Vogt Koyanagi Harada Syndrome Presented with Aseptic Meningitis: Diagnosis not to be Missed: A Case Report
Received: 14-Mar-2022 / Manuscript No. JNID-22-57029 / Editor assigned: 16-Mar-2022 / PreQC No. JNID-22-57029(PQ) / Reviewed: 30-Mar-2022 / QC No. JNID-22-57029 / Revised: 04-Apr-2022 / Manuscript No. JNID-22-57029(R) / Published Date: 11-Apr-2022 DOI: 10.4172/2314-7326.1000385
Abstract
VKH syndrome or uveomeningitic syndrome is a systemic disorder involving many organ systems, including the eye, skin, ear, integumentary and nervous system. An autoimmune process in a genetically susceptible individual who contacts a viral infection is the most likely mechanism.Here we reported Asian 43 female patient, presented with symptoms of aseptic meningitis, bilateral uveitis, bilateral hearing loss and vitiligo. She was initially suspected bacterial CNS infections and was managed with empiricala antibiotics then after revised clinical criteria and ruling out of underlying infectious causes, diagnosis of VKH syndrome was done and was started pulse intravenous steroids with marked improvement of hearing and tinnitus.
Keywords: Vogt Koyanagi Harada; Aseptic meningitis; Bilateral hearing loss; Exudative retinal detachment; Vitiligo
Keywords
Vogt Koyanagi Harada; Aseptic meningitis; Bilateral hearing loss; Exudative retinal detachment; Vitiligo
Introduction
VKH syndrome or uveomeningitic syndrome is a granulomatous multisystemic disorder involving many organ systems, including the eye, ear, integumentary and nervous system [1]. The disease has a predilection for more darkly pigmented races such as Asians, Hispanic, and American Indians [2]. Most patients are in the second to fifth decade of life at the onset of the disease [2]. The exact etiology of VKH is still unknown. An autoimmune process in a genetically susceptible individual who contacts a viral infection is the most likely mechanism. The autoimmune aspect in VKH includes a cellular immune response against melanocytes [3]. The American Uveitis Society diagnostic criteria for VKH syndrome included no history of ocular trauma (including surgery) and at least one finding in three, out of the following four categories:
1) Bilateral chronic iridocyclitis
2) Posterior uveitis, including exudative retinal detachment, disk hyperemia or edema and sunset glow fundus
3) Neurologic signs: tinnitus, meningismus
4) Cutaneous findings of alopecia, poliosis [4]
The treatment of VKH usually begins with early and aggressive use of systemic steroids followed by slow tapering over three months. Cytotoxic and immunosuppressive agents are reserved for the cases which are refractory to steroids [4, 5]. So we aimed from case report to increase awareness about this rare disease and its uncommon presentation as a cause of aseptic meningitis in order not to be missed.
Informed Consent
Written informed consent was obtained from the case. A copy of the written consent is available for review by the Editor of this journal.
