Research Article Open Access
Venous Thromboembolism Prophylaxis in Patients Immobilised in Plaster Casts
Cezary Kocialkowski, Abhijit Bhosale and Anand Pillai*Department of Trauma and Orthopaedics, University Hospital of South Manchester, United Kingdom
- *Corresponding Author:
- Anand Pillai
Consultant Orthopaedic Surgeon, Clinical Research Fellow
Department of Trauma and Orthopaedics, University Hospital of South Manchester
South Moor Road, Wythenshawe, M23 9LT United Kingdom
Tel: 01619987070
E-mail: anand.pillai@uhsm.nhs.uk
Received date: Jan 12, 2016; Accepted date: Sep 03, 2016; Published date: Sep 19, 2016
Citation: Kocialkowski C, Bhosale A, Pillai A (2016) Venous Thromboembolism Prophylaxis in Patients Immobilised in Plaster Casts. Clin Res Foot Ankle 4:203. doi:10.4172/2329-910X.1000203
Copyright: © 2016 Kocialkowski C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Clinical Research on Foot & Ankle
Abstract
Introduction: Lower limb immobilisation in plaster is associated with a risk of venous thromboembolism. It has been demonstrated that prophylaxis with low molecular weight heparin can reduce this risk. Recent guidelines have therefore recommended thromboprophylaxis for all patients immobilised in plaster and with one further risk factor.
Method: In order to standardise the thromboprophylaxis process, our trust recently developed a risk assessment tool, for all patients with a lower limb fracture immobilised in plaster. Patients are scored on a variety of risk factors and if judged to be sufficiently high risk, are prescribed low molecular weight heparin.
Results: Regular audit of the process has shown that good compliance can be achieved. In addition root cause analysis has only demonstrated three cases of venous thromboembolism, since the introduction of the tool, which suggests that the assessment can accurately differentiate high risk patients.
Conclusion: A risk assessment tool for lower limb immobilisation can be used successfully to target high risk individuals with thromboprophylaxis. This process ensures that all patients are correctly risk assessed and that low risk patients are not over exposed to the risks of low molecular weight heparin therapy.
Keywords
Venous thromboembolism; Lower limb immobilization; Ankle fracture; Plaster cast; Low molecular weight heparin
Introduction
The overall incidence of lower limb injuries is increasing, possibly due to greater participation in sporting activities [1]. Many fractures and significant soft tissue injuries, including Achilles tendon ruptures, are treated with immobilisation in plaster cast [2]. Lower limb immobilisation is a recognised risk factor for venous thromboembolism (VTE) [3], with the incidence of deep vein thrombosis (DVT) after lower limb immobilisation ranging between 1.1% and 20% [4]. Although the majority of DVTs are asymptomatic distal thrombi, there is a small risk of clot propagation, potentially leading to fatal pulmonary embolism (PE) [5]. Other complications of DVT include development of post-thrombotic syndrome and venous ulcers [6].
Low molecular weight heparin (LMWH) has been established as a successful method of preventing VTE for many surgical procedures; especially hip and knee arthroplasty and has been demonstrated to reduce proximal and distal DVT by 70% [7]. Despite these benefits, there has been no clear consensus on the role of LMWH in the prevention of VTE in patients with immobilisation of lower limbs [8]. Multiple studies have however, demonstrated a significant reduction in VTE with the use of LMWH, in patients with lower limb immobilisation [3,9-11]. A Cochrane review also demonstrated a reduction in symptomatic VTE from 2.5% to 0.3% and an overall halving of the incidence of VTE [12]. In view of this increasing evidence, recent guidelines from the College of Emergency Medicine in the United Kingdom, have recommended VTE prophylaxis using LMWH for all patients immobilised in lower limb plaster cast who have one further risk factor for VTE [13].
