Unclassified Tibial Hemimelia-A Case Report
Received: 15-Apr-2018 / Accepted Date: 26-Apr-2018 / Published Date: 03-May-2018 DOI: 10.4172/2329-910X.1000266
Abstract
Tibial hemimelia is an uncommon longitudinal limb deficiency disorder involving the osseous and soft tissue components of the medial part of the leg. It is a syndrome of partial to complete absence of tibia at birth. Because of wide spectrum of presentation of the condition, many authors have tried to classify but none of the classification covers all the variations of tibial hemimelia. The case report presented here is a case of tibial hemimelia with bifurcated ankle having separate skin cover distal end of tibia fibula. This type of tibial hemimelia cannot be classified into any of the category; so far existing classification system is available. Further research is needed to develop a classification system which can include this type of tibial hemimelia.
Keywords: Tibial hemimelia; Club hand; Amputation
Introduction
Tibial hemimelia is a rare congenital condition with an incidence of 1 in 1 million live births [1]. It is characterized by deficiency of tibia with relatively intact fibula. The condition is less common in comparison to fibular and femoral deficiencies in lower extremity but more frequently seen in syndromic children. The condition is associated with marked shortening of the involved extremity with a severe equinovarus deformity [2]. The defect could be either complete or incomplete and present as a solitary disorder or as a part of more complex malformation syndrome [3].
There may be total or partial, unilateral or bilateral tibial deficiency. The incidence of total and unilateral presentation is more frequent with right limb commonly affected than left. In partial defect, distal end of the tibia is frequently absent. In bilateral cases, there may be total absence on both sides, or total on one side and partial on other. Males are predisposed than females. Though the family history is usually negative for congenital abnormalities and other diseases, there is considerable chance of occurrence of congenital defect of tibia or of other abnormalities, in near or remote relatives. Some case of tibial hemimelia is genetically transmitted, whereas others are sporadic [3]. Few syndromes such as tibial hemimelia foot polydactyli triphalangeal thumb syndrome (Werner syndrome), tibial hemimelia split hand/foot syndrome, and tibial hemimelia with radial agenesis syndrome are considered to be transmitted as autosomal dominant. In others such as tibial hemimelia cleft lip/palate syndrome, tibial hemimelia split hand/ foot syndrome, and autosomal recessive inheritance is suggested [4]. Hence abnormalities commonly associated with tibial hemimelia include polydactyly, club hand, radio-ulnar synostosis, bifid femur, cleft lip or palate. Because of varied presentation of condition different authors have tried to classify the condition but none of the classification could include all the variations of tibial hemimelia specially associated upper limb abnormalities. The reported case here is a case of tibial hemimelia which cannot be classified in any of the category of its existing classification system.
Case Report
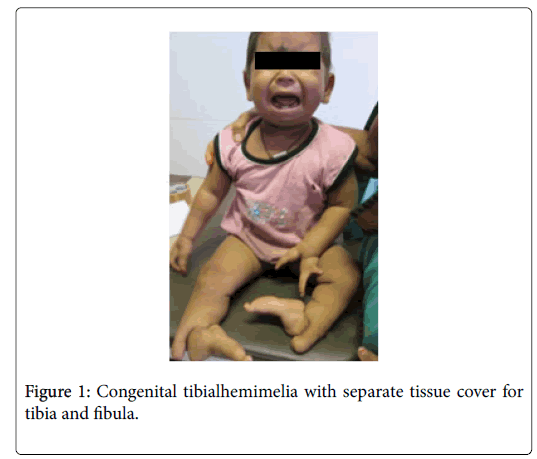
A 10-month-old male child presented by parents complaining of deformity of both legs, feet and hands present at birth. The child was born as a full term baby of 32 years old mother. The child’s birth weight was 3.1 kg. Her antenatal period was mostly uncomplicated except history of 1 week of non-specific fever at 1st trimester of her pregnancy for which chest X-ray was done. She had no history of diabetes or hypertension or use of any teratogenic drugs. There is no consanguity among parent. On examination of the child, both the legs were comparatively shorter in comparison to trunk. Both the feet are proximally migrated, sole supinated through 180 degree with severe varus deformity. Feet were significantly smaller with absence of first ray of feet (Figure 1). There was absolutely no movement at sub talar or mid foot joints and passive pronation of foot was not possible. Foot was in equinus and further planterflexion was possible to some extent but there was not even a trace of dorsiflexion movement. The distal part of leg appeared bifurcated with separate tissue and skin cover over that (Figure 2).
