The Immediate Effects of Therasuit̨̉ on the Gait Pattern of a Child with Unilateral Spastic Cerebral Palsy
Received: 27-Mar-2017 / Accepted Date: 10-Apr-2017 / Published Date: 17-Apr-2017 DOI: 10.4172/2572-4983.1000S1011
Abstract
Aim: This study analyzes the immediate effects of using TheraSuit® (TS) on the gait of a child with left spastic hemiplegia level II (GMFCS).
Methods: Spatiotemporal gait parameters and kinematic variables in the sagittal plane were compared between baseline and TS conditions.
Results: Positive effects were noted on temporal parameters in the TS condition, such as a reduced gait cadence. The analysis of angular displacements in joint angles showed that at initial contact there was a reduction in the: (i) Plantarflexion on the paretic side; (ii) Dorsiflexion on the non-paretic side; and (iii) Knee flexion angles in both limbs. Furthermore, an increase in hip and knee extension angles during stance, and a decrease in knee and hip flexion on the non-paretic limb during swing were also detected.
Conclusions: Further investigations with larger samples are necessary to confirm these effects of wearing TS on gait kinematics, aiming toward providing a more functional and safer gait pattern in children with spastic hemiplegia.
Keywords: Cerebral palsy; Spastic hemiplegia; Gait analysis; Suit therapy; Spatiotemporal gait parameters; Case study
Introduction
Hemiplegia is a form of spastic Cerebral Palsy (CP) that affects one side of the body. Spastic hemiplegic Cerebral Palsy (SHCP) is the most common syndrome in children born at term, and is second in frequency only to spastic diplegia among preterm infants [1]. Children with this serious condition may have varying combinations of weakness, sensory loss and spasticity, involving the arm and leg of either side of the body [2]. In addition, they exhibit asymmetry between the paretic and the non-paretic sides [3], with decreased muscle volume in the paretic side [4] and significant leg length discrepancy [5].
There are many different therapeutic approaches used in CP rehabilitation by physical therapists (e.g. context-focused therapy, bimanual training, constraint induced movement therapy, neurodevelopmental treatment, goal-directed/functional training, muscle strengthening, and/or home programs for improving motor activities or self-care function). The inclusion of a dynamic orthosis such as TheraSuit®(TS) in the (re)habilitation program of children with CP is usually considered as a complementary therapy. According to Koscielny, suit therapy is considered appropriate for children from 2 years of age to adulthood [6]. However, to our knowledge, there are no published studies conducted with children younger than 6 years of age [7]. This dynamic orthosis could allow more efficient balance control by facilitating proprioception and improving symmetry, walking speed and cadence, trunk control, and motor function in every dimension of Gross Motor Function Measure (GMFM) and self-care. However, a recent systematic review and meta-analysis [7] has highlighted several methodological shortcomings in studies addressing suit therapy, and consequently it was suggested that more research is needed to demonstrate unequivocally that suit therapy is an effective treatment. Furthermore, the authors also raised concern for the lack of clarity on the effects of elastic orthotic. Thus, it is necessary to compare intensive suit therapy with other physical therapy programs, and also to analyze the specific immediate effects of suit therapy on postural control and gait variables by using quantitative analysis.
The aim of this study was to evaluate the immediate effects of TS on spatiotemporal and kinematic variables on the gait of a child with left spastic hemiplegia, level II (GMFCS).
Method
This research with a single-case quasi experimental design, was approved by the Ethics Committee of the Rehabilitation Medicine Center in Alcoitao (CMRA), Portugal. The child was selected based in the following criteria: a) ability to walk independently without the use of assistive devices or orthosis; b) cognitive level and emotional state facilitating understanding and cooperation of the participant; c) parental consent and child assent as required by the ethical committees of the CMRA; d) no history of functional lower limbs surgery and absence of pharmacological treatments in the last year; e) no prior experience with this type of dynamic orthosis (TS) before this study.
Case Description
MR was a five years and 10 months old female with left spastic hemiplegia, classified as level II according to Gross Motor Function Classification System (GMFCS) [8]. Born at 41 weeks of gestational age by spontaneous delivery after an uneventful pregnancy, with birth weight of 3.070 g and Apgar 9-10 at 5-10 min. An ultrasound at 3 days was normal. A Magnetic Resonance Imaging scan at 12 months confirmed an old ischemic partial infarction of the middle cerebral artery on the right side. Fifteen months prior to the study, MR was submitted to a percutaneous lengthening procedure of the left Achilles tendon for reducing ankle equinus.