Routine use of LMWH as out-patient prophylaxis does however, expose patients to the small but significant risk of side effects, such as major bleeding episodes and heparin induced thrombocytopenia (HIT) [3,14]. Many low risk patients may therefore be unnecessarily be exposed to the potential side effects of treatment. Identifying a high risk sub-group on whom to target thromboprophylaxis has however, proved challenging [12]. To assess this problem, our trust recently developed a risk assessment tool for all patients immobilised in lower limb plaster cast, in either the orthopaedic fracture clinic or emergency department (ED), based on our experiences with in-patient VTE prophylaxis.
Method
In May 2013, our trust introduced a new VTE risk assessment proforma for all patients immobilised in lower limb plaster cast in either the orthopaedic fracture clinic or ED. This risk assessment proforma was developed by the local VTE committee, with regard to the available evidence of VTE in lower limb immobilisation and also from the experience of in-patient VTE risk assessment, which has been well established in our trust for many years.
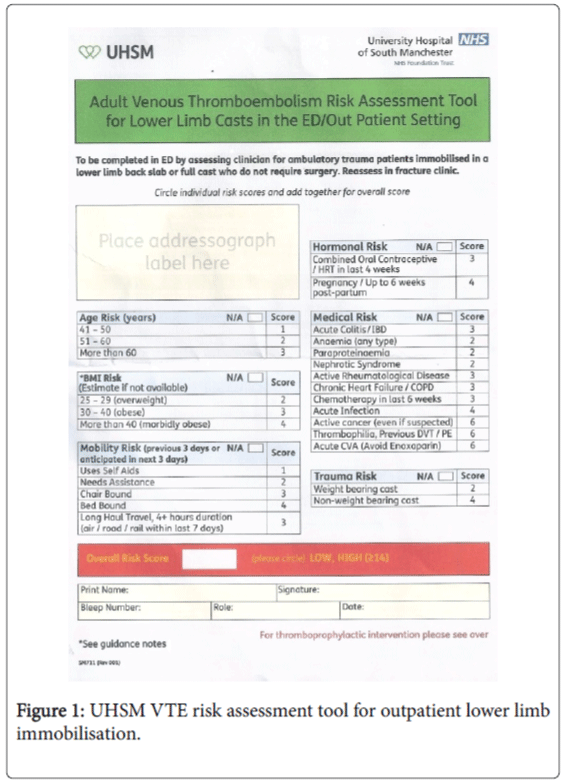
The VTE committee recognised that although there was a need to provide VTE prophylaxis for patients with lower limb immobilisation, there was a risk of over treating low risk patients and unnecessarily exposing them to the risks of LMWH therapy. As a result the committee attempted to identify a high risk subset of patients, who would stand most to benefit from VTE prophylaxis. A series of risk factors were identified, similar to the pre-existing risk assessment of hospital in-patients. These risk factors included age, body mass index, mobility risk, hormone risk, medical risk and trauma risk (Figure 1).
Patients would be scored on each risk factor by an admitting clinician with a threshold target set of 14 points, to qualify for automatic LMWH prophylaxis. This threshold was set as such, because it was felt to identify patients who had several risk factors and would be ‘high risk’ for VTE. Patients who scored below 14 points would be considered ‘low risk’ and would simply be advised hydration and mobilisation. It was nevertheless possible for clinicians to use their clinical judgment and LMWH could still be prescribed to low risk individuals, if the admitting clinician felt this was appropriate. The most important aspect of the process was that all patients would be risk assessed and therefore the clinicians could discuss with patients the potential risks of VTE as well as the risks and benefits of LMWH prophylaxis.
Thromboprophylaxis was prescribed as Enoxparin 40 mg (Sanofi, Paris, France) once daily subcutaneous injection, which is our inpatient LMWH of choice for thromboprophylaxis. The tool was developed with close cooperation of the hospital pharmacy department, who would provide the Enoxaparin as an outpatient prescription for all high risk patients. Due to the low risk of HIT, it was not felt that regular blood test monitoring was necessary but all patients who were commenced on thromboprophylaxis had baseline blood tests performed and reviewed, including a full blood count, urea and electrolytes and clotting studies.
