Triaging Hospitalization in Threatened Preterm Labor Patients Using a Biochemical Marker and Transvaginal Ultrasound-A Pilot Implementation Study in a Tertiary Center of North India
Received: 03-Oct-2018 / Accepted Date: 17-Dec-2018 / Published Date: 24-Dec-2018 DOI: 10.4172/2376-127X.1000400
Abstract
Background: Hospitalization rates for threatened or arrested preterm labour pains are high but often unnecessary. The main aim of this study was to determine the need for hospitalization in patients with threatened Preterm Labor (PTL) after testing for the presence of Phosphorylated Insulin like Growth Factor Binding Protein-1 (phIGFBP-1) in cervicovaginal secretions followed by cervical length assessment.
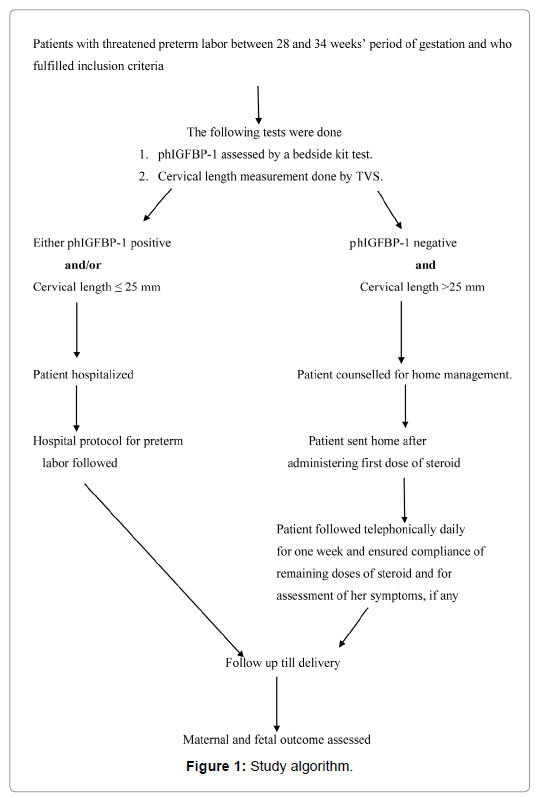
Methods: A prospective study was conducted in a cohort of one hundred patients of threatened PTL. They were evaluated for presence of phIGFBP-1 in cervicovaginal secretions using a bedside kit followed by cervical length measurement by Transvaginal Sonography (TVS). If either phIGFBP-1 test was positive and/or cervical length was less than or equal to 25 mm, the patient was admitted and hospital protocol was followed. If phIGFBP-1 was negative and cervical length was more than 25 mm, then the patient was counselled for home management. All patients were followed till delivery.
Result: Implementation of these tests resulted in hospitalization rate of 16% in patients with threatened PTL which was a reduction by 80% and was statistically significant with p value of <0.001. No patient assigned to home management (n=84) delivered either within 48 h or 7 days of testing. Nine patients (10.7%) delivered between one to four weeks whereas the remaining 75 patients (89.2%) delivered after four weeks. Approximate cost savings varied from INR 1,62,000 to INR 1,536,570 ($2323 to $22030) for 100 patients.
Conclusion: The use of these tests will decrease burden of hospitalization amongst patients thereby resulting in minimising unnecessary treatment and medical expenses.
Keywords: Cervical length; phIGFBP-1; Preterm birth
Abbreviations
phIGFBP-1: Phosphorylated Insulin like Growth Factor Binding Protein-1; TVS: Transvaginal Sonography; PTL: Preterm Labor; POG: Period of Gestation; CL: Cervical Length
Introduction
Preterm labor pain refers to labor pain that occurs before 37 weeks Period of Gestation (POG). Threatened preterm labor is defined as patients with POG less than 37 weeks presenting with pain abdomen with palpable premature uterine contractions (at least one contraction in 10 min) with minimal or no cervical changes and may include other symptoms such as pelvic pressure, backache, menstrual-like cramps, show or shortened cervix [1-3]. Routinely, every patient with threatened preterm labor is hospitalized, even though only a minority of them, around 5% deliver preterm [4]. Hence it is necessary to triage these patients to decide on the subsequent course of management.
In the last decade, the discovery of novel biomarkers has helped in identifying women who would subsequently deliver preterm and need transfer to higher centre thus allowing timely medical intervention and targeted therapeutic treatments which would improve maternal and fetal outcomes. Detection of Fetal fibronectin, phosphorylated Insulin like Growth Factor Binding Protein-1 (phIGFBP-1) in cervicovaginal secretions and cervical length measurement by Transvaginal Sonography (TVS) are investigating modalities that are in clinical use in predicting preterm birth.
