Research Article Open Access
The Outcome of Blood Cultures in Febrile Children Presenting at theEmergency Department
Salamah KM1*, Awean GZ1, Alkume N2 and Abdussalam Shah AK1
1Department of Pediatrics, Hamad Medical Corporation, Al Wakra Hospital, Qatar
2Department of Pediatrics, Sidra Medical and Research Center, Qatar
- *Corresponding Author:
- Salamah KM
Department of Pediatrics
Hamad Medical Corporation
Al Wakra Hospital, Qatar
Tel: 0097440114258
E-mail: ksalameh@hamad.qa
Received Date: November 24, 2016; Accepted Date: December 12, 2016; Published Date: December 19, 2016
Citation: Salamah KM , Awean GZ, Alkume N, Abdussalam Shah AK (2016) The Outcome of Blood Cultures in Febrile Children Presenting at the Emergency Department. Neonat Pediatr Med 2: 117. doi: 10.4172/2572-4983.1000117
Copyright: © 2016 Salamah KM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Neonatal and Pediatric Medicine
Abstract
Background: An unknown number of children who attend an Emergency Department may have a serious underlying, systemic infection as a cause of their fever. Blood culture (BC) remains the gold standard approach to establish the diagnosis and presence of pathogens in a child with a suspected, serious bacterial infection. This study investigated the proportion of positive blood cultures and the correlation with basic laboratory investigations (Creactive protein, white blood cell count, and absolute neutrophil count), prescription of antibiotics in patients visiting a pediatric emergency department in a primary hospital Methods: A retrospective study in Qatar- Al Wakra Hospital- Pediatric Emergency Department, over one year. Patients younger than 3 months of age and patients with any form of immune deficiency were excluded. Results: A total of 828 patients (median age 3.55 years) with fever (>38°C) or a history of fever (>38°C). 121 (14.6%) were later admitted to the pediatric ward; 10 (1.2%) to the pediatric intensive care unit and 4 (0.4%) to pediatric surgery. In total, positive blood culture was present in 20 (2.42%) children. Of these 20,4 (20%) were admitted to the pediatric ward, and 9 (45%) were observed in the hospital for less than 24 hrs and 7 (35.0%) were sent back home after a clinical assessment and the results of the initial laboratory tests. The referrals of patients with negative blood culture were similar. There were no differences in the mean value of absolute neutrophil counts or CRP measurement between patients exhibiting positive or negative BC. Conclusion: The incidence of a positive BC in routine care of febrile patients in an emergency department setting is low, 2.42%. There were no significant differences in associated clinical laboratory results (WBC, CRP or ANC) or admission to hospital wards between the groups with positive or negative BC.
Keywords
Blood cultures; Bacteremia; CRP; Neutrophils; Antibiotics
Background
Fever is the most frequent reason for presentation at the pediatric emergency department (PED) [1-5]. The percentage of patients who attend the PED due to fever ranges from 10.5 to 25% [3]. Fever is an important clinical sign because of the association of an underlying infection, although most infections are viral. However, a small group of these children may have a serious bacterial infection as the cause of the fever [2,3,5-7]. One of the greatest challenges to physicians caring for febrile children in the PED is therefore the risk of an occult bacteremia (OB) [8,9]. The proportion of occult bacteremia is variable, and for children less than 3 years of age, it was estimated to be 3-10% in the pre-Hemophilus influenzae B (HiB) vaccine era. This figure has dropped after the introduction of the HiB vaccination and is currently 0.5% after the worldwide adoption of this vaccination program [10]. The mortality rate associated with bacteremia may be as high as 30% [11]. The clinical management of children older than 3 months of age, who present in the PED with fever, is still controversial [10,12]. There is great heterogeneity in the evaluation and the management practices of this group of patients, including the need for a complete blood count (CBC), measurement of C-reactive protein (CRP) and blood culture (BC) [2-4,6,7,13]. BC remains still the gold standard approach to determine the presence or absence of pathogens in a child with a suspected serious bacterial infection or fever of unknown origin [10,14-18]. However, the value of BC in febrile children in the ED has been questioned recently [10,19,20]. In hospital-based studies, the proportion of patients with a positive blood culture was less than 3% [16], even reported to be low as 2% [21]. However, another concern is that blood culture contamination rates in the ED are also substantial and may vary from 1 to 9% and may reach as high as 11%. The consequences of a false positive result include the unnecessary administration of antibiotic therapy, admissions to hospital, prolonged duration of hospitalization and the request of more laboratory tests [14,15,17,22]. It has been described that about 17% to 90% of children receive antibiotics for the common cold [23]. Unnecessary administration of antibiotics creates diagnostic confusion and is associated with increased antibiotic resistance [8,24]. In contrast, delayed antibiotic therapy may result in morbidity and mortality for children who do have a serious bacterial infection [16-19]. Consequently, the issue of the value of blood cultures for children presenting to the ED is an important one. Blood cultures are expensive, painful, and false positive results have many adverse consequences. This study will describe the proportion of positive BC in a population of children with fever or history of fever, the prescription of antibiotics, the association to other markers of infection and the referral to hospital wards.
