Voluntary HIV Counselling and Testing (VCT): Knowledge, Attitudes, Hindrances, and Practices of Adults Seeking Treatment at Gulu Regional Referral Hospital on the Spread of HIV in Northern Uganda: A Cross-Sectional Study
Received: 10-Dec-2021 / Editor assigned: 01-Jan-1970 / Reviewed: 01-Jan-1970 / Revised: 01-Jan-1970 / Accepted Date: 03-Jan-2022 / Published Date: 10-Jan-2022
Abstract
Background: In 2011, Uganda had a national HIV prevalence of 6.7%. Between 2008 and 2009, there was an upsurge in HIV in Gulu District from 9.4% to 16.0% with Gulu Municipality at 22.1%. Similarly, in 2020, the prevalence of HIV in Gulu District persistently remained high at 14.0%, much higher than the national average at 6.0%. The objective of this study was to assess knowledge, attitudes, hindrances, and practices on voluntary HIV counselling and testing (VCT) and determine factors associated with VCT practices among adults seeking treatment at the outpatient department of Gulu Regional Referral Hospital.
Methods: A cross-sectional study was conducted with 384 participants. Simple random sampling was used to recruit participants. Knowledge and practices on VCT were determined using knowledge ratings and attitudes using a modified Likert scale. A questionnaire with an internal validity of Cronbach’s α=0.71 was used. Ethical approval was obtained, and SPSS was used for data analysis at univariate, bivariate and multivariable logistic regression. A p-value less than 0.05 were considered significant.
Results: The most significant findings were that knowledge and attitude significantly affect VCT practices among adults in Gulu Hospital. Most participants had adequate knowledge (297/379, 78.4%), the most common source of VCT information was radio (236/372, 63.4%) and few from parents (30/372, 8.1%). 158/380(41.6%) had strongly positive attitudes however, 4/10(40.0%) believed knowing HIV status was not beneficial because of fear of stigma, 299/380(78.7%) had good practices,13/45(28.9%) did not undertake VCT due to ignorant on the importance, 9/45(20.0%) feared positive results, and 5/45(11.0%) for far-off service centers. Among those who discouraged others, 15/45 (83.0%) did it for no reason, while 2/45 (11.0%) believed it was a risky and painful process. Knowledge and attitude on VCT practices had an adjusted R square of 0.421, p<0.001. The independent predictors of VCT practices in a multivariable regression analysis was knowledge (β=0.478, t=10.374, p<0.001) and attitudes (β=0.257, t=5.570, p<0.001).
Conclusion: Knowledge and attitudes significantly influenced VCT practices among adults attending outpatient services at Gulu Hospital. The independent determinants of VCT practices were knowledge and attitudes. However, HIV stigma, fear of positive results and divorce/separation were the most deterring factors on VCT practices among participants.
Keywords: VCT; HIV; Knowledge; Attitudes; Practices; Hinderances; Gulu Regional Referral Hospital; Stigma
Introduction
The role voluntary counselling and testing (VCT) plays in HIV and AIDS prevention and control is multifaceted [1]. Many studies indicate that VCT can be considered an entry point to prevention and care for ongoing emotional and spiritual care and social support for persons affected with HIV and AIDS [1]. However, to achieve better results from VCT in African communities, there is a need to consider adults’ opinions, as they are mainly guardians and mentors to the young generation, especially the youth [2]. Adults in African communities play a large role in moderating the pattern, control, and prevention of sexual transmission of HIV in many communities [2]. In addition, the transmission of HIV and AIDS in these communities is determined mainly by social, legal, and economic relations between genders [2].
Of important historical analysis was that during the 1980s, there were few HIV testing services in Uganda, particularly outside researchrelated programs, and none was linked to counselling programs [3,4]. At the time, there was an enormous burden placed on Uganda Blood Transfusion Services (UBTS), as many Ugandans donated blood to determine their HIV status [3,4]. In response to the growing demand for HIV testing, several organizations convened a meeting to discuss the need for anonymous VCT services [3,4]. As a result, Uganda established Africa’s first confidential VCT services, thereby launching the AIDS Information Center (AIC) in Kampala, Uganda, in 1990 [3,4].
This action reportedly became one of the major success stories Uganda undertook in scaling down the HIV prevalence from a double digit to a single digit over a period of two decades [5-7]. Interestingly, this success story was maintained for a couple of years, but it is facing many challenges leading to a suspected upsurge in HIV prevalence across the country and in particular Northern Uganda [8].
According to research conducted and published in 2009 in Northern Uganda by Health Alert, a non-governmental organization, 82% of females and more than 50% of males in Gulu District were not knowledgeable about VCT. This finding suggested that a lack of VCT knowledge, poor attitudes and practices could contribute to the increase in HIV prevalence from 9.4% in 2008 to 16.0% in 2009 in Gulu District [8], with Gulu Municipality health subdistrict leading at 22.1%.
Similarly, a recent study conducted by the Uganda AIDS Commission (UAC) in 2020 found that the prevalence of HIV and AIDS in Gulu District was 14.0%, which was much higher than the national average of 6.0% and Northern Uganda’s average of 7.0% [9]. Recent UAC data showed that the HIV prevalence in Gulu District was much higher in females (17.1%) than in males (8.0%). The high prevalence was attributed to many factors, especially male residents having multiple sexual partners, low uptake of safe male circumcision, and poverty, among many other reasons [9].
Additionally, a study conducted in Gulu District in 2011 found that 36.1% of respondents had undertaken VCT, while the majority (63.9%) had not [5]; 77.9% had two or more sexual partners, and most of them said they used condoms, so there was no need for testing because they felt they were protected against any sexually transmitted diseases [5,10].
Interestingly, many studies conducted among African parents observed that most of them were uncomfortable talking with their children about sexuality, although previous information showed that many lacked accurate sexual health knowledge and information [11]. In Africa, it was experiential that cultural barriers, age, and gender differences contributed to inadequate or complete reluctance of parents to discuss sexual matters with their families and children [12,13]. These factors are believed to have negatively impacted sexual and reproductive development among children [10].
This study was designed to assess knowledge, attitudes, hindrances, and VCT practices and determine the factors associated with VCT practices among adults attending outpatient department (OPD) services at Gulu Regional Referral Hospital.
Methodology
Study design
This was a cross-sectional study conducted among adults attending outpatient clinics at Gulu Regional Referral Hospital in Northern Uganda in 2012.