Hospitalization rates for threatened or arrested preterm labour pains have increased in the last two decades especially with the use of assisted reproduction techniques. Though prematurity is an important contributor to perinatal morbidity and mortality, the incidence of early preterm delivery (<34 gestational weeks’) is only 1%-3.6% of total births [5]. These unnecessary hospitalizations pose an economic and an emotional burden on patients and their families. Hence it is essential to identify patients with true preterm labour pains which would reduce unnecessary admissions, transfers and referrals thereby decreasing the workload for medical and paramedical professionals. This would be even more relevant in developing and low resource countries like India where the doctor to patient ratio is only 1: 1800 [6].
This analysis was conducted in a tertiary care centre in north India as a pilot operational analysis to ratify an algorithm proposed in a study done earlier in the same institution [7]. The main aim of this study was to determine the need for hospitalization in patients with threatened preterm labor using two parameters viz. phIGFBP-1 in cervicovaginal secretions followed by cervical length measurement by Transvaginal Sonography (TVS).
Method and Materials
A prospective study was conducted in patients who presented with threatened preterm labor over a period of eighteen months between October 2014 and March 2016 in a tertiary care institution in New Delhi. Total of 100 Institutional Review Board (IRB) approved patients with singleton pregnancy ranging from 28 to 34 weeks presenting with symptoms of preterm labor and at least one palpable uterine contraction in ten min (assessed by treating obstetrician), but with minimal or no cervical changes, with intact membranes and no clinical evidence of chorioamnionitis (maternal or fetal tachycardia, febrile illness and uterine tenderness) were included in the study. A written informed consent to participate in the study was taken from all the recruited patients. Patients in active labor (cervical dilatation >3 cm), with bleeding per vaginum, with multiple gestation, having preterm premature rupture of membranes or those with associated comorbidities like GDM, hypertension were excluded from the study. Demographic and clinical details for the patient were entered in a predesigned proforma.
The patients were initially evaluated for phIGFBP-1 in cervical secretions by using a simple and easy bedside kit test named Actim Partus manufactured by Medix Biochemica, Kauniainen, Finland [4]. The kit contained three components (a polyester swab, specimen extraction solution tube and an immunochromatographic dipstick). After recruitment, per speculum examination was done for all patients. A sample was taken from the cervical os by holding the polyester swab for 10 to 15 sec at the level of os. Then the swab was placed in specimen extraction solution tube for 10 sec and swirled around. Later, the dipstick was immersed in this solution until the liquid front reached the result area. Then the result was read as positive if two blue lines appeared (one control and one test line) and negative if only one blue line appeared (control line only). This test has a detection limit of 10 μg/dL.
This was followed by cervical length measurement by Transvaginal Ultrasonography (TVS). Cervical length was measured transvaginally using Philips HD7 ultrasound machine having a 6.5 MHz TVS probe. The patient was examined with empty bladder. The cervical length was obtained by measuring from external to internal os in a longitudinal axis. Three measurements were taken and the shortest of the three values was taken as the final cervical length. Cut off value to decide for admission was cervical length less than or equal to 25 mm.
If either phIGFBP-1 test was positive and/or transvaginal cervical length was less than or equal to 25 mm, then the patient was admitted and hospital protocol for preterm labor was followed for further management. Hospital protocol includes information to senior obstetrician on call and neonatal team, administration of corticosteroids, maternal and fetal monitoring, tocolysis in case of persistent uterine contractions to provide time for completion of corticosteroid regime (Nifedipine is the first line tocolytic agent used) (Figures 1 and 2).
If phIGFBP-1 was negative and transvaginal cervical length measurement was more than 25 mm, then the patient was counselled for home management. If the patient gave consent, then she was sent home after administering first dose of steroid (dexamethasone 6 mg intramuscular). The patient was advised to take remaining three doses of dexamethasone, 12 h apart in a nearby clinic or nursing home as part of out of hospital management. The patient was followed telephonically daily for one week to ensure that the course of steroid was completed and also to enquire regarding pain or presence of any other symptoms. Administration of steroid was done in all cases as this is the policy being routinely followed in the institution and it was felt that in ethical interest the baby should not be in jeopardy.
All patients were followed till delivery to assess maternal and fetal outcome. After delivery, the birth weight, need of neonatal intensive care and perinatal outcome were observed.