Subjects and Methods
This was a retrospective study carried out on patients who visited the Pediatric Emergency Department at Al Wakra Hospital (AWH), Qatar - over one year (01-06-2012 to 31-05-2013). The study was approved by the Institutional Review Board of Hamad Medical Corporation, Doha. Following this, a clinical chart review was conducted in order to determine the demographics, clinical presentations, treatment and the blood culture results. The information was entered into an electronic database and subsequently analyzed.
The study population included patients older than 3 months up to 14 years of age. Patients were excluded if they had any of the following: 1) age less than or equal to 3 months, 2) had a congenital or an acquired immune deficiency disease or a malignancy. The criteria to obtain a blood culture was fever (38°>C) or a history of fever and no signs of a focal, localized infection, e.g. pneumonia, UTI or tonsillitis/ear infection. Temperature was evaluated by tympanic measurement. Blood samples were collected under aseptic technique by well trained nurses and send for culture and other analysis [such as white blood cell count (WBC), absolute neutrophil counts ANC and Creactive protein (CRP).
Statistical Analysis
The statistical analysis was carried out using descriptive statistics, including means and frequencies, and inferential statistics, that included using Student’s t test and χ2 test. Student’s t test was used to test the significance of the differences between the mean values of two continuous variables. The χ2 analysis was performed to test the differences in proportions of categorical variables between ≥2 groups. In 2 × 2 tables, the Fisher exact test replaced the χ2 test if the assumptions underlying the χ2 test were violated. The level of p<0.05 was considered as the cutoff value for significance. Data analysis was done using SAS software, version 9.4.
Results
The results of blood cultures (BC) taken over one year for 828 patients is presented in Table 1.
| Characteristic | Number (%) |
|---|---|
| Gender | |
| Male | 469 (56.6) |
| Female | 359 (43.4) |
| Nationality | |
| Qatari | 228 (27.5) |
| Non-Qatari | 600 (72.5) |
| Age, years | |
| All, Median, (Range) | 3.55 (0.25-13.83) |
| ≤ 3 | 464 (56.0) |
| >3 to 6 | 205 (24.8) |
| >6 to 10 | 107 (12.9) |
| >10 | 52 (6.3) |
| Blood culture | |
| Positive | 20 (2.42) |
| Negative | 808 (97.6) |
| Antibiotic Use | |
| Before blood culture | 83 (10.0) |
| After blood culture | 559 (67.5) |
| Admissions | |
| Admission for observation (<24hrs) | 425 (51.3) |
| Admission to PICU | 10 (1.2) |
| Admission to the pediatric ward | 121 (14.6) |
| Admission to surgical ward | 4 (0.4%) |
| Sent home within 2 hrs | 273 (32.9) |
| Temperature °C, Median (Range) | 38.9 (36-41.4) |
| Duration of Fever (Days), Median (Range) | 2.0 (1-30) |
| Laboratory Results | |
| WBC, Median (Range) (x103/ul) | 11.5 (2.0-30.8) |
| ANC, Median (Range) (x103/ul) | 6.8 (1.0-37.9) |
| CRP, Median (Range) (mg/L) | 20.0 (1.0-417.0) |
Table 1: Patient characteristics.
Results
The results of blood cultures (BC) taken over one year for 828 patients is presented in Table 1.