Both the thighs have normal length and appearance. Quadriceps power of both the side was adequate with active extension against gravity. No fixed flexion deformity around knee. No sensory deficit over foot and leg on either side. However dorsalispedis arterial pulsation was not palpable on both the sides.
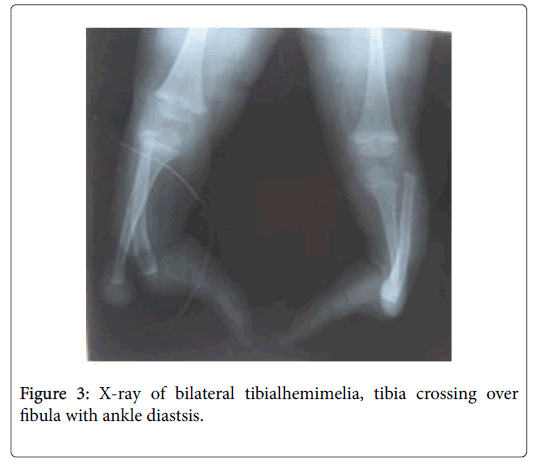
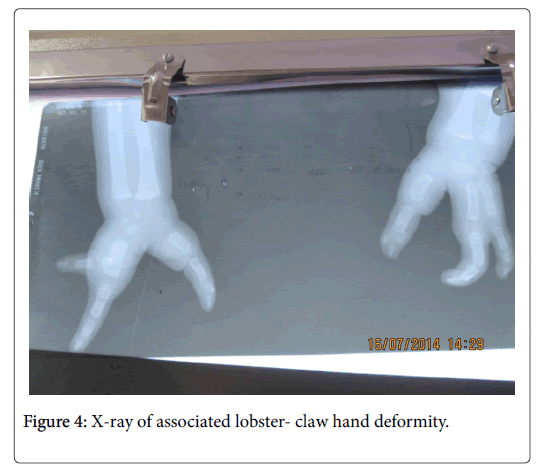
Both the upper limb presented with V shaped split hand deformity with absence of middle ray. Bilateral elbow, shoulder and hip joints are clinically normal. No orofacial abnormalities noted. Radiographic evaluation of both the legs and feet showed proximally displaced fibula with diastasis of both proximal and distal tibiofibular joint. At the distal third of leg, the tibia crossed fibula and took its position on lateral side, leaving the talus to form a pseudoarthrosis with an enlarge distal fibula. There was no true ankle joint. The distal tibial physis was absent and bones of the feet were few in number with features of tarsal coalition (Figure 3). The radiograph of pelvis and hip were normal. Radiographic evaluation of both the hand showed absence of both the central metacarpals with absence of corresponding digits (Figure 4).
A thorough discussion was made with parents regarding various treatment options. Advantages and disadvantages of different methods of management including orthotic alone, amputation followed by prosthetic treatment, limb reconstruction procedure were explained to the parent. Looking towards the bony abnormalities, none of the reconstructive procedure could provide a promising result. Amputation below knee level would have been best for the child. Because of social and cultural issues parent did not give consent for amputation. No surgical reconstruction was possible for the child and fitment of any ambulatory appliances could not be possible as the child was too young to use.
However in the series of 21 cases by Schoenecker et al. [5], all the limbs had either knee disarticulation or Syme amputation after tibial fusion.
Discussion
The first simplified classification for tibial hemimelia was known by Jones classification [6] which divide tibial hemimelia with four categories depending on radiological complete absence, partial absence or reduction in length. Kalamachi et al. [7] did thorough evaluation of initial films and assessment of changes with growth lead to classify these patients into three types with different degrees of tibial deficiency. These types were considered in conjunction with their clinical data and were further characterized to total absence tibia (type I), distal tibial aplasia (type II), dysplasia of distal tibia with diastasis of distal tibiofibular joint. Their study also showed most frequent hand anomaly was split hand deformity. All these classifications were based on X-ray evaluation of tibia, without giving much attention to tibial anlages or cartilage caps which are not visible on X-ray. Detection of a cartilaginous anlage by ultrasonography or MRI is of considerable clinical significance. If the cartilaginous cap comes in contact with corresponding joint, it matures completely to an osseous structure, including growth plates, because of functional loading. The ossification is often significantly delayed for 3-4 years. Then the earlier radiological type of tibialhemimelia may change to different type. Michael [8] modified the earlier terminology tibial aplasia to tibial agenesia. Weber developed a new classification system where the cartilaginous anlage plays a key role. He divides the condition to seven categories and each category subdivided to with or without tibial anlage. This classification system has therapeutic value. Paley’s classification with subtypes further spreads the spectrum of tibial hemimelia [9]. However none of the classification system does include any of associated limb abnormalities which are of therapeutic importance. Victor et al. reported association of vertebral anomaly with tibial hemimelia as association of hemi vertebra is not a part of any of described syndrome complex.