The algorithm used was similar to the one proposed in an earlier study [7]. The data obtained was entered in Microsoft Excel and analysed in SPSS version 17 and analysed using appropriate statistical test. Quantitative variables were determined by unpaired t test or Mann Whitney test whereas qualitative variables were determined by Chi-square test or Fisher exact test. p value less than 0.05 was considered to have a significant difference.
Results
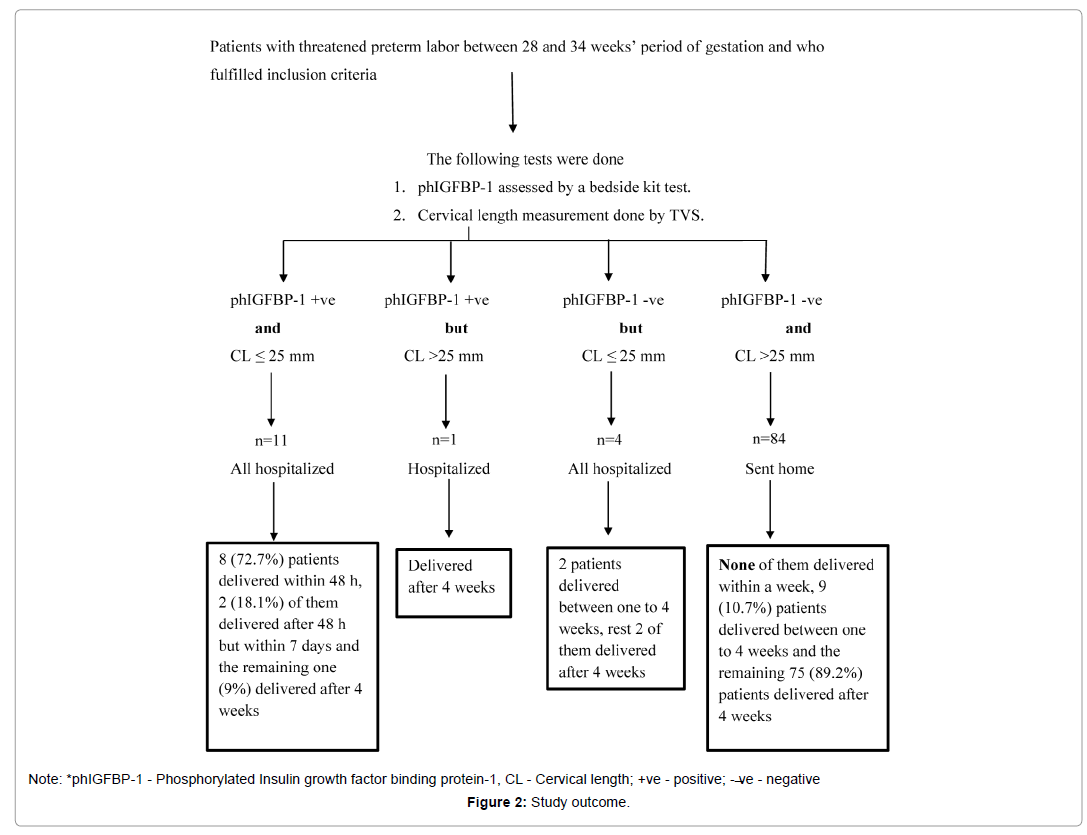
Demographic characteristics of the study group based on their period of gestation at delivery are shown in Table 1. The patient outcomes in relation to test results are shown in Table 2. There were eleven patients with both phIGFBP-1 positive and cervical length less than or equal to 25 mm. Of these, eight (72.7%) delivered within 48 h, two patients (18.1%) delivered after 48 h but within seven days and only one patient (9%) delivered after four weeks of initial presentation and testing (at 37+2 weeks). Amongst the patients assigned to home management three required readmission but they all delivered after 36 weeks (Table 3).
| S. No | Demographic characteristics | Early preterm<34 weeks (n=9) | Late preterm 34+0-36+6 weeks (n=15) | Term>37 weeks (n=76) | |
|---|---|---|---|---|---|
| 1 | Parity | P0 | 6 | 6 | 32 |
| P1 | 3 | 6 | 30 | ||
| P2 and above | 0 | 3 | 14 | ||
| 2 | Status of external Cervical os |
Open | 2 | 3 | 6 |
| Closed | 7 | 12 | 70 | ||
| 3 | Mean maternal age (years) | 23.0 ± 2.55 | 24.53 ± 2.66 | 24.94 ± 4.02 | |
| 4 | Mean gestational age at enrolment (weeks) | 31.2 ± 1.51 | 32.65 ± 1.37 | 32.20 ± 1.64 | |
| 5 | Mean gestational age at delivery (weeks) | 31.69 ± 1.48 | 36.26 ± 0.92 | 38.9 ± 0.77 | |
| 6 | Mean birth weight (grams) | 1583 ± 414 | 2441 ± 482 | 2926 ± 383.9 | |
Table 1: Demographic characteristics of the study group based on their period of gestation at delivery.