Study site
This study was conducted at Gulu Regional Referral Hospital (GRRH), a regional public hospital located in the Laroo Division of Gulu Municipality, Gulu District, Northern Uganda. It is a regional referral health facility for the central North of Uganda and treats patients from the surrounding districts, South Sudan, and the Democratic Republic of Congo (DRC). The hospital has a bed capacity of 397, with an average bed occupancy of 220 patients per day and an average bed occupancy rate of 61.3% (unpublished GRRH report of 2010/2011). The general outpatient department (OPD) attendance in the financial year 2010/2011 was 77,128 patients, many of whom were adults (63,212), and most of them did not know their HIV status, yet VCT services were available in the hospital at no fee. GRRH also provides specialized services in ophthalmology, Ear Nose and Throat, orthopedics, mental health, physiotherapy, diabetes, hypertension, sickle cell disease, dermatology, accident and emergency, cardiology, surgery, internal medicine, maternal and child health, dental, pediatrics, HIV, and adolescent health services, among others.
Study population
These were adults seeking treatment at outpatient department clinics, i.e., general OPDs and specialized clinics of GRRH.
Selection criteria
Inclusion criteria:
• Adult seeking care at the outpatient department of GRRH.
• Informed consent.
The exclusion criteria were as follows:
• Adults with hearing and speech difficulties.
• Adults who were acutely ill and could not be interviewed.
Sampling method
The research team adopted a simple random sampling method for recruiting participants to this study. A simple random sampling technique was used because it was found important that each sample had an equal probability of being chosen, and thus, an unbiased representation of the sampled population was obtained. An unbiased random sample was important for drawing rational conclusions.
Sample size estimation
The minimum sample size was calculated using the Kish-Leslie (1965) formula 
where, n=sample population
Z=confidence level
p=prevalence value
q=1-p, and
d=precision value
With a 95% confidence level (1.96), an estimated prevalence of VCT utilization in the community of approximately 50% (0.5), and a precision value of 0.05, we calculated the sample size of this study population. We used 50% to estimate the sample size because the VCT prevalence in this study population was not yet known.
The calculated sample size of the study population was
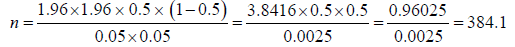
Thus, the minimal sample size obtained for this study population was 384.
Sampling technique
A total sample of 384 participants was randomly and consecutively selected from OPD clinics of Gulu Regional Referral Hospital.
Data collection
Study instrument: We collected data for this study using a questionnaire (Supplementary File A1). The questionnaire was designed by the research team and had structured questions (SQs) and unstructured questions (UQs). Questions on socio-demographic and personal characteristics of participants were age, sex, address, occupation, tribe, religion, marital status, number of children, and highest level of education attained); on knowledge (basic information on what VCT was, where it was conducted, how it was conducted, when it was conducted, and usefulness) were explored, attitudes (whether knowing one’s HIV status was necessary, beneficial, or whether one was afraid of being tested, aware of VCT services, and whether sensitization of people on VCT was important), hinderances (If one had not tested for HIV, and the explanation? If one discouraged the other from undertaking VCT, and the explanation? If knowing one’s HIV status was not important, the explanation? If one discouraged the other from undertaking VCT, the explanation was required), VCT practices (Whether one had tested for HIV? If no, the explanation? whether one had undertaken VCT with a partner? If no, the explanation? If one had encouraged the other from undertaking VCT? If no, the explanation? If one had discouraged others from undertaking VCT? if yes, the explanation? And finally, participants were asked when the best time for undertaking VCT was?). These UQs provided the opportunity for participants to express their thoughts and views on VCT services.
Pretest of the questionnaire: The questionnaire was designed by the research team to collect sociodemographic data and information on knowledge, attitudes, hindrances, and practices on voluntary HIV counselling and testing. It was pretested among adult patients attending OPD services at St. Mary’s Hospital, Lacor, a hospital that is six kilometers from GRRH but within the Bardege division of Gulu Municipality. The internal validity of the questions was Cronbach’s α=0.71.
After the pretest, the questionnaire was improved to help participants recall VCT events. Spaces were added to consider other relevant information on services provided. To avoid any unnecessary semantics and misunderstandings, the questionnaire was written in simple English and translated to Acholi, the main regional language. The translation from English to Acholi was conducted by the research team in conjunction with trained interviewers and interpreters from the Department of Language at Gulu University. As part of the interviews, participants were asked openended questions to describe their knowledge, attitude, hindrances, and VCT practices.
In addition, participants were required to restate the information to interviewers before entry into the questionnaire. The extra spaces added were used for qualifying remarks, which aided considerably in providing additional information that assisted researchers in filling the questionnaire accurately. Voluntary HIV counselling and testing (VCT) in this study was defined as a process whereby an individual, a couple, or a family receives voluntary HIV counselling and testing for HIV prevention, treatment, care, and support [5-7,10].
Data collection procedures: Upon consenting to the study, face-toface questionnaire interviews were conducted with participants within the OPD settings of GRRH, and each interview lasted between 45-60 minutes (Supplementary File A1). No more than five respondents were selected per day by each interviewer to ensure that adequate time for interviews was provided. The dependent variable for the study was voluntary HIV counselling and testing practices among participants.
Additionally, all nine researchers (coauthors) were trained on how to select, interview, and accurately record response of participants. Data collection process was supervised by the corresponding author, who was the academic supervisor of the research team. Researchers (5 males and 4 females) were medical students of Gulu University medical school in final year who had gathered enough experience on voluntary HIV counselling and testing. The research team visited the OPD, the site for data collection between 8:30 am and 5:30 pm on weekdays and between 9:00 pm and 2:00 pm on Saturdays. These hours were chosen because they were the most convenient stints for respondents to be interviewed. The average length for each interview was 40-60 minutes. Ultimately, interviews were conducted in English, as most respondents could speak and understand the English language well.
Determination of knowledge of participants: A knowledge rating scale was developed by the research team and used to determine knowledge grades for each participant. The questionnaire had six items covering basic information on knowledge on VCT. For every correct answer by a participant, a score of one point was awarded, and for a wrong one, a score of zero point. The aggregated scores for individual participants were computed and categorized as limited knowledge (scores less than 2 or <33.3%), average knowledge (scores between 2 and 4 or 33.3%-66.7%), and adequate knowledge (scores between 5 and 6 or 83.3%-100%) (Table 5).
Determination of attitudes of participants: A modified Likert scale was adopted by the research team to assess attitudes of participants in this study. There were six attitude items in the questionnaire. Each question on attitude was rated on a 5-point Likert scale as (0 for “strongly negative”, 1 for “negative”, 2 for “neutral”, 3 for “positive”, and 4 for “strongly positive”). The items on attitude to VCT were presented to participants expecting strongly positive as best answer for all six questions. This engrossed a maximum score of 24 points and a minimum of 0. The aggregated scores for participants were categorized as strongly negative for (<5 or <29%); negative for (5-10 or 29-41.7%); neutral for (11-16 or 45.8-66.7%); positive for (17-22 or 70.8-91.7%) and strongly positive for (23-24 or 95.8-100%) (Table 5).
