Commentary Open Access
The Difficulty of the Definition of Igg4 Related Sclerosing Cholangitis – Should Cases with Bile Duct Stricture Limited to Intrapancreatic Area be Included in this Disease?
Hirano Kenji*Department of Gastroenterology, University of Tokyo, Tokyo, Japan
- *Corresponding Author:
- Hirano Kenji
Department of Gastroenterology
University of Tokyo, 7-3-1 Hongo
Bunkyo-ku, Tokyo, Japan
Tel: 81-3-3815-5411
E-mail: khirano-tky@umin.ac.jp
Received date: April 17, 2014; Accepted date: May 28, 2014; Published date: June 02, 2014
Citation: Kenji H (2014) The Difficulty of the Definition of Igg4 Related Sclerosing Cholangitis – Should Cases with Bile Duct Stricture Limited to Intrapancreatic Area be Included in this Disease? . J Gastroint Dig Syst 4:187. doi:10.4172/2161-069X.1000187
Copyright: © 2014 Kenji H. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Short Commentary
IgG4-related sclerosing cholangitis (IgG4-SC) is a characteristic type of sclerosing cholangitis which may be regarded as a biliary lesion of IgG4 related disease [1]. The disease name of IgG4-SC is now well known among gastroenterologists, however, there is a confusing problem about its diagnosis. That is, how to deal with intrapancreatic biliary stricture is very difficult. It is known that IgG4-SC is often associated with autoimmune pancreatitis (AIP). As pancreatic head edema may cause the compression of intrapancreatic bile duct, such lesion can be regarded as a part of pancreatic lesion [2,3]. On the other hand, there is another opinion that it should be also regarded as a biliary lesion because biliary wall thickening is often observed in such patients [4].
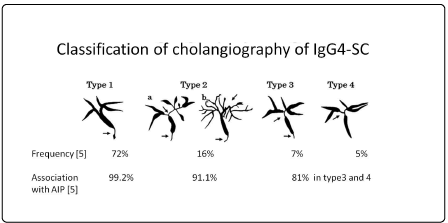
Recently published diagnostic criteria of IgG4-SC included biliary stricture limited to the intrapancreatic area in IgG4-SC (Type 1 IgG4-SC) [1]. Same authors of this diagnostic criteria reported in another paper that 72% of IgG4-SC belonged to Type 1, and 99.2% of Type 1 IgG4-SC was associated with AIP [5] (Figure 1). This very high association rate (99.2%) may suggest that Type 1 IgG4-SC is not an independent biliary lesion. In my previous paper, AIP patients with and without pancreatic head lesion were compared. Intrapancreatic bile duct stricture was observed more frequently in the former group (41/44 vs 2/12, p<0.0001). In addition, the frequency of intrapancreatic biliary wall thickening was also higher in the former group (20/20 vs 2/9, p<0.0001). Thus, intrapancreatic biliary stricture as well as wall thickening is rare without pancreatic head lesion [3]. In fact, according to the recent Japanese national survey of IgG4-SC patients without AIP, only 2% (3/43) belonged to Type 1 [6]. Even if intrapancreatic biliary wall thickening is observed and its pathological findings do not contradict those of IgG4 related diseases, it may be difficult to say that its inflammatory origin is bile duct because such biliary lesion is very rare without pancreatic head lesion. It should be ragarded as spreading of inflammation from pancreas. If pancreatic head cancer infiltrates bile duct and biopsy of bile duct reveals adenocarcinoma, nobody says that such biliary lesion is bile duct cancer. Biliary stricture associated with alcoholic acute or chronic pancreatitis has not been called cholangitis if mild biliary wall thickening was observed [3]. Likewise, the term “Ig4-SC” as an independent disease name should be used when the inflammatory origin is bile duct, not pancreas.
The recent study by Watanabe et al. [7] also showed that there were a small number of patients in whom biliary wall thickening was the dominant factor for the intrapancreatic bile duct stricture [7]. Perplexingly, however, they concluded that type1 IgG4-SC should be included in IgG4-SC. They argued that inherent biliary wall thickening was a dominant factor for the intrapancreatic blle duct stricture in some patients, thus the classification of Type 1 was necessary to pick up them. Objectively speaking, such stricture is dependent on pancreatic head lesion in many cases, and it seems very unreasonable to discuss Type 1 IgG4-SC in line with other types. The problem of including or excluding Type 1 is important because it affects the statistics of IgG4-SC. If this problem is unsolved, it will cause a lot of confusion in discussing IgG4-SC. Many doctors may believe that diagnostic criteria are authoritative, and they should not be changed easily once they are established. However, it is never too late to mend. Type 1 should be excluded from IgG4-SC, or at least it should be separately documented from other types of IgG4-SC considering the difference of pathogenesis.
References
- Ohara H, Okazaki K, Tsubouchi H, Inui K, Kawa S, et al. (2012) Clinical diagnostic criteria of IgG4-related sclerosing cholangitis 2012. J HepatobiliaryPancreatSci 19: 536-542.
- Björnsson E, Chari ST, Smyrk TC, Lindor K (2007) Immunoglobulin G4 associated cholangitis: description of an emerging clinical entity based on review of the literature. Hepatology 45: 1547-1554.
- Hirano K, Tada M, Isayama H, Yamamoto K, Mizuno S, et al. (2010) Endoscopic evaluation of factors contributing to intrapancreatic biliary stricture in autoimmune pancreatitis. GastrointestEndosc 71: 85-90.
- Naitoh I, Nakazawa T, Ohara H, Ando T, Hayashi K, et al. (2009) Endoscopic transpapillaryintraductal ultrasonography and biopsy in the diagnosis of IgG4-related sclerosing cholangitis. J Gastroenterol 44: 1147-1155.
- Ohara H, Nakazawa T, Kawa S, Kamisawa T, Shimosegawa T, et al. (2013) Establishment of a serum IgG4 cut-off value for the differential diagnosis of IgG4-related sclerosing cholangitis: a Japanese cohort. J GastroenterolHepatol 28: 1247-1251.
- Tanaka A, Tazuma S, Okazaki K, Tsubouchi H, Inui K, et al. (2014) Nationwide survey for primary sclerosing cholangitis and IgG4-related sclerosing cholangitis in Japan. J HepatobiliaryPancreatSci 21: 43-50.
- Watanabe T, Maruyama M, Ito T, Maruyama M, Muraki T, et al. (2014) Mechanisms of lower bile duct stricture in autoimmune pancreatitis. Pancreas 43: 255-260.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15443
- [From(publication date):
June-2014 - Aug 24, 2025] - Breakdown by view type
- HTML page views : 10816
- PDF downloads : 4627