Case Presentation
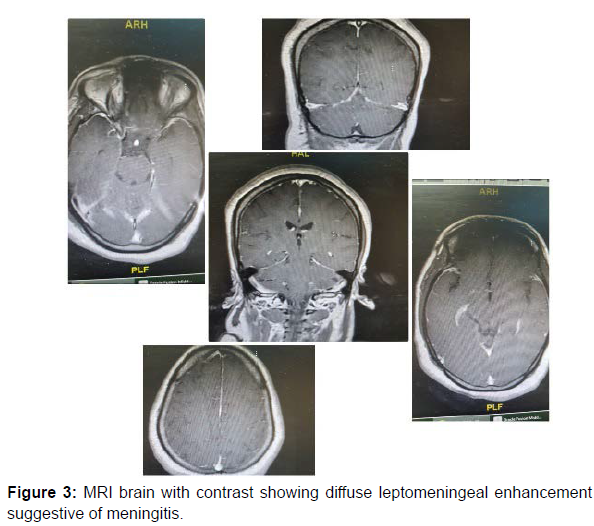
43 years old Asian female patient previously healthy was presented at February 2022 to our hospital with subacute onset stationary course of low grade fever, headache, mild cloudiness in conscious level, bilateral severe local ocular inflammation (Figure 1) with bilateral diminution of vision, bilateral tinnitus and diminution of hearing with no history of trauma, treatment or surgery in either eye.By examination she was vitally stable and her general examination showed discolored patchy skin areas distributed on both upper limbs and trunk mostly vitilgo (Figure 2). She was slightly agitated, with bilateral rupture globe, uveitis, scleritis and exudative retinal detachment mainly on left side with no light perception on left side and only hand motion on right side, bilateral sensory neural hearing loss, no other cranial nerve affection. There were no signs suggestive of motor or sensory or coordination affection. No meningeal irritation signs. Central nervous system infection was suspected and urgent MRI brain with contrast was done with picture of diffuse meningeal enhancement (Figure 3). Lumbar puncture was done showed total cell count of 50 cells /mm3 mainly PMNLs and high proteins of 900 mg /dl with slightly consumed CSF glucose 2 mmol/l (lower limit was 2.5 mmol/l). According to these results bacterial CNS infection including tuberculosis was suspected and was covered with empirical antibiotics and antituburculous medications till result of culture and sensitivity which was negative later on. Also TB PCR and T spot test of tuberculosis were negative and there was no improvement in general condition. After ruling out underlying CNS infection other causes of aseptic meningitis were investigated including autoimmune causes and all were negative. After revising history and clinical criteria of the patient presentation, the diagnostic entity considered most likely was Vogt-Koyanagi-Harada syndrome (VKH). And the patient was started intravenous pulse methylprednisolone 1gm for 5 days then was shifted on oral steroids with a dose of 1 mg / kg, and showed marked improvement in hearing and reduced tinnitus but unfortunately no improvement in visual acuity. Then she was referred to ophthalmology department for follow up long term management plan.
Discussion
VKH is a disease that has been well studied, with precise diagnostic criteria. Despite having a regular and consistent clinical presentation pattern, it is little known. The clinical diagnosis of VKH can offer difficulties for several reasons. First, the disease has 4 chronological phases and at the time of the initial consultation the patients may be in any phase of the disease and the demonstration of choroidomeningeal inflammation and its characterization in the corresponding phase becomes a real challenge. Second, when the acute uveitic phase occurs, the patients alarmed by the visual alterations consult for the first time, usually ophthalmology [6]. However, it is important to keep in mind that this phase of acute ocular alterations. This presentation of the disease constitutes a diagnostic challenge for the medical group. Its clinical approach should include the study of the ophthalmological alteration and the neurological and otovestibular involvement, simultaneously. It was in these conditions of clinical concomitance between the prodromal phase and the acute uveitic phase when the patient of this case consulted. Therefore, in cases like this, it is considered important to recognize the various presentations of VKH emphasizing the clinical and paraclinical characteristics of the 2 initial phases in order to diagnose the disease early [7]. Regarding the diagnostic criteria, ophthalmologists of endemic areas of VKH and experts in uveitis of specialized reference centers question the need to practice LP as a diagnostic procedure, considering that the diagnosis of the disease is fundamentally clinical and, in doubtful cases, the AGF and OCT images of the macula and optic nerve help to confirm the clinical impression and, therefore, it is not advisable to expose patients to the side effects of LP [8]. Against this opinion, the authors of the present work consider that, on the one hand, the diagnosis of choroiditis during the acute uveitic phase of VKH disease is not as evident in a first ophthalmological examination and, on the other hand, although the classic acute choroiditis of VKH, with or without retinal detachments, is observed in the ophthalmological examination, if the patient has headache and signs of meningeal irritation the neurological approach is necessary and the LP is mandatory [9]. In fact, the uveomeningoencephalic syndrome poses a very broad etiological spectrum that includes several infectious, neoplastic, paraneoplastic and autoimmune diseases. Consequently, the study of the CSF is key to give precision and diagnostic certainty. If lymphocytic pleocytosis in CSF is demonstrated, in consonance with aseptic meningitis, a criterion that allows to initiate immunosuppressive treatment is met. Even, a new LP should be performed to a patient with established diagnosis of VKH, immunosuppressed with treatment, who in the course of the evolution presents headache and meningism, in order to rule out an opportunistic neuroinfection or recurrent aseptic meningitis. In a riskbenefit balance, the benefit obtained from LP is much greater compared to its possible complications; the fear of side effects derived from an LP does not appear to be a valid reason to hinder its realization [10].