In addition, the six items on attitudes towards VCT were further assessed with answers of “yes definitely”, “no”, “I am not sure”, “I do not know”, and “I do not care”. The aggregated participants’ scores and averages for each question were summarized in frequencies and percent (%) and tabulated accordingly (Table 2).
Determination of VCT practices among participants: Four openhanded questions were used to assess VCT practices among participants. Each question had a “yes” or “no” answer but with a follow-up question inviting participants to explain reasons for their answers. Each question with a correct answer (“yes”) was awarded 1 point, and for a wrong one (“no”), 0 point. The summation of each participant’s answers could reach a maximum of 4 points from a minimum of 0. The research team then graded VCT practices as poor (0), fair (1-2) and good (3-4) (Table 5).
Variables: Variables for this study population were the sociodemographic characteristics of participants (age, sex, address, occupation, tribe, religion, marital status, number of children, and highest level of education attained), knowledge, attitudes, hinderances and VCT practices.
Data quality control and assurance: To obtain quality data, all researchers were trained on data collection and how to select and administer face-to-face questionnaire interviews to research participants. Next, the questionnaire was pretested among adult patients attending OPD services at St Mary’s Hospital Lacor, a not-for-profit hospital that was six kilometers from Gulu Regional Referral Hospital where the main study was conducted. Results of the pretest were excluded from the main study; however, its findings were used to adjust questions in the questionnaire, ensuring that the required chronology and spaces for answers of participants were made. Last, questions in the questionnaire had an internal validity of Cronbach’s α=0.71.
Data analysis: Data were analyzed using the computer software program Statistical Package for Social Sciences (SPSS) version 17.0. Descriptive statistics are presented as frequencies, percentages, and tables. In this study, the primary unit of analysis was participants’ sociodemographic characteristics, knowledge, attitudes, practices, and hindrances to VCT. Furthermore, bivariate and multivariable logistical regression analyses were conducted on the data. For bivariate analysis, the chi square test (χ2) was used to assess associations between independent and dependent variables at 95% Confidence Intervals (95% CIs). At this point, any p-value less than 0.05 were considered statistically significant.
In addition, a multivariable logistic regression analysis was conducted to determine factors associated with VCT practices among adult patients attending OPD services at Gulu Regional Referral Hospital. All variables at the bivariate analysis with p-values less than or equal to 0.2 were entered into the final logistic regression model to determine independent factors associated with the dependent variable (VCT practices). Confounding was checked by observing whether addition of covariate(s) in the regression model caused changes in adjusted R square and the standardized coefficient Beta of the main exposure variable. Next, we tested the sensitivity of the final logistic regression model by adding covariates and conducting backward and forward adjustments on the model until the adjusted R square and the standardized coefficient Beta remained stable. At this point, we took values of standardized Coefficients Beta (β), t-values and p-values (at 95% Confidence Interval) in the final model as the independent factors associated with VCT practices among adult patients attending OPD services at Gulu Regional Referral Hospital. A p-value less than 0.05 was considered statistically significant.
Ethical considerations: Ethical approval for the study was obtained from Gulu University, Faculty of Medicine Research and Ethics Committee (Gulu IREC). Institutional approval was obtained from the administration of Gulu Regional Referral Hospital, and informed consent was obtained from each participant. The study was carried in accordance to relevant institutional guidelines and regulations. In addition, confidentiality, respect, privacy, and high moral principles were observed with respondents and their information during and after the study.
Results
Findings from this study displayed information obtained on VCT practices among adults attending outpatient department clinics at Gulu Regional Referral Hospital. The questionnaire completion rate was 380/384 (98.96%). Table 1 shows the socio-demographic characteristics of participants who were generally young adults in the age-group of 20-29 years 220/357(61.7%), females 217/372(58.3%), students 132/371(35.6%), catholic 220/377(58.4%), married 164/378(43.4%), Acholi 271/377(71.9%) and had attained ordinary level of education 130/376(34.6%). The male to female ratio was 1:1.4.
| Variables | Frequency (n=384) | Percent (%) |
|---|---|---|
| Ages (years) | ||
| <20 | 34 | 9.5 |
| 20-29 | 220 | 61.7 |
| 30-39 | 66 | 18.5 |
| 40-49 | 24 | 6.8 |
| 50-59 | 5 | 1.4 |
| 60-69 | 3 | 0.9 |
| >70 | 5 | 1.4 |
| Sub total | 357 | 100 |
| Sex | ||
| Male | 155 | 41.7 |
| Female | 217 | 58.3 |
| Sub total | 372 | 100 |
| Occupation | ||
| Students | 132 | 35.6 |
| Peasant Farmer | 83 | 22.4 |
| Business | 81 | 21.8 |
| Drivers | 14 | 3.8 |
| Others | 61 | 16.4 |
| Sub total | 371 | 100 |
| Highest level of education attained | ||
| No formal education | 24 | 6.4 |
| Nursery | 3 | 0.8 |
| Primary School | 69 | 18.4 |
| Ordinary level | 130 | 34.6 |
| Advanced level | 63 | 16.8 |
| Others | 87 | 23.1 |
| Sub total | 376 | 100 |
| Religion | ||
| Catholic | 220 | 58.4 |
| Protestant | 78 | 20.7 |
| Born Again | 46 | 12.2 |
| Muslim | 17 | 4.6 |
| Traditionalist | 6 | 1.6 |
| Others | 10 | 2.7 |
| Sub total | 377 | 100 |
| Tribes | ||
| Acholi | 271 | 71.9 |
| Baganda | 12 | 3.2 |
| Alur | 11 | 2.9 |
| Itesot | 21 | 5.6 |
| Langi | 36 | 9.5 |
| Lugbara | 4 | 1.1 |
| Banyankole | 6 | 1.6 |
| Others | 16 | 4.2 |
| Sub total | 377 | 100 |
| Marital status | ||
| Single | 159 | 42.1 |
| Married | 164 | 43.4 |
| Co-habiting | 25 | 6.6 |
| Separated/Divorced | 15 | 4.0 |
| Widowed | 13 | 3.4 |
| Others | 2 | 0.5 |
| Sub total | 378 | 100 |
Note: The Mmst participants were 20-29 years old 220/357(61.7%), females 217/372(58.3%), students 132/371(35.6%), had attained ordinary level of education 130/376(34.6%), catholic 220/377(58.4%), Acholi 271/377(71.9%), and married 164/378(43.4%).
Table 1: Socio-demographic characteristics of participants.