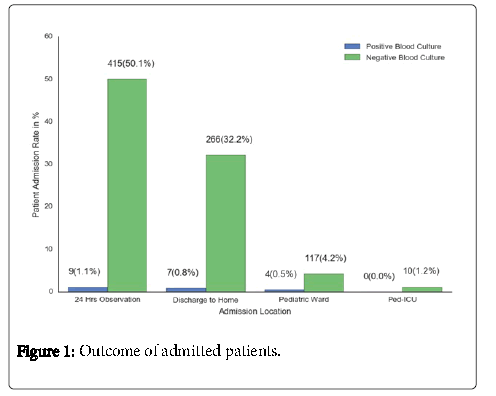
The ages of the patients range from 0.25 to 13.83 years and the median age was 3.55 years. Temperatures ranged from (36.0-41.4°C), with a mean of 38.82°C. The duration of fever ranged from 1 to 30 days, with a mean of 2.8 days. Those patients with a temperature below 38°C, where considered as febrile if there was a history of fever or a consumption of antipyretics prior to admission. Of the 828, 425 (51.3%) were observed in hospital less than 24 hrs and then discharged home. 121 (14.6%) were admitted to the pediatric ward, and 10 (1.2%) admitted to the pediatric intensive care unit (PICU), while 4 (0.4%) were admitted to pediatric surgery.
273 (22.9%) were sent home within 1-2 h, after the initial investigations’ results were available (Figure 1). 83 (10.0%) received oral antibiotic before testing for BC, while 559 (67.5%) were started on empiric antibiotic treatment after the delivery of BC. 808 (97.6%) had negative BC, whereas 20 (2.42%) patients demonstrated a positive BC.
For the group with positive BC, the mean age was 2.90 ± 3.03 years, for negative BC was 3.56 ± 3.17 years, (P=0.3450). The mean temperature in positive and negative BC was 39.27°C and 38.8°C, respectively (P<0.05). 9 of these twenty patients (45.0%) were observed in hospital less than 24 hrs, 4 (20%) were admitted to the pediatric ward, and 2 (10.0%) received oral antibiotic treatment prior to obtaining a BC. 17 (85%) started antibiotic therapy after the BC.
The mean value of WBC in patients with positive BC was 14.97 and in patients with negative BC 12.97, (P=0.4402). The ANC was 8.44 in positive, and 7.87 in negative cultures, (P=0.6484). The CRP was 36.4 in patients with positive BC, while the value in patients with negative BC was higher, 46.99. However, this surprising difference was not significant (P=0.4326).
In summary, Table 2 demonstrates the comparison of the results for groups with positive and negative BC.
| Characteristic | Blood Culture | P-value | |
|---|---|---|---|
| Positive Number (%) | Negative Number (%) | ||
| Gender | |||
| Male | 14 (70.0) | 455 (56.4) | 0.2599 |
| Female | 6 (30.0) | 352 (43.6) | |
| Nationality | |||
| Qatari | 5 (25.0) | 223 (27.6) | 0.7946 |
| Non-Qatari | 15 (75.0) | 584 (72.4) | |
| Age | |||
| ≤3 years | 14 (70.0) | 449 (55.6) | |
| >3 to 6 years | 4 (20.0) | 201 (24.9) | 0.5806 |
| >6 to 10 years | 1 (5.0) | 106 (13.1) | |
| >10 years | 1 (5.0) | 51 (6.3) | |
| Admissions | |||
| Admission for observation <24 hrs) | 9 (45.0) | 415 (51.42) | 0.843 |
| Admission to PICU | 0.0(0.0) | 10 (1.24) | 0.6165 |
| Admission to the pediatric ward | 4 (20.0) | 117 (14.5) | 0.4916 |
| Send home within 2 hrs | 7 (35.0) | 266 (32.9) | 0.8481 |
| Fever | |||
| Degree of fever, Mean ±SD | 39.27 ± 0.91 | 38.8 ± 1.09 | 0.0350* |
| Lab Results | |||
| WBC, Mean ±SD (x103/ul) | 14.25 ± 7.00 | 12.97 ± 12.11 | 0.4402 |
| ANC, Mean ±SD (x103/ul) | 8.44 ± 5.46 | 7.87 ± 5.17 | 0.6484 |
| CRP, Mean ±SD (mg/L) | 36.4 ± 39.5 | 46.99 ± 67.36 | 0.4326 |
| Antibiotic Use | |||
| Before blood culture | 2.0 (10.0) | 81 (10.0) | 0.9956 |
| After blood culture | 17 (85.0) | 541 (67.4) | 0.0903 |
Table 2: Comparison of positive and negative blood culture groups.