Procedure and Data collection
A physical examination was performed a day before data collection. The child showed normal Range of Movement in non-paretic limb and some limitation in paretic lower limb joints. Hip: flexion (125°); abduction with hip extension (35°); lateral rotation (40°). Knee: flexion (140°); extension (-5°). Ankle: dorsal flexion with knee extension (5°); inversion (30°). Plantar flexion and eversion were normal. Selective dorsiflexion of the ankle was graded 1 (i.e., dorsiflexion using extensor hallucis longus and extensor digitorum longus and no activity). The spasticity degree scored with modified Ashworth scale showed: hip flexors and adductors (1); medial rotators (1+); knee flexors (1); dorsiflexors (1+); plantar flexors and eversors (1). The functional profile was classified according recommendations from the Surveillance of Cerebral Palsy in Europe [9] with the following levels: GMFCS (II); Bilateral Fine Motor Function (III); Viking Speech Scale (I). The functional performance scored by the Gross Motor Function Measure-66 was 93.5% and by the Functional Mobility Scale was 5/5. No other associated disorders were reported. Additionally, observational gait analysis was performed by video recordings, to identify the child’s gait pattern. Two experienced pediatric physical therapists used slow-motion to classify the child’s gait pattern. All physical examination data (e.g. ROM, spasticity degree, selective dorsiflexion of the ankle and functional profile) were used to guide the placing of the elastic cords of the TS, according the child’s needs and to compensate her functional problems.
A day after a physical examination, the three-dimensional motion data were acquired during gait in two different conditions: 1) baseline (before TS) and 2) with TS. Anthropometric data was collected with shoes, including body mass (15.9 kg), height (1.145 m), knee width (left: 65 cm; right: 66 cm) and ankle width (left: 48 mm; right: 50 mm). The length of the lower limbs (LL) was clinically assessed (distance from Anterior Superior Iliac Spine to Medial Malleolus): left: 5350 mm; right: 5550 mm; leg discrepancy=20 mm.
Two video-digital cameras (Basler piA1000-48g? GigE) and six infrared cameras (VICON T10) sampled at 100 Hz were used to measure 3D motion of the lower limbs (LL). Sixteen retro-reflective markers were placed on anatomical landmarks of the pelvis and lower extremities, according to the Plug-in-Gait model (VICON, Oxford Metrics, UK) and a prior study [10]. The child wore a comfortable pair of commercially available sneakers during the test protocol [11]. To avoid marker displacement between different test conditions, and to reduce the influence from the footwear on the gait pattern, sneakers were used during baseline and TS conditions [10]. The markers were placed on the skin at the same spot as barefoot measurements reported in the literature [10], except for the hallux marker, which was placed on the shoe. However, when the child wore the TS, only the heel and toe markers remained in the same positions; all the others markers were placed on the TS at the positions that best reproduced the anatomical landmarks. The assessments were performed in one day by two experienced pediatric physical therapists.
The participant was asked to walk a distance of 4 m for at least five times (i.e. 20 m in total) at a self-selected walking speed, forward and back, until she was instructed to stop. The data set of spatiotemporal and kinematic variables was recorded to obtain at least three successful trials for each LL (range: 3-6) in both conditions. Rest breaks were allowed between the trials (three min) and between the conditions (20 min). Nine clinically relevant spatiotemporal gait parameters and LL angles displacement (sagittal plane) were selected for further analysis. Means and standard deviations were used to explore differences between the two conditions. Distance measures were non-normalized; however, temporal measures were normalized to a percentage of the gait cycle. Values of kinematic variables in the sagittal plane were used to compare differences in angular displacements of the hip, knee and ankle joints during gait cycle, in both conditions.