Table 2 describes the level of knowledge of participants regarding VCT. A total of 297/379 (78.4%) participants scored between 5 and 6, considered adequate knowledge, 61/379 (16.1%) scored between 2 and 4, considered average knowledge, and 21/379 (5.5%) scored between 0 and 1 and, considered limited knowledge. Three hundred and sixty (94.9%) participants knew how HIV status was determined, 358/379 (94.4%) had received information on VCT, 349/379 (92.1%) knew where VCT services were conducted, 311/379 (82.0%) knew the charges on VCT services, 297/379 (78.3%) knew VCT was a confidential activity, and 254/379 (67.0%) knew the closest VCT service site to them. The average knowledge score on VCT in this study population was 321/379 (84.7%).
| Responses (Frequency and %) | ||||
|---|---|---|---|---|
| Knowledge of participants | Yes (%) | No (%) | Not sure (%) | Total (%) |
| Are you aware how HIV status is determined? | 360(94.9) | 19(5.1) | 0(0.0) | 379(100) |
| Have you ever received information on VCT? | 358(94.4) | 21(5.6) | 0(0.0) | 379(100) |
| Do you know where VCT services are conducted in your area? | 349(92.1) | 22(5.8) | 8(2.1) | 379(100) |
| Do you know the charges for VCT services? | 311(82.0) | 18(4.8) | 50(13.3) | 379(100) |
| Do you know that VCT is a confidential activity? | 297(78.3) | 17(4.5) | 65(17.1) | 379(100) |
| Do you know how close a VCT service to you, the respondent? | 254(67.0) | 91(24.5) | 32(8.4) | 379(100) |
| Average | 321(84.8) | 32(8.4) | 26(6.8) | 379(100) |
| Attitudes of participants to VCT | Yes (%) | No (%) | Not sure (%) | Total (%) |
| Do you know that it is important to know one’s HIV status? | 351(92.3) | 8(2.1) | 21(5.6) | 380(100) |
| Do you know the benefits of knowing your HIV status? | 332(87.4) | 14(3.7) | 34(8.9) | 380(100) |
| Are you frightened by a test for HIV? | 181(47.7) | 163(42.8) | 36(9.5) | 380(100) |
| Do you believe in having enough information on HIV? | 203(53.4) | 177(46.6) | 0(0.0) | 380(100) |
| Are you aware of the importance of VCT? | 347(91.2) | 8(2.2) | 25(6.6) | 380(100) |
| Do you discuss freely your VCT results with your partner? | 323(85.1) | 40(10.6) | 16(4.3) | 380(100) |
| Average | 290(76.2) | 69(18.3) | 21(5.6) | 380(100) |
Note: The most participants had adequate knowledge on voluntary HIV counseling and testing (VCT). This was because most respondents knew how HIV status was determined 360/379(94.9%), had received VCT information 358/379(94.4%), knew where VCT services were conducted 349/379(92.1%), knew the charges on VCT services 311/379(82.0%), knew that VCT was a confidential activity 207/379(78.3%), and knew how close the service was to the participant 254/379(67.0%). For attitudes, the majority knew the importance of knowing one’s HIV status 350(92.3%), knew the benefits of knowing one’s HIV status 332(87.4%), frightened by a HIV test 181(47.7%), believed in having enough VCT information 203(53.4%), aware of the importance of VCT 347(91.2%) and discussed VCT results freely with partner 323(85.1%).
Table 2: Knowledge and attitudes of participants on voluntary HIV counselling and testing (VCT).
Attitudes of respondents on VCT are highlighted in Table 2. Most responses were as follows: 351/380(92.3%) said it was important to know one’s HIV status, 332/380(87.4%) it was beneficial to know one’s HIV status, 181/380(47.7%) were frightened by the HIV test, 203/380(53.4%) believed there was a need for getting enough information on HIV, 347/380(91.2%) said they were aware on the importance of VCT, and 323/380(85.1%) discussed their VCT results freely with their partners. The average response rate for the six questions on attitude was 290/380 (76.2%) (Table 2).
Table 3 describes participants’ opinion on why they had not undertaken VCT and reasons for their actions. Participants observed fear of stigmatization from community 4/10(40.0%), fear of divorce or separation from spouses 4/10(40.0%) and old age 1/8(13.5%) as reasons for their action. In addition, most participants 197/374(51.3%) preferred someone trained in VCT as best VCT service provider, followed by doctors 107/374 (28.6%) and nurses 9/374 (2.4%). The preferred sites for accessing VCT services were hospitals 172/376(45.7%), VCT centers 154/376(41.0%), and homes 28/376(7.4%). The preferred sources of VCT information were radios 236/372(63.4%), schools 57/372(15.3%) and parents 30/372(8.1%).
| Variables | Frequency | Percent (%) |
|---|---|---|
| Reasons for not undertaking VCT | ||
| There is no reason for not undertaking VCT | 7 | 87.5 |
| I am too old to care on VCT | 1 | 13.5 |
| Sub total | 8 | 100.0 |
| Reasons for believing that knowing HIV status was not beneficial | ||
| Fear of stigmatization from community members | 4 | 40.0 |
| Its personal | 2 | 20.0 |
| Fear of divorce/separation from spouses | 4 | 40.0 |
| Sub total | 10 | 100.0 |
| Reasons why one should not be afraid of testing for HIV and AIDS | ||
| There is no reason | 74 | 50.0 |
| Wanting to know and accept their own status | 27 | 18.2 |
| Felt it would help in early treatment | 13 | 8.8 |
| Had predetermined reasons | 19 | 12.8 |
| Would opt to live positively if found HIV positive | 13 | 8.8 |
| It could reduce the HIV prevalence | 2 | 1.4 |
| Sub total | 148 | 100.0 |
| Best VCT service providers | ||
| Anyone trained on VCT | 197 | 51.3 |
| Doctors | 107 | 28.6 |
| Any medical worker | 36 | 9.6 |
| Nurses | 9 | 2.4 |
| I do not know | 30 | 8.0 |
| Sub total | 374 | 100.0 |
| The preferred sites for accessing VCT services | ||
| Hospitals | 172 | 45.7 |
| VCT Centers | 154 | 41.0 |
| Workplaces | 3 | 0.8 |
| Homes | 28 | 7.4 |
| The place does not matter | 19 | 5.1 |
| Sub total | 376 | 100.0 |
| What is your preferred source of VCT information? | ||
| Radios | 236 | 63.4 |
| Schools | 57 | 15.3 |
| Parents | 30 | 8.1 |
| Friends | 29 | 7.8 |
| Others | 20 | 5.4 |
| Sub total | 372 | 100.0 |
Note: The most participants preferred hospitals for accessing VCT services 172/376(45.7%), best VCT services were provided by someone trained on VCT 197/374(51.3%), radios as the best means for conveying VCT information 236/372(63.4%), there was no reason for fearing to test for HIV 74/148(50%), and the main reason for not undertaking VCT was the fear of divorce/separation with spouses 4/10(40%) or stigma 4/10(40%), and there was no specific reason for not undertaking VCT services 7/8(87.5%).
Table 3: Reasons why participants do not undertake VCT.