| Combined Parameters | Category of Management |
Total number of patients (n) | Delivered within 48 h (n) | Delivered after 48 h but within 7 days (n) | Delivered between one to 4 weeks (n) | Delivered after 4 weeks (n) | |
|---|---|---|---|---|---|---|---|
| phIGFBP-1 | CL | ||||||
| Positive and | = 25 mm | Hospital | 11 | 8 | 2 | 0 | 1 |
| Positive but | >25 mm | Hospital | 1 | 0 | 0 | 0 | 1 |
| Negative but | = 25 mm | Hospital | 4 | 0 | 0 | 2 | 2 |
| Negative and | >25 mm | Home | 84 | 0 | 0 | 9 | 75 |
| Total | - | - | 100 | 8 | 2 | 11 | 77 |
Table 2: Outcome of patients in relation to combination of test results.
| Need for readmission within one week | Frequency (n) | Time interval between assessment and readmission | Percent (%) | POG at delivery (weeks) |
|---|---|---|---|---|
| Recurrence of pain | 2 | 12-48 h | 2.4% | 36+5, 38+0 |
| For gastroenteritis | 1 | 7-48 h | 1.2% | 38+5 |
| Total | 3 | 3.6% |
Table 3: Details of need for subsequent admission within one week in home management patients (n=84).
Comparison between home and hospital managed patients is depicted in Table 4. None of the patients assigned to home management delivered either within 48 h or within 7 days of testing. Though the home management group does show some preterm deliveries they all delivered much after testing. This is of relevance as the validity of the test is for within seven days of testing. Nine patients (10.7%) delivered between one to four weeks and 75 patients (89.2%) delivered after four weeks. The statistical parameters of each test for predicting delivery within seven days, individually and in combination, is shown in detail below (Table 5).
| Parameters | Home Management (n=84) | Hospital Management (n=16) |
|---|---|---|
| Delivery within 48 h (n) | Nil | 8 |
| Delivery within 7 days but>48 h (n) | Nil | 2 |
| Delivery between 7-14 days(n) | 1 | Nil |
| Delivery between 15-21 days (n) | 2 | 1 |
| Delivery between 22-28 days (n) | 6 | 1 |
| Delivery after more than 28 days (n) | 75 | 4 |
| Gestational age at delivery | ||
| Early pre-term (<34 weeks) | 1 | 8 |
| Late pre term (34-36+6 weeks) | 11 | 4 |
| Term (37-40 weeks) | 60 | 4 |
| >40 weeks | 12 | Nil |
Table 4: Comparison of outcome of hospitalized patients versus those assigned to home management.
| Statistical parameters | phIGFBP-1 +ve [n=12] (95% CI) |
CL = 25 mm [n=15] (95% CI) |
phIGFBP-1 +ve and CL = 25 mm [n=11] (95% CI) |
|---|---|---|---|
| Sensitivity (%) | 100 | 100 | 100 |
| (69.2% to 100%) | (69.2% to 100%) | (69.2% to 100%) | |
| Specificity (%) | 97.8 | 94.4 | 98.9 |
| (92.2% to 99.7%) | (87.5% to 98.2%) | (93.6% to 100%) | |
| PPV (%) | 83.3 | 66.7 | 90.9 |
| (56% to 95.2%) | (46% to 82.4%) | (58.8% to 98.6%) | |
| NPV (%) | 100 | 100 | 100 |
| Positive likelihood ratio | 45.45 | 17.9 | 90 |
| (4.9 to 17.6) | (7.7 to 42.2) | (12.11 to 596.51) | |
| Negative likelihood ratio | 0 | 0 | 0 |
Note: *phIGFBP-1 - Phosphorylated Insulin growth factor binding protein-1, CL - Cervical length, +ve – Positive, -ve – Negative.
Table 5: Statistical parameters of various tests for predicting delivery within seven days.