Results
Table 1 summarizes the mean and standard deviation values of spatiotemporal parameters, in both conditions.
| Conditions | Baseline (without TS) | With TS | ||
|---|---|---|---|---|
| ST Parameters | Paretic LL | Non Paretic LL | Paretic LL | Non Paretic LL |
| Cadence (steps/min) | 156 ± 10.1 | 132 ± 3.43 | ||
| Velocity (m/second) | 1.33 ± 0.11 | 0.95 ± 0.052 | ||
| Step time (second) | 0.43 ± 0.036 | 0.35 ± 0.025 | 0.50 ± 0.040 | 0.41 ± 0.020 |
| Stance Phase (%gait cycle) | 52.7 ± 1.75 % | 61.6 ± 1.36 % | 53.7 ± 2.25 % | 63.2 ± 1.43 % |
| Swing Phase (%gait cycle) | 46.3 ± 2.78 % | 41.8 ± 5.15 % | 45.1 ± 2.80 % | 41.6 ± 4.68 % |
| Single support (% gait cycle) | 37.3 ± 1.29 % | 46.3 ± 2.78 % | 38.0 ± 3.17 % | 45.1 ± 2.80 % |
| Double support (% gait cycle) | 15.4 ± 1.71 % | 16.9 ± 3.12 % | ||
| Step Length (m) | 0.50 ± 0.022 | 0.54 ± 0.021 | 0.41 ± 0.029 | 0.46 ± 0.045 |
| Stride width (m) | 0.10 ± 0.022 m | 0.19 ± 0.029 | ||
Table 1: Spatial-temporal (ST) gait parameters of the lower limbs (LL) derived from data collection at baseline and Therasuit® (TS) conditions.
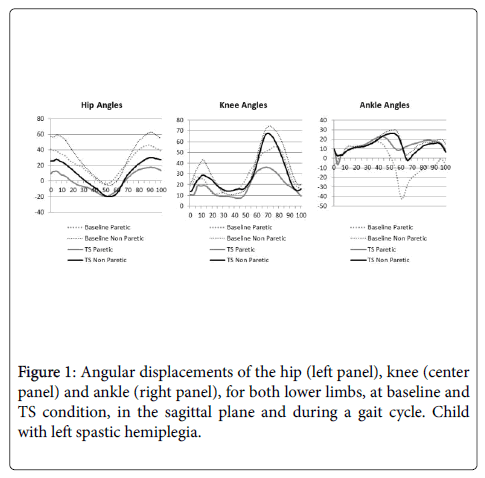
Some positive effects of TS on temporal parameters were noted in the child’s gait, such as a reduced cadence (Table 1). Furthermore, the results showed a slower gait velocity and an increase in double support duration in the TS condition. However, we found no positive effects of wearing TS on spatial parameters (shorter step length and larger step width). Figure 1 represents the kinematic data (hip, knee and ankle angles), in both conditions.
Effects on the kinematic variables were also detected. At baseline condition, the dorsiflexion angle was higher on the non-paretic LL at initial contact but the paretic LL had a plantarflexion. However, in the TS condition there was a reduction of dorsiflexion on the non-paretic side (BL: 10.2º +/- 3.4; TS: 9.2º +/- 1.5) and plantarflexion on the paretic side (BL: -5.8º +/- 1.1; TS: 9.3º +/- 1.4). Regarding the knee and hip joints, at baseline, both limbs displayed an excessive flexion at initial contact and during stance. Several effects were detected in the TS condition (Figure 1). First, there was a decrease in knee flexion angle on both sides and in hip flexion on the non-paretic side, at initial contact. Second, during the stance phase, we observed an increase in knee extension angle on the paretic LL and in hip extension on both sides. Finally, in the swing phase, there was a decrease in knee and hip flexion angles on the non-paretic LL.
Discussion
This study investigated the immediate effect of using TS on the gait of a child with left spastic CP hemiplegia. The most notable effects concerned temporal gait parameters and kinematic variables. Specifically, when compared with the baseline condition, in the TS condition there was an increase in single support and a decrease of swing phase duration. The stance phase was longer on the non-paretic side in both conditions due to the child’s reduced capability to load and transfer weight [12], and also because of the muscle weakness [13] on the paretic limb. Although wearing TS was associated with some positive effects on gait, it was not sufficient to improve weight transfer to the left side of the body or for the acquisition of better gait symmetry. The results show that the child’s kinematic angles such a marked flexion motion pattern [12] decreased in the TS condition, particularly in the hip and knee joints during the gait cycle. It is possible that the TS provided a higher pattern of extension and a better foot prepositioning for initial contact, thus normalizing dorsiflexion in stance. Typical sagittal-plane abnormalities in the involved limb persisted in the TS conditionwith some values far from normal [14]. Our findings are in agreement with previous studies on hinged ankle foot orthoses (HAFO) [15] and emphasize the importance of studying adaptations on both sides of the body and not only on the paretic side. As proposed by Allen et al., [16] the kinematic changes of the uninvolved limb may result from a compensation of the abnormalities of the hemiplegic side on a normal but functionally longer limb. Although some positive results were found, the mechanisms underlying the changes in gait pattern while wearing TS remain unclear. This dynamic orthosis appears to function as a biomechanical constraint that limits the use of typical alternative strategies. Thus, the TS may be used by physical therapists during gait training for children with CP as an alternative dynamic orthosis, which may drive the child to use a new motor strategy, resulting in a safer and more functional gait pattern. Considering the lack of clarity regarding the effects of this elastic orthotic, further investigations are necessary to compare not only intensive suit therapy with other physical therapy programs (conventional method or NDT), but also to analyze the specific immediate and long term effects of the TS on gait pattern in children with all types of Cerebral Palsy.