Table 4 describes VCT practices among participants with majority expressing ignorance on the importance of VCT services 13/45(28.9%), some feared receiving a positive test result 9/45(20.0%), others had busy work schedule 6/45(13.3%), and one said he was too old to participate in VCT services 1/8(12.5%). The report showed that many participants feared that their conditions would become worse when they got to know their HIV status 1/18 (5.6%) and that VCT was too risky and painful process 2/18 (11.2%). In addition, some preferred VCT to be undertaken anytime 266/373 (71.3%), just before marriage 70/373 (18.8%) and others when they were feeling very sick 26/373 (7.0%).
| Variables | Frequency | Percent (%) |
|---|---|---|
| Reasons for not undertaking VCT by participants | ||
| Ignorant on the importance of HIV testing | 13 | 28.9 |
| They had predetermined results | 11 | 24.1 |
| Scared of a positive test result | 9 | 20.0 |
| Busy work schedule | 6 | 13.3 |
| VCT service centers were far | 5 | 11.1 |
| They thought they were too old | 1 | 2.2 |
| Sub total | 45 | 100 |
| Reasons for discouraging people from testing for HIV | ||
| The fear of their condition becoming worse | 1 | 5.6 |
| It’s a risky and painful process | 2 | 11.2 |
| Applicable but no answer | 15 | 83.3 |
| Sub total | 18 | 100 |
| When is the right time for undertaking VCT? | ||
| I prefer to go for VCT anytime I want | 266 | 71.3 |
| I want to do it just before marriage | 70 | 18.8 |
| When I am feeling sick | 26 | 7.0 |
| For any unspecified time | 11 | 2.9 |
| Sub total | 373 | 100 |
| Practices of respondents on VCT | Yes (%) | No (%) |
| Have you ever undertaken a HIV test? | 312(82.0) | 68(18.0) |
| Have you ever undertaken VCT with your partner? | 185(48.8) | 195(52.2) |
| Have you ever encouraged people to undertake VCT? | 189(76.1) | 91(24.9) |
| Have you ever discouraged people from undertaking VCT? | 362(95.2) | 18(4.8) |
| Average | 287(75.5) | 93(24.5) |
Note: The most participants did not know the importance of VCT 11/45(28.9%), there was no reason for discouraging people from undertaking VCT 362/380(95.2%) and that the preferred time for undertaking VCT was anytime 266/373(71.3%). In the assessment for VCT practices, most participants 312(82.0%) had tested for HIV, 195(52.2%) had not undertaken VCT with their partners, 189(76.1%) had encouraged others to undertake VCT, and 362(95.2%) had discouraged others from undertaking VCT.
Table 4: Practices of participants to VCT.
In Table 5, knowledge, attitudes, and practices of participants on VCT were presented, with majority having adequate knowledge (297/379, 78.4%), positive attitudes (151/380, 39.7%), strongly positive attitudes (158/380, 41.6%) and good VCT practices (299/380, 78.7%).
The modified Likert scale used showed the following: strongly negative 7/380(1.8%), negative 13/380(3.4%), neutral 51/380(13.4%), positive 151/380(39.7%), and strongly positive attitudes 158/380(41.6%) (Table 5).
| Variables | Frequency | Percent (%) |
|---|---|---|
| Level of knowledge of respondent on VCT | ||
| Limited | 21 | 5.5 |
| Average | 61 | 16.1 |
| Adequate | 297 | 78.4 |
| Sub total | 379 | 100.0 |
| Attitudes of respondents to VCT | ||
| Strongly negative | 7 | 1.8 |
| Negative | 13 | 3.4 |
| Neutral | 51 | 13.4 |
| Positive | 151 | 39.7 |
| Strongly positive | 158 | 41.6 |
| Sub total | 380 | 100.0 |
| Practices of respondents to VCT | ||
| Poor | 20 | 5.3 |
| Average | 61 | 16.1 |
| Good | 299 | 78.7 |
| Subtotal | 380 | 100.0 |
Note: Most participants had adequate knowledge (297/379, 78.4%), with a strongly positive attitude (158/380, 41.6%) and good practices for VCT (299/380, 78.7%).
Table 5: Grading knowledge, attitude, and practices of participants to VCT.
In the bivariate analysis, associations between dependent (VCT practices) and independent factors (knowledge and attitudes) were assessed using a three-by-three table, as shown in Table 6. Statistically significant associations between VCT practices and knowledge (χ2=0.613, p<0.001) and between VCT practices and attitudes (χ2=0.509, p<0.001) were observed.
| Variables | Knowledge | Attitudes | Practices | |
|---|---|---|---|---|
| Knowledge | Pearson Correlation 1 | 1 | ||
| Sig. (2-tailed) | ||||
| N | 379 | |||
| Attitudes | Pearson Correlation 1 | 0.528(**) | 1 | |
| Sig. (2-tailed) | 0.000 | |||
| N | 379 | 380 | ||
| Practices | Pearson Correlation 1 | 0.613(**) | 0.509(**) | 1 |
| Sig. (2-tailed) | 0.000 | 0.000 | ||
| N | 379 | 380 | 380 |
** Correlation is significant at the 0.01 level (2-tailed).
Note: The relationships between knowledge and attitude, attitude and practices, and knowledge and practices to VCT among participants. The results showed that there was a strong positive association between knowledge and VCT practices of participants (χ2=0.613, p<0.001), and there were moderate positive correlations between knowledge and attitude (χ2=0.528, p<0.001) and between attitude and practice (χ2=0.509, p<0.001). All these correlations were statistically significant with a high probability value of 0.000 in each case at 99% confidence intervals.
Table 6: Relationships between Knowledge, Attitudes and Practices to VCT.
In the multivariable logistic regression analysis, factors associated with VCT practices among adults in Gulu Regional Hospital were knowledge and attitudes. This was described in Table 7a, which showed that VCT practices were explained by attitude and knowledge up to 42.1% (Adjusted R Square=0.421; Sig. F Change=0.000). Other factors accounted for the remaining 57.9%. This regression analysis finding represents the significant relationship between independent and dependent variables.
| Model | R | R square | Adjusted R square | Standard error of the estimate | Change statistics | ||||
|---|---|---|---|---|---|---|---|---|---|
| R square change | F Change | df1 | df2 | Sig. F change | |||||
| 1 | 0.651(a) | 0.424 | 0.421 | 1.115 | 0.424 | 138.299 | 2 | 376 | 0.000 |
Note: The independent variables (attitude and knowledge) predict the dependent variable practice is indicated by the coefficient of determination (adjusted R Square). Thus, Table 7 indicates that VCT practice is explained by attitude and knowledge up to 42.1% (Adjusted R Square=0.421; Sig. F Change=0.000). Other factors accounted for the remaining 55.9%. This is a substantial finding considering that regression analysis may describe the cause-effect relationship.
Table 7a: Regression analysis on knowledge, attitude, and practices on VCT.