After the risk assessment proforma was rolled out across the trust, the process was audited after six months to assess compliance with the process. Any VTE diagnoses in patients with lower limb immobilisation were highlighted to a coordinator, who performed root cause analysis to assess whether the risk assessment tool was functioning correctly. The VTE committee met at regular intervals to discuss the results of audit and root cause analysis, to decide whether any further amendments of the proforma were required.
Results
Initial audit of the risk assessment proforma demonstrated that compliance with the process was good, with overall 80% of patients risk assessed. The majority of these risk assessments were performed by specialist nurse practioners, who had been trained in the use of the risk assessment tool in the ED. Medical clinicians however, only performed risk assessments in 50% of cases when assessing patients in the ED or the fracture clinic.
In order therefore, to try and further improve compliance, particularly amongst medical personnel, a new policy was introduced, whereby no lower limb plaster casts would be applied by plaster technicians in the fracture clinic, if a valid risk assessment had not been performed.
There was also regular training provided to all ED and fracture clinic staff, to highlight the importance of risk assessments. Subsequent re-audit of the process demonstrated a significant improvement in compliance, with 100% of patients risk assessed in the ED and fracture clinic.
Overall 10% of patients were assessed as high risk in the audit. All of these patients received thromboprophylaxis for the period of immobilisation. In addition another 10% of patients did not meet the scoring criteria to be considered high risk, but were nevertheless prescribed thromboprophylaxis, based on the clinical judgement of the treating physician, usually a decision made in the fracture clinic by an orthopaedic surgeon.
Root cause analysis has so far highlighted three cases of patients developing VTE while immobilised in lower limb plaster. One was an elderly patient with an ankle fracture, who was assessed as high risk but was not prescribed LMWH for the entire period of immobilisation and subsequently developed a DVT.
Another was an elderly patient with an ankle fracture, considered as low risk but who had a recent long haul flight, which was not included in the risk assessment and subsequently developed a DVT.
The final case was younger patient with a navicular fracture, who was morbidly obese and had a family history of VTE, who was also considered low risk but who developed a PE.
These cases have helped to highlight the importance of correctly risk assessing all patients and ensuring that LMWH is prescribed for the full duration of immobilisation. With regard to the final case in particular, the VTE committee have decided to partially amend the risk assessment tool, in respect to the weighting of obesity as risk factor.
In future any patient who is morbidly obese (body mass index > 40) will trigger an immediate high risk score. Family history of VTE, was also not originally included in the proforma, as it was felt to be difficult to corroborate but has since been included in the amended proforma.
Discussion
It has been recognised for over half a century that patients with immobilisation of the lower limbs are at increased risk of VTE [15]. Several studies have been performed over the last couple of decades, examining the use of LMWH to reduce the risk of VTE in these patients. One of the earliest trials was by Kujath et al. [9], who randomised patients with lower limb immobilisation in plaster, to either daily LMWH or no thromboprophylaxis. The control group had a VTE incidence of 16.5%, whilst the treatment group had a significantly lower incidence of 4.8%.
Another trial by Kock et al. [3] randomised patients with any type of lower limb injury, immobilised in plaster, to either daily LMWH or no prophylaxis. The DVT rate in the control group was significantly higher, 4.3% compared to zero in the treatment group. Patients above the age of 40 and patients with an above knee plaster were particularly at risk. Lassen et al. [10] performed a study where patients with lower limb immobilisation were randomised to either daily LMWH or placebo injections. There was a significant reduction in the rate of DVT in the treatment group with an odds ratio of 0.45 and with reductions seen in both patients with fractures and Achilles tendon ruptures.