Discussions
The identification of women at high risk of preterm delivery remains a major challenge. Patients with threatened preterm labor are generally admitted, irrespective of whether the patient is in labour or not, to improve perinatal morbidity and mortality. This is because biochemical marker test is not done routinely in clinical practice and cervical length measurement is difficult to perform due to limited availability of resources in developing countries like ours. Of these admitted patients, hardly any deliver preterm. Various biochemical tests and ultra-sonographic parameters that aid in predicting preterm labour have been studied since many decades with varying degrees of accuracy. In patients presenting with threatened preterm labor, the outcome measure of relevance is to diagnose whether patient will deliver within the next 48 h or seven days as the clinical dilemma revolves around the issue of whether the patient is truly in labour or not. Therefore, there is a need to triage the patient regarding need for hospitalization in a unit with facilities for neonatal intensive care and decision regarding administration of tocolytics. This exercise was conducted to identify the true requirement of hospitalization for patients with threatened preterm labor using results of biochemical predictor (phIGFBP-1) and cervical length.
Two studies showed that admissions for threatened preterm labour had led to unnecessary expenses and exploitation of health care [8,9].
Liu et al. did a study to examine the incidence and trends of hospitalization during pregnancy among Canadian women. Even though the overall antenatal hospitalization ratio calculated per 100 deliveries declined by 43%, from 24.0 per 100 deliveries between 1991 and 1992 to 13.6 between 2002 and 2003, threatened preterm labour remained to be one of the five most common causes for antenatal hospitalization [10].
Yost et al. did a study to compare whether hospitalization of women with arrested preterm labour had an effect on period of gestation at delivery when compared with women discharged home. Among the hospitalized women, 71% reached 36 weeks or greater, compared with 72% of those discharged home. They concluded that outpatient management of women with arrested preterm labour and intact membranes had no association with the rate of preterm birth [11].
In 2010, a similar study was done in US by Rose et al. on patients with symptoms of preterm labor [12]. They triaged admissions using a standard protocol using cervical length measurement and fetal fibronectin assay and found that hospital admission rate was reduced by 56%. On contrary to that study, this study was done with an algorithm using phIGFBP-1 (instead of fetal fibronectin) and cervical length measurement. In this study, the hospitalization rate was only 16% in patients with threatened preterm labor contrary to current practice where all patients with threatened preterm labor are admitted. Using these tests, the hospitalization rate was reduced by 80% which was statistically significant with p value <0.001.
Delivery outcome details are shown in Table 4. Only ten of sixteen hospitalized patients delivered within a week of testing positive and others later, it shows that hospitalisation could have been avoided in those patients also who had only one of the tests abnormal as these ten patients who delivered had both tests positive. Thus hospitalization rate could be even further decreased (Table 4).
In patients who were sent home, the need for subsequent admission was 3.6%. These patients continued to have subjective perception of pain and hence were subsequently admitted. However, all of them delivered after five weeks of initial testing. This proved the accuracy of results of phIGFBP-1 and cervical length as hospitalization could have been avoided in them also.
In patients with home management, only one patient delivered before 34 weeks. Even though she delivered an early pre-term neonate, she went into true labour after four weeks of testing as she had been recruited between 29+0 and 29+6 weeks. This further proves the accuracy of testing for both parameters.
The combination of phIGFBP-1 and cervical length had a statistically significant p value of <0.001 in predicting delivery both within 48 h and seven days from testing. In these patients with both tests abnormal, the mean gestational age at delivery was 32.58 weeks and the rate of neonatal intensive care admission was 45.45% which was also statistically significant, having a p value of 0.001.
In India, the approximate cost for 48 h hospitalization varies from INR 2000 to INR 18,970 ($ 30 to $272) depending upon the type of hospital where the patient is evaluated. Therefore, for 100 patients cost would range from INR 200,000 to INR 1,897,000 ($2867 to $27,196). In this study, the hospitalization rate was reduced by 80%. The cost savings approximately varied from INR 1,62,000 to INR 1,536,570 ($2323 to $22030) for 100 patients. This was a very significant reduction in our setup or in low resource countries.
Fetal fibronectin is widely studied biochemical marker to predict preterm birth which is also recommended in various guidelines for management of preterm labor. However, there are few limitations regarding its regular use. The procedure to test fetal fibronectin requires a separate analyser and also it is costly. It cannot be tested in patients who had sexual intercourse in the last 24 h. However, phIGFBP-1 overcomes these limitations as it is less expensive, simple, bedside kit test which is unaffected by urine or presence of semen. Various studies had also suggested that phIGFBP-1 could be used as a substitute to fetal fibronectin.