In Table 7b, the multivariable analysis found the determinants of VCT practices as knowledge (β=0.478, t=10.374, p<0.001) and attitudes (β=0.257, t=5.570, p<0.001).
| Model | Un-standardized Coefficients | Standardized coefficients | t | Sig. | ||
|---|---|---|---|---|---|---|
| B | Std Error | Beta | ||||
| 1 | Constant | 0.933 | 0.293 | 3.189 | 0.002 | |
| knowledge | 0.386 | 0.037 | 0.478 | 10.374 | 0.000 | |
| Attitude | 0.194 | 0.035 | 0.257 | 5.57 | 0.000 | |
Note: Indicates the best explanatory variable for VCT practices as knowledge (beta=0.478; t=10.374, p=0.000). This means that a unit change in knowledge causes a 47.8% variation in VCT practices. In addition, a unit variation in attitude caused 25.7% variation in VCT practice (beta=0.257; t=5.570, p=0.000). This variation in VCT practices is statistically significant at the 95% confidence interval. The prediction equation proposed by the regression model on VCT practices is given as VCT Practice = 0.478 VCT Knowledge+0.257 VCT Attitude. The implication for this finding is that more resources could be invested in offering knowledge in addition to delivering attitude change to VCT practices among patients attending OPD services a GRRH.
Table 7b: The Regression coefficients suggesting the predictive model for the variables.
Discussion
The most significant findings were that knowledge and attitude significantly affect practices on voluntary HIV counselling and testing among adults attending outpatient clinics at Gulu Regional Referral Hospital. This was presented by a formula from the regression analysis as VCT practices=0.478 VCT knowledge+0.257 VCT attitude.
This finding suggests that investing in knowledge and attitude can significantly influence practices on voluntary HIV counselling and testing among the study population. This finding has implications on how VCT practices could be improved in this community, for example, by increasing information on VCT, it would improve knowledge and attitudes of community members to undertake VCT services. The Ugandan Ministry of Health and administration of Gulu Regional Referral Hospital could take advantage of this finding to increase VCT uptake in this community by making IEC materials readily available and using radio talk shows for reaching out to community members explaining the importance of VCT services in access and care for HIV and AIDS patients. This could become very useful, as statistics show that the incidence and prevalence of HIV is slowly and steadily increasing in Northern Uganda, disrupting the gains already achieved by Uganda over the bane of HIV and AIDS.
The sociodemographic characteristics of participants were comparable to many studies conducted in Northern Uganda [5-7,10], where most respondents were young adults in their productive agegroup of 20-29 years, females in the ratio of 1.4:1 to males and the majority were students, not married and had attained ordinary level of education (Table 1). Other sociodemographic data, such as tribe, occupation, and religion, were consistent with the pattern of population distribution in Northern Uganda and did not significantly affect VCT practices in this study population [5-7,10].
To our knowledge, most participants in the current study had adequate VCT knowledge on what, why, how, where and when VCT services were conducted (Table 2). Similarly, a study conducted among students at a polytechnic in southeastern Nigeria found 115 (63.2%) students were aware of VCT services, with 68 (59.1%) having heard about it a year prior to the study [14]. In addition, mass media and churches were the most common sources of VCT information [14]. However, most students did not know where VCT services could be obtained, and their knowledge on VCT was low [14]. Nevertheless, 127 (69.8%) students approved the need for counselling prior to testing, and 117 (64.3%) were ready to take a positive test result in good faith [14]. Similarly, the commonest source of VCT information for the current study was radios and schools, while parents were the least common (Table 3). Similarities observed in the two studies have implications on how the application of this information could become strategy to augment VCT knowledge, attitudes, and practices. These authors suggest that line ministries in Uganda and Nigeria could use radios, schools, and churches as means for engaging, mobilizing, and sensitizing the population on voluntary HIV counselling and testing. This was expected to generate positive impacts in the fight against HIV, which was beginning to heave in the two African communities.
It is important to know one’s HIV status because it is considered the first step in accessing health care and preventing further infection with HIV and AIDS [5,15]. Knowledge on test results enables an individual to initiate and maintain safer behaviors to prevent acquiring HIV and other sexually transmitted diseases (STDs) and, if found positive, to stop infecting others and gain early access to HIV-specific care, treatment, and support [2]. Additionally, voluntary counselling and testing for HIV have been established as one of the most effective strategies for early access to HIV and AIDS treatment, support, and care [2,5-7,10,16-19].
Furthermore, a study conducted among healthcare students undertaking professional courses at certificates, diplomas, and degrees showed multiple responses with respect to sources of VCT information [20]. The commonest sources of information were from radios, televisions, friends, schools, church seminars, and VCT centers [20]. Most participants in that study held the view that VCT was important and enabled individuals to know their HIV status [20].
These authors suggest that information obtained from this current study could be used to strengthen information sharing among career professionals, and hopefully this would improve their VCT knowledge, and they become champion for VCT services in communities where they work. This was expected to have long-term and sustainability effects on VCT practices in their communities.
Furthermore, a comparative study conducted by Kalichman and Simbayi (2003) revealed that individuals who were not tested for HIV demonstrated significantly more AIDS-related stigmas, ascribing greater shame, guilt and social disapproval to people living with HIV and AIDS [21]. As previously seen, the problem of stigma has had profound effects on the fight against HIV in many communities in Africa [21]. It has been one of the drivers of HIV spread, mental health issues, and family problems, for example, domestic violence, separation, divorce, family neglect and unstable families in many communities in Africa [21].
These authors suggest a need for a comprehensive analysis on the root causes of stigma, its values, and concerns in the spread of HIV and AIDS in many communities in Africa. This is because most studies in Africa have shown stigma as one of the main drivers for poor participation in VCT services, treatment, support, and care for HIVaffected populations in many African communities.
Regarding attitudes in the current study, most participants had strongly positive attitude towards VCT (Table 3). Most respondents agreed that it was necessary to know their HIV status, although a minority was frightened to get tested and believed they had enough information on VCT (Table 3). Some participants believed that knowing their HIV and AIDS status was not beneficial because they feared the level of stigma they would go through in their communities in addition to the risk of divorce/separation from their spouses (Table 3). Similar findings were observed in [6,7,21], where stigma and fear of separation with spouses were cited.
These authors were mesmerized by participants who were afraid of taking HIV and AIDS tests for which they had no rock-hard reason for doing so (Table 4). This contrasts with a comparative study conducted in Nigeria among graduate students in a polytechnic school that found that 64.3% were ready to take a positive test result in good faith [14]. Their findings contrast with our current study, perhaps due to differences in sociodemographic characteristics, countries of study and differential advances in the spread and control of HIV in the two countries. Differences in the two studies were not new, as authors argue that these were behavioral and social sciences surveys where opinions and perspectives of individuals and communities change with time and were affected by circumstances, environment, study population and time of the survey.