Conflict of Interest
The authors state that there are no conflicts of interest that could have influenced the preparation of this manuscript.
Funding
This research was funded by the Foundation for Science and Technology (Portugal) PTDC/DTPDES/6776/2014.
References
- Kulak W, Sobaniec W (2004) Comparisons of right and left hemiparetic cerebral palsy. Comparative Study. PediatrNeurol 31: 101-108.
- Boyd RN, Morris ME, Graham HK (2001) Management of upper limb dysfunction in children with cerebral palsy: a systematic review. Eur J Neurol 8: 150-166.
- NovacheckTF, Gage JR (2007) Orthopedic management of spasticity in cerebral palsy. Childs NervSyst 23: 1015-1031.
- Malaiya R, McNee AE, Fry NR, Eve LC, Gough M, et al. (2007) The morphology of the medial gastrocnemius in typically developing children and children with spastic hemiplegic cerebral palsy. J ElectromyogrKinesiol 17: 657-663.
- Riad J, Finnbogason T, Brostrom E (2010) Leg length discrepancy in spastic hemiplegic cerebral palsy: a magnetic resonance imaging study. J PediatrOrthop. 30: 846-850.
- Koscielny R (2004) Strength training and cerebral palsy. Cerebral Palsy Magazine 2: 12-14.
- Martins E, Cordovil R, Oliveira R, Letras S, Lourenco S, et al. (2016) Efficacy of suit therapy on functioning in children and adolescents with cerebral palsy: a systematic review and meta-analysis. Dev Med Child Neurol 58: 348-360.
- Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, et al. (1997) Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 39: 214-223.
- Cans C (2000) Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Surveillance of Cerebral Palsy in Europe (SCPE). Dev Med Child Neurol 42: 816-824.
- Hollander K, Riebe D, Campe S, Braumann KM, Zech A (2014) Effects of footwear on treadmill running biomechanics in preadolescent children. Randomized Controlled Trial. Gait Posture 40: 381-385.
- Wolf S, Simon J, Patikas D, Schuster W, Armbrust P, et al. (2008) Foot motion in children shoes: a comparison of barefoot walking with shod walking in conventional and flexible shoes. Gait Posture 27: 51-59.
- Cimolin V, Galli M, Tenore N, Albertini G, Crivellini M (2007) Gait strategy of uninvolved limb in children with spastic hemiplegia. EuraMedicophys 43: 303-310.
- Olney SJ, MacPhail HE, Hedden DM, Boyce WF (1990) Work and power in hemiplegic cerebral palsy gait. PhysTher 70: 431-438.
- Sutherland DH, Olshen RA, Biden E, Wyatt MP (1988) The development of mature walking. Oxford: Mac Keith Press.
- Buckon CE, Thomas SS, Jakobson-Huston S, Sussman M, Aiona M (2001) Comparison of three ankle-foot orthosis configurations for children with spastic hemiplegia. Dev Med Child Neurol 43: 371-378.
- Allen PE, Jenkinson A, Stephens MM, O'Brien T (2000) Abnormalities in the uninvolved lower limb in children with spastic hemiplegia: the effect of actual and functional leg-length discrepancy. J PediatrOrthop 20: 88-92.
Citation: Martins E, Cordovil R, Oliveira R, Pinho J2, Vaz JR (2017) The Immediate Effects of Therasuit® on the Gait Pattern of a Child with Unilateral Spastic Cerebral Palsy. Neonat Pediatr Med 3: S1011. DOI: 10.4172/2572-4983.1000S1011
Copyright: © 2017 Martins E, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5176
- [From(publication date): 0-2015 - Dec 11, 2025]
- Breakdown by view type
- HTML page views: 4241
- PDF downloads: 935