Riboni et al. in 2011 compared phIGFBP-1 and fetal fibronectin and found that the former was better in predicting preterm birth <34 weeks because of high odds ratio (23.61 vs 3.97) [13]. Then a systematic review and meta-analysis done by Conde-Agudelo et al. in 2016 showed that phIGFBP-1 had a limited accuracy in predicting symptomatic preterm labor patients who will not deliver within next 48 h. According to this study, the pooled sensitivity and specificity for predicting delivery within 7 days were 67% and 77% respectively [14]. However, a study by Brujin et al. in 2016 analysed that combination of phIGFBP-1 with cervical length was equivalent to combination of cervical length and fetal fibronectin in predicting preterm delivery within 7 days [15]. Melchor et al. in 2018 did a meta-analysis using phIGFBP-1 and fetal fibronectin and found that pooled sensitivity, specificity, positive predictive value, negative predictive value, positive likelihood and negative likelihood ratios of phIGFBP-1 for predicting delivery within 7 days were 93%, 76%, 35.2%, 98.7%, 3.8% and 0.09% while for fetal fibronectin are 58%, 84%, 34%, 93.3%, 3.63% and 0.50%. This showed that sensitivity and negative predictive value of phIGFBP-1 is better than fetal fibronectin [16]. All these indicate that phIGFBP-1 could be used as an alternative to fetal fibronectin due to cheaper cost in minimal resource settings [17-19].
Table 6 shows a comparison of various studies of phIGFBP-1 for predicting preterm birth. The present study has a high sensitivity, specificity, PPV and NPV when compared to the previous studies for predicting delivery within 7 days. However, for predicting delivery at less than 37 weeks, the current study has only high specificity with fall in sensitivity and NPV [20,21]. This may be because in the current study, patients were mainly enrolled between 28 and 34 weeks and hence patients who had negative phIGFBP-1 test have also delivered at period of gestation less than 37 weeks even though that was after a month of initial testing. Though they were in the category of preterm by virtue of POG, neonatal outcome was not in jeopardy (Table 6).
| Prediction of delivery | Study | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) | Positive likelihood ratio | Negative likelihood ratio |
|---|---|---|---|---|---|---|---|
| Within 7 days | Ting et al. [17] | 69 | 78 | 39 | 92 | - | - |
| Riboni et al. [13] | 54.1 | 72.1 | 17.4 | 93.5 | - | - | |
| Cooper at al. [18] | 33 | 74 | 2 | 98 | 1.28 | 0.9 | |
| Nikolova et al. [19] | - | - | 18.6 | 98.2 | 3.1 | 0.3 | |
| Current study | 100 | 97.8 | 83.3 | 100 | 45.45 | 0 | |
| Less than 37 weeks | Lembet et al. [20] | 89.5 | 94.1 | 94.4 | 88.9 | - | - |
| Altinkaya et al. [21] | 70 | 87.5 | 56 | 92.5 | - | - | |
| Cooper et al. [18] | 39 | 76 | 24 | 86 | 1.63 | 0.8 | |
| Current study | 41.6 | 97.5 | 83.3 | 84.9 | - | - |
Table 6: Comparison of various studies using phIGFBP-1 for predicting preterm birth.
A study done by Brik et al. in 2010 at Spain showed that phIGFBP-1 and cervical length were good predictors individually, however their combination did not improve preterm delivery prediction rates [22]. A study by Eroglu et al. in 2007 showed that when phIGFBP-1 and cervical length <25 mm were combined to predict preterm birth within 7 days, the specificity and PPV increased [23]. The same results were found in our study also, when comparing the statistical parameters of only positive phIGFBP-1 test with combination of positive phIGFBP-1 and short cervical length, sensitivity and negative predictive value was 100% for both former and the latter. However, there was minimal increase from 83.3% to 90.9% in positive predictive value for the combination when compared to phIGFBP-1 alone [24]. Table 7 shows the comparison of various studies using combination of phIGFBP-1 and cervical length. In the current study, sensitivity and NPV remained almost similar but this study had high specificity and positive predictive value compared to others (Table 7).
| Study | Sensitivity (%) | Specificity (%) | PPV (%) | NPV (%) |
|---|---|---|---|---|
| Danti et al. [24] | 100 | 73 | 8 | 100 |
| Azlin et al. [25] | 80 | 97.8 | 80 | 97.8 |
| Current study | 100 | 98.9 | 90.9 | 100 |
Table 7: Comparison of studies that used combination of phIGFBP-1 and cervical length less than or equal to 25 mm for prediction of preterm birth within 7 days.