Notably, a Ugandan 2000-2001 Demographic Health Surveys (DHS) found that 8.4% of women and 12.0% of men had tested for HIV with women in their 20s, and men aged 25-39 years, the most tested [22]. In addition, respondents living in urban areas, in Kampala district and those with secondary education were the most likely to have undertaken HIV counselling and testing [22]. However, among those who had not tested, 63.7% and 65.4% of women and men wanted to have a HIV test, respectively [22]. The report showed that many respondents were afraid of seeking HIV services because they feared stigma and discrimination by their families and communities [5,6,10,23]. This information highlights the reason why VCT services should always preserve individual client’s confidentiality so that they do not suffer the distress of stigma in their communities [5,6,10,23].
Studies have shown that if VCT services were properly carried out, they helped break the vicious circle of fear, stigma, and denials, which propagated the spread of HIV in many communities in Africa [5,6,10,23]. Interestingly, in some circumstances, people asked for partners, relatives, and friends to be present during VCT processes, especially at the declaration of test results [23]. Furthermore, some participants preferred to receive their test results within the privacy of their homes [24]. Therefore, VCT could be promoted as a preventive measure and an entry point to support and care for those tested positive for HIV [24]. This has important implications that it could increase the number of couples attending VCT services in the fight against HIV and AIDS pandemics in their communities [23].
This finding is supported by a study conducted by the United States Centre for Disease Control and Prevention (CDC) and Uganda Virus Research Institute (UVRI), which found that the VCT model concentrating on home-based provision of counselling and receiving HIV test results was highly acceptable and greatly increased the proportion of those who received HIV test results compared to others [25]. These researchers suggested that their findings could be attributable to transport costs, which were often barriers to access to VCT, even though VCT services were freely offered in Uganda [25].
Furthermore, there were reportedly several psychosocial influences on women’s accessibility and utilization of VCT services more than men [26]. Partly, the psychosocial influence emanated from the community’s responses, personal beliefs, and attitudes towards VCT services [26]. Notably, the socioeconomic factors that could explain this vulnerability were that women were less mobile, had fewer economic possibilities for seeking treatment due to high transport costs to centers providing VCT services, unequal power relations whereby women often needed the approval of their husbands and family for health visits, and a low level of education among women [26].
In regard to VCT practices in the current study, most participants had good practices, reported having tested for HIV and AIDS, and encouraged others to undertake VCT (Table 4). This finding contrasts with a previous study conducted in Gulu in 2011, where only 36.1% of respondents had undertaken VCT, while 63.9% had not [5]. These authors argue that these differences in VCT practices were due to differences in the years when the two studies were conducted and ages of the study populations. Similarly, a study conducted in Rakai (Uganda) found that 93% (9,910 of 10,618) of respondents requested their HIV test results at the first instant [27]. Test result requests were higher among persons aged 15-24 years, those who had never married persons with no formal education and persons who reported no sexual partners in the past six months [27]. In addition, there were no differences in test result requests between female and male respondents (93% and 94%, respectively). However, HIV test result requests were highest among persons who had prior VCT from the Rakai Program (96.1%) and among those with self-reported VCT results (95.7%) but lowest among individuals with no prior VCT (90.1%) [27]. Too, reported in the same study was that the uptake of VCT results delivered at home rose from 35% in the first year of study in 1994–5 to 65% in 1999–2000 [27]. Additionally, a study conducted in rural Uganda found that the overall VCT uptake among men was low at only 23.3% [28]. This finding was similarly observed in another study conducted in a black township in Cape Town, South Africa, where only 47% of participants self-reported having undertaken HIV tests [21]. These studies above show that VCT uptake in many communities in Africa have remained low, which may explain the rising incidence and prevalence of HIV and AIDS in many communities in Africa.
Additionally, a multicenter study conducted among university undergraduates in South Africa, India and the USA reported that only 20% of South Africans and Americans, and 10% of Indian students had undergone HIV testing [29]. Beguilingly, all these studies show that people who underwent VCT were fewer but were in better position to promote prevention and control of HIV. For these reasons, knowledge, attitude, hindrances, and practices on VCT among adults should always be assessed and analyzed appropriately to help design appropriate intervention measures for the affected communities in Africa.
It is important to note from this current study that improvement in knowledge and attitudes of participants on VCT services also significantly improved their VCT practices (Tables 5-7). The explanatory model derived from this multivariable regression analysis could perhaps be important in understanding and improving VCT uptake in this community, where HIV incidence and prevalence have steadily been rising for several years.
The implication of these findings is that in the long run, if this information is used appropriately by the Ugandan Ministry of Health, it could support improvement in VCT practices in this community, a place where prevention of HIV has become paramount. Curiously, this study confirms the long-held view in Uganda’s successful story for reducing the prevalence of HIV and AIDS more than any other African countries from a double digit to a single digit over the last two decades [30-35]. In the current situation of Northern Uganda, the incidence and prevalence of HIV and AIDS are increasing. These authors argue that Uganda ought to go back to the drawing board to reverse the downturn in the increasing incidence and prevalence of HIV and AIDS, and maintains the gains achieved over the years.
In the 2020 report released by the Uganda AIDS Commission (UAC), Gulu District had the highest prevalence of HIV and AIDS in Northern Uganda [9]. At 14.0%, the prevalence rate of HIV in Gulu was higher than the national average at 6.0% compared to Northern Uganda’s statistics, which stood at 7.0% [9]. In addition, the UAC report showed that HIV prevalence in Northern Uganda was higher in females at 17.1% than in males at 8.0%. Accordingly, the UAC report showed that higher prevalence of HIV in Gulu District and Northern Uganda in general was attributable to many factors, for example residents having multiple sexual partners, low uptake of safe male circumcision, high level of community stigma, enormous poverty among the population and many other reasons, such as poor traditional practices and beliefs, wife inheritance, immense youth unemployment, and rapid urbanization, which have led to increased population, poor lifestyles, and poor social determinants of health in the region [9].
Therefore, in the 2020 UAC report, the District Health Officer of Gulu District reported that there were 27,000 people living with HIV in the district [9]. However, he revealed that many persons reported to be living with HIV and AIDS in Gulu were from neighboring districts but receive their antiretroviral drugs (ARVs) from Gulu District, particularly from Gulu Regional Referral Hospital, TASO Gulu and St. Mary’s Hospital, Lacor. He argued that this may in part explain the reported high prevalence of HIV in the Gulu District because the district was the regional hub of the region [9].
These authors contend that HIV and AIDS prevalence challenges in Gulu District were enormous. To address issues of high HIV prevalence, there was need to address VCT knowledge, attitudes, and practices in the community. To increase VCT uptake in this community, knowledge, attitudes, and confidentiality of VCT reports were critical. This was because stigma to persons living with HIV and AIDS (PWLHAs) would reduce people's willingness to have themselves tested for human immunodeficiency virus (HIV), thereby reducing the number of people who openly declare their HIV status and thus increase the risk of HIV transmission in communities since most sufferers would go underground.