Discussion
Over one year we reviewed 828 patients presented to the PED. The patients age more than 3 months up to 14 years old, with mean age of 3.55 ± 3.17. Only 2.42% (20) exhibited positive blood culture. This is in line with previous studies since most of the reviews on blood culture reports have a positive rate of 4-8% [25-29]. A question that rises is to what extent a positive result did change the management of the patients. For example, current guidelines do not support the use of blood culture for patients with the diagnosis of for example asthma or bronchiolitis [30,31]. A substantial part of all patients (273), 33.0%, were send home within 24 hrs, with no significant difference between the groups with negative or positive blood culture. Interestingly, the same proportion of patients in the two groups, positive and negative blood culture, 35.0% and 33.0%, respectively were sent home within two hours. That suggests there were no differences in their clinical conditions. Almost 15% who required admission after more than 24 hrs, and were send to the pediatric ward or PICU, had negative culture results, whereas 20% of those with positive culture were admitted to the pediatric ward, but none to the PICU. The reason for this lack of difference is most likely due to similar clinical presentations between the two groups, and further emphasis the lack of value for a clinical decision by the BC. Furthermore, there were no significant differences in the admissions to the different types of hospital care between the two groups. That indicate physicians had inappropriately and frequently suspected a bacteremia [32] in the group of negative BC. In our study the temperature was significantly higher in the group with positive BC (P<0.001). Therefore, the degree of fever was a clinical feature that was associated with bacteremia. Blood culture investigation in adult ED has been questioned, in particularly in immune-competent patients with a common infection or an infection that can be diagnosed by other means, with the conclusion that the BC was of very limited usefulness [33-35]. In most of the patients that later was confirmed with a positive BC, empiric antibiotic treatment was started more frequently than in patients with a negative BC (P=0.015), illustrating that other clinical factors, e.g. presentation and/or fever were used for the guidance of clinical decision making. However, the figures from this study also demonstrate that antibiotics were prescribed to a large proportion of the patients with negative BC, i.e. 67.5%. Altogether, 77.5% of all patients with suspected infection received antibiotics. A surprising finding was the lack of correlations between BC and the additional blood markers for infections, i.e. ANC, WBC and CRP. The results of these additional laboratory investigations were not correlated to the results of positive or negative BC. However, bacteremia can be present even with a normal white blood cell count [36,37]. Our finding is in contrast to Stathakis and coworkers (2007) who found that a pathological neutrophil count was the strongest predictor to bacteremia in children aged 3-36 months [38]. The difference in results can also be explained by a broader in age range in our study.
CRP has been suggested to be an important predictor of serious bacterial infections [39]. However, in the present study, the analysis of CRP did not demonstrate any difference between the groups with positive and negative blood culture. The most frequent use of CRP has been for respiratory tract infections where its use has demonstrated a reduction in the prescription of antibiotics [40].
Conclusion
Although, blood culture is regarded as the gold standard approach to confirm diagnosis in a child with suspected serious bacterial infection or fever of unknown origin, the rate of bacteremia in a population of children attending an ED is low. This finding questions the policy of blood culture sampling as a “mandatory” measure to obtain diagnosis in this group of patients. Furthermore, the results of BC demonstrated no association with the admission to hospital wards or the prescription of antibiotics.
There is no significant correlation between BC outcome and the result of WBC, ANC and CRP. This is of interest from a practical point view since the results of these laboratories test most often create the foundation for the decision to prescribe antibiotics and/or referral for inpatient care.
Our recommendation is therefore to restrict the ordering of BC to cases where the source of infection is not clear and the clinical picture speaks in favor of a bacterial origin. This is also an important step in order to reduce the costs for laboratory analysis.
Declaration
Acknowledgment: We would like to thank the medical record staff for their assistance in abstracting the medical records, Zakarya Elmabrouk and Mona Elganainy for data collections, and Dr. Prem Chandra (all at Hamad Medical Corporation, Doha), for his contributions to the protocol.
Ethics approval and consent to participate: The study was approved by the Institutional Review Board of Hamad Medical Corporation, Doha.
Availability of data and material: The datasets during and/or analyzed during the current study available from the corresponding author on reasonable request.
Authors' contributions: All authors participated in conceiving and design of the study and helped to draft the manuscript. All conducted the research, and KS coordinated the project. All authors read and approved the final manuscript.