The PPV of cervical length alone is only 66.7%. In many centres this cervical length measurement is being utilized for determining hospitalization but this low PPV means that many who are admitted do not actually deliver hence leading to unnecessary hospitalisations even if not universal [25].
NICE guidelines on preterm labor and birth recommend cervical length measurement in patients with symptoms of preterm labor with POG>30 weeks and fetal fibronectin to be done only if TVS for cervical length could not be performed and also they have proposed not to use both in combination for prediction of preterm labor [26]. The American Congress of Obstetricians and Gynecologists (ACOG) recommends using cervical length measurement or fetal fibronectin alone or in combination to diagnose preterm labor [27].
In this study, Number Needed to Treat (NNT) was 1.42. This means that of 1000 patients sent home, 1.42 patients may deliver preterm and that would possibly also be after a fortnight of testing. Hence according to our pilot study, it appears that a positive test of phIGFBP-1 alone could also be taken as a good predictor of preterm birth. This is of special relevance in centres where TVS may not be able to be performed as there was only minimal increase in positive predictive value with the combination which may not have much significant clinical implication. This may have repercussion in context of low resource settings as phIGFBP-1 can be evaluated by a simple bedside test which can be done even by a trained paramedical person in rural hospitals whereas facility and expertise for measurement of cervical length by TVS may have only limited availability.
The limitation of this study is its small sample size due to financial constraints in procurement of testing kits. It is suggested that this same algorithm be followed in a randomized controlled study having larger number of patients before change of common clinical practice can be recommended.
Conclusion
This study showed that hospitalization can be avoided in patients with threatened preterm labor having a negative test of phIGFBP-1 in cervicovaginal secretions and cervical length more than 25 mm. The use of these tests will decrease burden of hospitalization of patients presenting with threatened preterm labor thereby resulting in minimising unnecessary treatment and medical expenses. This study also showed good accuracy in identifying those patients of threatened preterm labor who are likely to deliver preterm who can then be referred to a higher centre to optimise fetal outcome.
Ethical Approval
IRB approval was accorded from our institution Maulana Azad Medical College, New Delhi, India during a meeting held in September 2014 and the reference number is F.No./11/IEC/MAMC/2011/147 dated 5th December 2014.
Acknowledgment
We acknowledge that our institution, Maulana Azad Medical College, New Delhi, has granted some partial funding for this study
References
- Iams JD, Creasy RK (2009) Preterm labor and delivery. In: Creasy RK, Resnik R, Iams JD (eds), Maternal-fetal medicine: Principles and practice. 6th edition, Philadelphia: Saunders.
- Heng YJ, Pennell CE, Chua HN, Perkins JE, Lye SJ (2014) Whole blood gene expression profile associated with spontaneous preterm birth in women with threatened preterm labor. Plos One 9: e96901.
- Hezelgrave NL, Shennan AH (2017) Threatened and actual preterm labor. In: James D, Steer P, Weiner C, Gonik B, Robson S (eds), High risk pregnancy: Management options: Five-year Institutional subscription with online updates. 5th edition. Cambridge: Cambridge University Press. Pp: 1624-1654.
- Honest H, Bachmann LM, Gupta JK, Kleijnen J, Khan KS (2002) Accuracy of cervicovaginal fetal fibronectin test in predicting risk of spontaneous preterm birth: Systematic review. BMJ 325: 301.
- Goldenberg RL, Culhane JF, Iams JD, Romero R (2008) Epidemiology and causes of preterm birth. Lancet 371: 75-84.
- Deo MG (2013) Doctor population ratio for India-The reality. Indian J Med Res 137: 632-635.
- Tripathi R, Tyagi S, Yadav P, Meenoo S, Shah S, et al. (2017) Evaluation of phosphorylated insulin like growth factor binding protein-1 and sonographically measured cervical length for prediction of preterm birth in threatened preterm labor: A clinical approach. Int J Preg Child Birth 2: 00024.
- Nicholson WK, Frick KD, Powe NR (2000) Economic burden of hospitalizations for preterm labor in the United States. Obstet Gynecol 96: 95-101.
- Lucovnik M, Chambliss LR, Garfield RE (2013) Costs of unnecessary admissions and treatments for "threatened preterm labor". Am J Obstet Gynecol 209: 217.e1-3.
- Liu S, Heaman M, Sauve R, Liston R, Reyes F, et al. (2007) An analysis of antenatal hospitalization in Canada, 1991-2003. Matern Child Health J 11: 181-187.