The case presented here does not fulfill the criteria of any recognized syndrome complex. There is complete diastasis of distal tibiofibular joint and separate soft tissue cover for the distal tibia and fibula. Tibia is crossing at the middle of fibula to lateral side . Foot is aligned with fibular end. However it can be considered as a variant of Jone’s type IV or can be placed in sub type of Paley’s type 2 in which foot is usually positioned between the divergent tibia and fibula due to absence of tibial plafond [10]. In the current case foot position is different from the classical Paley’s type 2 variety. All the classification systems have ignored the associated limb abnormalities which really has an overall relation with ultimate functional recovery. Presence of split hand deformity of the case presented here will largely concern in donning and doffing of prosthesis if amputation is chosen as the definite procedure for this case. However more detail research is required on such type of unclassified tibial hemimelia to find out a place in a new classification system with due attention to associated upper limb abnormalities.
Conclusion
Congenital abnormalities present in a wide spectrum, sometime not fit to any standard classification system and the management protocol becomes controversial. A number of surgical procedures are described in literature but none of them can give a promising result. A comprehensive rehabilitation protocol is required considering the functional limitations and ambulatory difficulties. A corrective orthosis, extension prosthesis, shoe compensation or prosthesis after amputation is required in almost all the conditions associated with the use of some walking aids. Upper limb function plays a major role for use of those walking aids. Associated hand abnormalities and foot position of lower limb makes the case unique to rethink about the plan of management. Counseling of the parent plays a vital role on overall management.
Acknowledgement
No financial support has been received from any source.
Conflict of Interest
There are no conflicts of interest.
References
- Palazzi FF, Bendahan J, Rivas S (1998) Congenital deficiency of the tibia: A report on 22 cases. J Pediatric Orthop B 7: 298–302.
- Rozbruch SR, Ilizarov S (2007) Tibial hemimelia limb lengthening and reconstructive surgery. New York Information Health Care, NY, USA. Â pp: 429-447.
- Matsuyama J, Mabuchi A, Zhang J, Lida A, Ikeda T, et al. (2003) A pair of siblings with tibial hemimelia born to phenotypically normal parents. J Human Genetics. 48: 173-176.
- Costa RA (1987) Tibial hemimelia-Cleft lip/palate in a Brazilian child born to consanguineous parents. Am J Med Genetics 28: 325-329.
- Schoenecker PL, Capelli AM, Millar EA, Sheen MR, Haher T (1989) Congenita deficiency tibia. J Bone and Joint Surg Am 71: 278-287.
- Jones D, Barnes J, Liloyd Roberts G (1978) Congenital aplasia and dysplasia with intact fibula: Classification and management. J Bone Joint Surg 60: 13-31.
- Kalamachi A, Dawe RV (1985) Congenital deficiency of the tibia. J Bone Joint Sur 67: 581-584.
- Weber M (2008) New classification and score for tibial hemimelia. J Child Orthop 2: 169-175.
- Paley D (2016) Tibial hemimelia : A new classification and reconstructive options. J Child Orthop 10: 529-555.
- Paley D (2002) Principle of deformity correction. Springer, Berlin, Germany.
Citation: Sahoo PK, Sahoo MM (2018) Unclassified Tibial Hemimelia-A Case Report. Clin Res Foot Ankle 6:266. DOI: 10.4172/2329-910X.1000266
Copyright: © 2018 Sahoo PK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5978
- [From(publication date): 0-2018 - Nov 21, 2025]
- Breakdown by view type
- HTML page views: 5033
- PDF downloads: 945