In contrast to this however, Lapidus et al. [16,17] performed two separate studies examining the use of LMWH to prevent VTE in patients with lower limb immobilisation following ankle fracture or Achilles tendon rupture, randomising to either LMWH or placebo injections. There was no significant reduction found in either group with the use of LMWH. Another study by Jorgensen et al. [4] also found no significant reduction in VTE in lower limb immobilisation with the use of LMWH but the prophylactic dose was smaller than in most other studies and may have contributed to the lack of treatment effect.
Teestroote et al. [12] performed a Cochrane review assessing the use of LMWH to prevent VTE in lower limb immobilisation. Overall they found a significant reduction in the incidence of VTE with the use of LMWH with an odds ratio of 0.49. Significant reductions were found in patients with conservatively and surgically managed fractures and also in patients with soft tissue injuries. Based on these results the authors recommended routine prophylaxis for all patients immobilised in a plaster cast or a brace.
One of the controversies regarding the use of LMWH to prevent VTE is that the majority of thromboses are asymptomatic distal DVTs [16]. The significance of these distal thrombi has been debated, as it is recognised that many of these DVTs will undergo spontaneous thrombolysis and may therefore not require treatment [17]. Other studies have however suggested that proximal extension of distal DVTs can be as high as 28%, which can in turn result in potentially fatal PE [5]. In addition there is a risk of patients developing post-thrombotic syndrome and venous leg ulcers [8].
Another controversy has been whether a high risk subset of patients can be identified in whom to target prophylactic therapy. Some studies have suggested that older patients, immobilisation in a plaster and fractures or Achilles tendon ruptures are associated with increased risk of VTE [4,18]. Other research however, has not demonstrated any difference in rate of VTE in different subgroups, with even patients considered as low risk, having significant rates of DVT following lower limb immobilisation. This has led to some authors recommending that all patients with lower limb immobilisation receive thromboprophylaxis, especially as the incidence of side effects from LMWH has generally been very low [12,19].
Not all studies however, have found such high rates of VTE after lower limb immobilisation. Patel et al. [14] performed a retrospective review of patients with Achilles tendon ruptures and found that the rate of symptomatic DVT was only 0.43% and PE was 0.34%. The authors felt that this low incidence of VTE did not merit blanket thromboprophylaxis of all patients with lower limb immobilisation. In the United Kingdom guidelines from the College of Emergency Medicine recommend that all patients who are immobilised in plaster cast and have one other risk factor for VTE, should receive prophylactic LMWH. Our local protocol is slightly more stringent and patients must score sufficiently highly on a number of risk factors to automatically be prescribed thromboprophylaxis.
Limitations to our study include the fact that our root cause analysis only detects symptomatic DVTs and PEs. It has been widely recognised that the majority of thrombotic events in immobilised patients are asymptomatic distal DVTs, which are likely to be missed in our cohort. In addition it is difficult to assess patient compliance with the process and LMWH injections, although the majority of patients assessed in fracture clinic have been satisfied with the process and the majority have self-administered the injections.
We believe that out risk assessment tool provides a robust and objective method of assessing all patients immobilised in lower limb plaster cast and enables clinicians and patients to reach a balanced decision regarding thromboprophylaxis. It allows us to target higher risk patients and prevent over treating low risk individuals.
Conclusions
The development of a risk assessment proforma for all patients immobilised in lower limb plaster cast, in our hospital trust, has demonstrated that patients can be safely risk assessed as either high or low risk for VTE and that thromboprophylaxis can be safely reserved for those patients judged to be at increased risk. Good compliance with the process is achievable in the ED and fracture clinic. Regular review of the risk assessment proforma and root cause analysis of all VTE events is however required to ensure that the process remains robust and amendments are made to the assessment as required.
Acknowledgements
We would like to thank Sr. Christine Bailey, venous thromboembolism specialist nurse, and Ms. Anna Poole, senior pharmacist, as well as all other members of the VTE Committee, for their help in developing the risk assessment tool.
Conflicts of Interest
The authors confirm no conflict of interests.
Funding
The authors confirm that they, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article. No outside grants or funding were received for this study.