- Yost NP, Bloom SL, McIntire DD, Leveno KJ (2005) Hospitalization for women with arrested preterm labor: A randomized trial. Obstet Gynecol 106: 14-18.
- Rose CH, McWeeney DT, Brost BC, Davies NP, William J (2010) Cost-effective standardization of preterm labor evaluation. Am J Obstet Gynecol 203: 250.e1-5.
- Riboni F, Vitulo A, Dell’avanzo M, Plebani M, Battagliarin G, et al. (2011) Biochemical markers predicting pre-term delivery in symptomatic patients: Phosphorylated insulin-like growth factor binding protein-1 and fetal fibronectin. Arch Gynecol Obstet 284: 1325-1329.
- Conde-Agudelo A, Romero R (2016) Cervical phosphorylated insulin-like growth factor binding protein-1 test for the prediction of preterm birth: A systematic review and metaanalysis. Am J Obstet Gynecol 214: 57-73.
- Bruijn MC, Vis JY, Wilms FF, Oudjik MA, Kwee A, et al. (2016) Comparison of the actim partus test and the fetal fibronectin test in the prediction of spontaneous preterm birth in symptomatic women undergoing cervical length measurement. Eur J Obstet Gynecol Reprod Biol 206: 220-224.
- Melchor JC, Khalil A, Wing D, Schleussner E, Surbek D (2018) Prediction of preterm delivery in symptomatic women using PAMG-1, fetal fibronectin and phIGFBP-1 tests: Systematic review and meta-analysis. Ultrasound Obstet Gynecol 52: 442-451.
- Ting HS, Chin PS, Yeo G, Kwek K (2007) Comparison of bedside test kits for prediction of preterm delivery: Phosphorylated insulin-like growth factor binding protein-1 (pIGFBP-1) test and fetal fibronectin test. Ann Acad Med Singapore 36: 399-402.
- Cooper S, Lange I, Wood S, Tang S, Miller L, et al. (2012) Diagnostic accuracy of rapid phIGFBP-I assay for predicting preterm labor in symptomatic patients. J Perinatol 32: 460-465.
- Nikolova T, Uotila J, Nikolova N, Bolotskikh VM, Borisova VY, et al. (2018) Prediction of spontaneous preterm delivery in women presenting with premature labor: A comparison of placenta alpha microglobulin-1, phosphorylated insulin-like growth factor binding protein-1 and cervical length. Am J Obstet Gynecol 219: 610.e1-6.
- Lembet A, Eroglu D, Ergin T, Kuscu E, Zeyneoglu H, et al. (2002) New rapid bed-side test to predict preterm delivery: Phosphorylated insulin-like growth factor binding protein-1 in cervical secretions. Acta Obstet Gynecol Scand 81: 706-712.
- Altinkaya O, Gungor T, Ozat M, Danisman N, Mollamahmutoglu L (2009) Cervical phosphorylated insulin-like growth factor binding protein-1 in prediction of preterm delivery. Arch Gynecol Obstet 279: 279-283.
- Brik M, Hernández AI, Pedraz CC, Perales A (2010) Phosphorylated insulin-like growth factor binding protein - 1 and cervical measurement in women with threatening preterm birth. Acta Obstet Gynecol Scand 89: 268-274.
- Eroglu D, Yanik F, Oktem M, Zeyneloglu HB, Kuscu E (2007) Prediction of preterm delivery among women with threatened preterm labor. Gynecol Obstet Invest 64: 109-116.
- Danti L, Prefumo F, Lojacono A, Corini S, Testori A, et al. (2011) The combination of short cervical length and phIGFBP -1 in the prediction of preterm delivery in symptomatic women. J Matern Fetal Neonatal Med 24: 1262-1266.
- Azlin MI, Bang HK, An LJ, Mohamad SN, Mansor NA, et al. (2010) Role of phIGFBP-1 and ultrasound cervical length in predicting pre-term labour. J Obstet Gynaecol 30: 456-460.
- Committee on Practice Bulletins Obstetrics (2016) Practice bulletin No.171: Management of preterm labor. Obstet Gynecol 128: e155-164.
Citation: Meenoo S, Tripathi R, Tyagi S, Ramji S, Shah S, et al. (2018) Triaging Hospitalization in Threatened Preterm Labor Patients Using a Biochemical Marker and Transvaginal Ultrasound-A Pilot Implementation Study in a Tertiary Center of North India. J Preg Child Health 6:400. DOI: 10.4172/2376-127X.1000400
Copyright: © 2018 Meenoo S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6532
- [From(publication date): 0-2019 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 5560
- PDF downloads: 972