN (1997) Bilateral Dislocation of the Temporomandibular Joints in a 2-Year-Old Child: Report of a Case. J Oral Maxilo fac Surg 55: 646-647.
- Sicard L, O’Hana D, Khonsari RH, Kaddour Brahim A (2018) Bilateral Dislocation of the Temporomandibular Joint in Children. J Oral Maxillofac Surg 76: 1-9.
- Mojtaba MA, Kouhi A, Meighani A, Emami H (2009) Temporomandibular Joint Dislocation Reduction Technique. A New External Method vs the Traditiona. Head and nuck surgery 63: 1–3.
- Sharma NK, Singh AK, Pandey A, Verma V, Singh S(2015) Temporomandibular joint dislocation. Natl J Maxillofac Surg 6: 16-20.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Achabi N, Chhoul H, Ramdi H (2022) Temporomandibular Joint Dislocation in an 36-Month-Old Child: A Rare Emergency. Neonat Pediatr Med 8: 269. DOI: 10.4172/2572-4983.1000269
Copyright: © 2022 Achabi N. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3223
- [From(publication date): 0-2022 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 2756
- PDF downloads: 467