References
- Leppilahti J, Orava S (1998) Total Achilles tendon rupture: a review. Sports Med 25:79-100.
- Jensen SL, Andresen BK, Mencke S, Nielsen PT (1998) Epidemiology of ankle fractures. A prospective population-based study of 212 cases in Aalborg, Denmark. ActaOrthopScand 69:48-50.
- Kock H-J, Schmidt-Neuerburg KP, Hanke J, GRudofsky(1995) Thromboprophylaxis with low-molecular weight-heparin in outpatients with plaster cast immobilisation of the leg. Lancet 346:459-461.
- Jorgensen PS, Warming T, Hansen K, Paltved C, Vibeke Berg H, et al. (2002) Low molecular weight heparin as thromboprophylaxis in outpatients with a plaster cast: a venographic controlled study. Thromb Res 105:477-480.
- Lohr JM, James KV, Deshmukh RM, Kimberly AH (1995). Calf vein thrombi are not a benign finding. Am J Surg 170:86–90.
- International Consensus Statement (1997) Prevention of venous thromboembolism. Med-Orion Publishing, London.
- Hirsh J, Dalen J, Guyatt G (2001) The sixth ACCP guidelines for antithrombotic therapy for prevention and treatment of thrombosis: American College of Chest Physicians. Chest 119:1S-2S.
- Batra S, Kurup H, Gul A, Andrew JG (2006) Thromboprophylaxis following cast immobilisation for lower limb injuries–survey of current practice in United Kingdom. Injury 37:813-817.
- Kujath P, Spannagel U, Habscheid W (1993) Incidence and prophylaxis of deep venous thrombosis in outpatients with injury of thelower limb. Haemostasis23:20–26.
- Lassen MR, Borris LC, Nakov RL (2002) Use of the low-molecular- weight heparin reviparin to prevent deep-vein thrombosis after leg injury requiring immobilization. N Engl J Med 347: 726-730.
- Ettema HB, Kollen BJ, Verheyen CC, Büller HR (2008) Prevention of venous thromboembolism in patients with immobilization of the lower limb extremities: a meta-analysis of randomized controlled trials. J ThrombHaemost 6:1093-1098.
- Testroote M, Stigter W, de Visser DC, Janzing H (2008) Low molecular weight heparin for prevention of venous thromboembolism in patients with lower-leg immobilization. Cochrane Database Syst Rev 4:CD006681.
- (2012)GEMNet guideline.Thromboprophylaxis in ambulatory trauma patients requiring temporary limb immobilization. College of Emergency Medicine.
- Patel A, Ogawa B, Charlton T, Thordarson D (2012) Incidence of deep vein thrombosis and pulmonary embolism after achilles tendon rupture. ClinOrthopRelat Res 470:270–274.
- Bauer G (1944) Thrombosis following leg injuries. ActaChirScand 90:229-249.
- Lapidus LJ, Ponzer S, Elvin A, Levander C, Larfars G, et al. (2007) Prolonged thromboprophylaxis with Dalteparin during immobilization after ankle fracture surgery. ActaOrthop 78:528–535.
- Lapidus LJ, Rosfors S, Ponzer S, Levander C, Elvin A, et al. (2007) Prolonged thromboprophylaxis with dalteparin after surgical treatment of achilles tendon rupture: a randomized, placebo-controlled study. J Orthop Trauma 21:52–57.
- Riou B, Rothmann C, Lecoules N, Bouvat E, Bosson JL, et al. (2007) Incidence and risk factors for venous thromboembolism in patients with nonsurgical isolated lower limb injuries. Am J Emerg Med 25:502–508.
- Healy B, Beasley R, Weatherall M (2010) Venous thromboembolism following prolonged cast immobilisation for injury to the tendo Achilles. J Bone Joint Surg Br 92:646–650.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 12840
- [From(publication date):
September-2016 - Aug 19, 2025] - Breakdown by view type
- HTML page views : 11839
- PDF downloads : 1001