References
- Brockmann VP, Ibarra GX, Silva WI, Hirsch BT (2007) Etiology of acute fever without source in infants consulting at an emergency department. Rev Chilena Infectol 24: 33-39.
- Pratt A, Attia MW (2007) Duration of fever and markers of serious bacterial infection in young febrile children. Pediatr Int 49: 31-35.
- Simon AE, Lukacs SL, Mendola P (2011) Emergency department laboratory evaluations of fever without source in children aged 3 to 36 months. Pediatrics 128: e1368-1375.
- Mansour KM, Kuypers FA, Wang TN, Miller AM, Larkin SK, et al. (2011) Secretory phospholipase A2: a marker of infection in febrile children presenting to a pediatric ED. Am J Emerg Med 29: 1163-1168.
- Nakabayashi M, Adachi Y, Itazawa T, Okabe Y, Kanegane H, et al. (2006) MxA-based recognition of viral illness in febrile children by a whole blood assay. Pediatr Res 60: 770-774.
- Manzano S, Bailey B, Gervaix A, Cousineau J, Delvin E, et al. (2011) Markers for bacterial infection in children with fever without source. Arch Dis Child 96: 440-446.
- Girodias JB, Bailey B (2003) Approach to the febrile child: A challenge bridging the gap between the literature and clinical practice. Paediatr Child Health 8: 76-82.
- Avner JR, Baker MD (2009) Occult bacteremia in the post-pneumococcal conjugate vaccine era: does the blood culture stop here. Acad Emerg Med 16: 258-260.
- Colmenares JP, Craig AS, Chu PS, Schaffner W (2005) Emergency department evaluation of febrile children after the introduction of Prevnar. Tenn Med 98: 184-186.
- Bressan S, Berlese P, Mion T, Masiero S, Cavallaro A, et al. (2012) Bacteremia in feverish children presenting to the emergency department: a retrospective study and literature review. Acta Paediatr 101: 271-277.
- Jager CP, van Wijk PT, Mathoera RB, de Jongh-Leuvenink J, van der Poll T, et al. (2010) Lymphocytopenia and neutrophil-lymphocyte count ratio predict bacteremia better than conventional infection markers in an emergency care unit. Crit Care 14: R192.
- Mace SE, Gemme SR, Valente JH, Eskin B, Bakes K, et al. (2016) Clinical Policy for Well-Appearing Infants and Children Younger Than 2 Years of Age Presenting to the Emergency Department With Fever. Ann Emerg Med 67: 625-639 e613.
- Baraff LJ (2008) Management of infants and young children with fever without source. Pediatr Ann 37: 673-679
- Hall RT, Domenico HJ, Self WH, Hain PD (2013) Reducing the blood culture contamination rate in a pediatric emergency department and subsequent cost savings. Pediatrics 131: e292-297.
- Weddle G, Jackson MA, Selvarangan R (2011) Reducing blood culture contamination in a pediatric emergency department. Pediatr Emerg Care 27: 179-181.
- Laupland KB, Church DL, Gregson DB (2005) Blood cultures in ambulatory outpatients. BMC Infect Dis 5: 35.
- Tokuda Y, Miyasato H, Stein GH (2005) A simple prediction algorithm for bacteraemia in patients with acute febrile illness. QJM 98: 813-820.
- Ehrenstein BP, Jarry T, Linde HJ, Scholmerich J, Gluck T (2005) Low rate of clinical consequences derived from results of blood cultures obtained in an internal medicine emergency department. Infection 33: 314-319.
- Parikh K, Davis AB, Pavuluri P (2014) Do we need this blood culture? Hosp Pediatr 4: 78-84.
- Greenes DS, Harper MB (1999) Low risk of bacteremia in febrile children with recognizable viral syndromes. Pediatr Infect Dis J 18: 258-261.
- Astete JA, Batlle A, Hernandez-Bou S, Trenchs V, Gene A, et al. (2014) Blood culture diagnostic yield in a paediatric emergency department. Eur J Emerg Med 21: 336-340.
- Murillo TA, Beavers-May TK, English D, Plummer V, Stovall SH (2011) Reducing contamination of peripheral blood cultures in a pediatric emergency department. Pediatr Emerg Care 27: 918-921.
- Huang N, Morlock L, Lee CH, Chen LS, Chou YJ (2005) Antibiotic prescribing for children with nasopharyngitis (common colds), upper respiratory infections, and bronchitis who have health-professional parents. Pediatrics 116: 826-832.