Conclusion
We report a Asian female case with criteria suggestive of vogt koyanagi harada syndrome was presented at neurology department as a case of aseptic meningitis and after ruling out underlying causes of CNS infection, diagnosis was maid and was started the proper management, so we aimed to increase awareness for this syndrome and its different rare presentations in order not to be missed because early management and intervention results in good prognosis especially for visual functions.
Conflict of interest: On behalf of all authors, the corresponding author states that there is no conflict of interest.
Funding sources: No fund was needed for this study
Author contribution: Dr Diana khedr responsible for data collection, analysis, interpretation of results and drafted the article. Dr Sulaiman elkhashan revised, approved the version to be published and was directly approving management plan Dr hany was the primary following admitting doctor of the case and helped in result interpretation and data collection .Dr shaimaa and Dr dina, were following response to management plan and helped in data collection and analysis.
References
- Jogn HJ, Paul GA (2010) Ocular Inflammatory Disease and Uveitis Manuel: Diagnosis and Treatment, 1st Ed. Lippincott Williams & Wilkins.
- Read RW, Holland GN, Rao NA, Tabbara KF, Ohno S, et al. (2001) Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: report of an international committee on nomenclature. Am J Ophthalmol 131(5): 647-652.
- Attia S, Khochtali S, Kahloun R, Zaouali S, Khairallah M (2012) Vogt – Koyanagi – Harada disease. Expert Rev. Ophthalmol 7(6): 565-585.
- Moorthy RS, Inomata H, Rao NA (1995) Major Review - Vogt-Koyanagi-Harada Syndrome. Surv Ophthalmol 39(4): 265-292.
- Snyder DA, Tessler HA (1980) Vogt-Koyanagi-Harada syndrome. Am J Ophthalmol 90: 69-75.
- Agarwal A (2008) Fundus Fluorescein and Indocyanine Green Angiography: A textbook and Atlas. Slack Inc.
- Chee SP, Jap A, Cheung CMG (2010) The Prognostic Value of Angiography in Vogt-Koyanagi-Harada Disease. Am J Ophthalmol 150(6): 888- 893.
- Nguyen M, Duker J (2015) Ophthalmic Pearls: Retina- Identify and Treat Vogt-Koyanagi-Harada Syndrome. American Academy of Ophthalmology, 2005.
- Morita S, Nakamaru Y, Obara N, Masuya M, Fukuda S (2014) Characteristics and prognosis of hearing loss associated with Vogt-Koyanagi-Harada disease. Audiol Neurootol 19(1): 49-56.
- Noguchi Y, Nishio A, Takase H, Miyanaga M, Takahashi H, et al. Audiovestibular findings in patients with Vogt-Koyanagi-Harada disease. Acta Otolaryngol 134(4): 339-344.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Khedr S, Soliman SH, Helal H, Mansour DF, Alkhashan S (2022) Vogt Koyanagi Harada Syndrome Presented with Aseptic Meningitis: Diagnosis not to be Missed: A Case Report. J Neuroinfect Dis 13: 385. DOI: 10.4172/2314-7326.1000385
Copyright: © 2022 Khedr S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3075
- [From(publication date): 0-2022 - Dec 04, 2025]
- Breakdown by view type
- HTML page views: 2426
- PDF downloads: 649