- Gille-Johnson P, Hansson KE, Gardlund B (2012) Clinical and laboratory variables identifying bacterial infection and bacteraemia in the emergency department. Scand J Infect Dis 44: 745-752.
- Bates DW, Cook EF, Goldman L, Lee TH (1990) Predicting bacteremia in hospitalized patients. A prospectively validated model. Ann Intern Med 113: 495-500.
- Mellors JW, Horwitz RI, Harvey MR, Horwitz SM (1987) A simple index to identify occult bacterial infection in adults with acute unexplained fever. Arch Intern Med 147: 666-671.
- Pfitzenmeyer P, Decrey H, Auckenthaler R, Michel JP (1995) Predicting bacteremia in older patients. J Am Geriatr Soc 43: 230-235.
- Aronson MD, Bor DH (1987) Blood cultures. Ann Intern Med 106: 246-253.
- Fontanarosa PB, Kaeberlein FJ, Gerson LW, Thomson RB (1992) Difficulty in predicting bacteremia in elderly emergency patients. Ann Emerg Med 21: 842-848.
- Ralston SL, Lieberthal AS, Meissner HC, Alverson BK, Baley JE, et al. (2014) Clinical practice guideline: the diagnosis, management, and prevention of bronchiolitis. Pediatrics 134: e1474-1502.
- Papadopoulos NG, Arakawa H, Carlsen KH, Custovic A, Gern J, et al. (2012) International consensus on (ICON) pediatric asthma. Allergy 67: 976-997.
- Makadon HJ, Bor D, Friedland G, Dasse P, Komaroff AL, et al. (1987) Febrile inpatients: house officers' use of blood cultures. J Gen Intern Med 2: 293-297.
- Kelly AM (1998) Clinical impact of blood cultures taken in the emergency department. J Accid Emerg Med 15: 254-256.
- Howie N, Gerstenmaier JF, Munro PT (2007) Do peripheral blood cultures taken in the emergency department influence clinical management? Emerg Med J 24: 213-214.
- Cisneros JM, Espigado I, Rivero A, Lozano de Leon F, Parra J, et al. (2005) [Empirical antifungal therapy in selected patients with persistent fever and neutropenia]. Enferm Infecc Microbiol Clin 23: 609-614.
- Seigel TA, Cocchi MN, Salciccioli J, Shapiro NI, Howell M, et al. (2012) Inadequacy of temperature and white blood cell count in predicting bacteremia in patients with suspected infection. J Emerg Med 42: 254-259.
- Fu CM, Tseng WP, Chiang WC, Lai MS, Chie WC, et al. (2012) Occult Staphylococcus aureus bacteremia in adult emergency department patients: rare but important. Clin Infect Dis 54: 1536-1544.
- Stathakis T, Acworth JP, Barnett AG (2007) Prediction tool for bacteraemia in children aged 3-36 months. Emerg Med Australas 19: 353-358.
- Sanders S, Barnett A, Correa-Velez I, Coulthard M, Doust J (2008) Systematic review of the diagnostic accuracy of C-reactive protein to detect bacterial infection in nonhospitalized infants and children with fever. J Pediatr 153: 570-574.
- Huang Y, Chen R, Wu T, Wei X, Guo A (2013) Association between point-of-care CRP testing and antibiotic prescribing in respiratory tract infections: a systematic review and meta-analysis of primary care studies. Br J Gen Pract 63: e787-794.
Relevant Topics
- About the Journal
- Birth Complications
- Breastfeeding
- Bronchopulmonary Dysplasia
- Feeding Disorders
- Gestational diabetes
- Neonatal Anemia
- Neonatal Breastfeeding
- Neonatal Care
- Neonatal Disease
- Neonatal Drugs
- Neonatal Health
- Neonatal Infections
- Neonatal Intensive Care
- Neonatal Seizure
- Neonatal Sepsis
- Neonatal Stroke
- Newborn Jaundice
- Newborns Screening
- Premature Infants
- Sepsis in Neonatal
- Vaccines and Immunity for Newborns
Recommended Journals
Article Tools
Article Usage
- Total views: 5320
- [From(publication date):
December-2016 - Aug 14, 2025] - Breakdown by view type
- HTML page views : 4241
- PDF downloads : 1079