Strengths and Limitations of this Study
This was hospital-based data derived from patients attending outpatient clinics at Gulu Regional Referral Hospital, and information generated should be interpreted in the context of a hospital setting. This may have created selection biases, as all information obtained were from patients, and this may not reflect accurate information from the general population of Gulu and northern Uganda. Moreover, data were obtained from only one regional hospital. However, as observed, the diversity of participants cutting across different sociodemographic characteristics, for example, gender, age, occupation, and tribes, give strength and diversity of information obtained, which were similarly observed in previous studies conducted in the region. Of interest was that GRRH is a public hospital that offers free health services to every person. The hospital has general outpatient and specialized clinics that offer unlimited access to medical services. The free medical services offered at GRRH may have reduced barriers to access to participants we interviewed and therefore a strength for this study.
Second, the questionnaire we used was not derived from a validated questionnaire to determine knowledge, attitude and VCT practices of participants however, we pretested the questionnaire in a nearby hospital, and the internal validity was Cronbach’s α=0.71, which was acceptable for the information we obtained.
Generalizability of these results
The results from this study could be generalized to most hospitalbased data in Uganda, especially regional hospitals that are situated in cosmopolitan urban centers in Uganda.
Conclusion
The most significant findings from this study were that adequate knowledge and positive attitudes significantly influence practices on voluntary counselling and testing for HIV and AIDS in adult population attending outpatient services at Gulu Regional Referral Hospital. However, factors such as stigma, discrimination, fear of divorce and separation from spouses, and lack of or inadequate information from parents may still hamper the flow of VCT information to the young population. Our study found that increasing knowledge and changing attitudes towards VCT could significantly improve VCT practices among the study population.
We recommend the following actions
• To conduct more studies to assess factors associated with poor VCT information transmission from parents.
• Use radios and schools for VCT information transmission to the population. Proposed and new policy on VCT should be communicated over radios and schools for wider dissemination to the population.
• To strengthen measures that reduce HIV and AIDS stigma in the community.
• To increase and strengthen VCT practices among 20–29-year-olds (5) to conduct studies to determine factors associated with poor VCT uptake in this community. According to the current study, 86% of participants had no reason(s) for not knowing their HIV status.
Declarations
Ethics approval and consent to participate
This study was approved by Gulu University IREC, and all participants consented to the study. In addition, the study was carried in accordance with the relevant institutional guidelines and regulations.
Consent for Publication
All participants consented to the publication of information derived from this study.
Availability of Data and Material
All datasets supporting the conclusion in this article are within this article and can be access by a reasonable request to the corresponding author.
Competing Interests
All authors declare no conflicts of interest.
Funding
Part of the funding for this study was obtained from Gulu University, an academic institution where these researchers were faculty and medical students. However, most funding was derived from contributions of individual researchers.
Authors' Contributions
All authors participated in the protocol design, literature review, ethical approval, data collection, data analysis and preparation of this manuscript for publication.
Acknowledgement
We acknowledge with many thanks the support from the administration of Gulu Regional Referral Hospital for the information obtained. Financial support from Gulu University, which enabled the team to conduct this study successfully, is most appreciated.
References
- UNAIDS (2000) Voluntary Counseling and Testing (VCT), UNAIDS Technical Update.
- Kawichai S, Beyrer C, Khamboonruang C, Celentano D, Natpratan C, et al. (2004) HIV incidence and risk behaviours after voluntary HIV counselling and testing (VCT) among adults aged 19-35 years living in peri-urban communities around Chiang Mai city in northern Thailand, 1999. AIDS Care 16:21-35.
- NHSBS (2007) Uganda Ministry of Health, HIV Sero, and behavioral survey: Ministry of Health (2004/2005).
- Ministry of Health (MOH) Uganda and ORC Macro: Calverton, Maryland, USA (2006) Uganda HIV/AIDS Sero-Behavioral Survey 2004-2005.
- Kitara DL, Ecik C (2011) The youths’ perspective on HIV/AIDS counseling and testing (HCT) in Gulu, Northern Uganda. A cross-sectional study. J Med Med Sci 2:812-820.
- Kitara DL, Amone C, Okello C (2012) Knowledge and misconceptions about HIV counseling and testing (HCT) among the post-conflict youths of Gulu, Northern Uganda. A prospective study design. Pan Afr Med J 6:12.
- Kitara DL, Aloyo J (2012) HIV/AIDS stigmatization, the reason for poor access to HIV counseling and testing (HCT) among the youths in Gulu (Uganda). Afr J Infect Dis 6:12-20.
- Uganda (2012) Ministry of Health, ICF International (Firm). Uganda AIDS indicator survey 2011.
- Uma P (2020) Gulu records highest HIV prevalence in Northern Uganda. Chimp Reports.
- Kitara DL, Nakitto A, Aloyo JK, Mwaka AD (2013) HIV/AIDS among youths in Gulu: A post-conflict northern Uganda. Pac J Med Sci 12:10-23.
- Pathfinder International (1999) Africa Regional Office. Adolescent Reproductive Health in Africa: Paths into the Next Century. Nairobi, Kenya: The Office.
- UNAIDS (1995) Knowledge is power: Voluntary HIV counseling and testing in Uganda.
- Caldwell JC (2000) Rethinking the African AIDS epidemic. Popul Dev Rev 26:117-135.
- Ikechebelu IJ, Udigwe GO, Ikechebelu N, Imoh LC (2006) The knowledge, attitude and practice of voluntary counselling and testing (VCT) for HIV/AIDS among undergraduates in a polytechnic in south-east Nigeria. Niger J Med 15:245-249.
- World Health Organization (2002) Report of a WHO Consultation. Geneva, Switzerland.
- Baggale R, Kayawe I, David Miller (2001) Counseling, testing and psychosocial support in HIV/AIDS prevention and care in resource constrained settings: A handbook for the design and management of programs, ed. Peter R. Lamptey and Helene D. Gayle 547-78
- Holtgrave D, McGuire J (2007) Impact of counseling in voluntary counseling and testing programs for persons at risk for or living with HIV infection. Clin Infect Dis 45:240-243.
- Robles RR, Matos TD, Colón HM, Marrero CA, Reyes JC (1996) Effects of HIV testing and counseling on reducing HIV risk behavior among two ethnic groups. Drugs Soc 9:173-184.
- Coates TJ (2000) Efficacy of voluntary HIV-1 counselling and testing in individuals and couples in Kenya, Tanzania, and Trinidad: A randomised trial. Lancet. 356:103-112.
- Charles MP, Kweka EJ, Mahande AM, Barongo LR, Shekalaghe S, et al. (2009) Evaluation of uptake and attitude to voluntary counseling and testing among health care professional students in Kilimanjaro region, Tanzania. BMC Public Health 9:128.
- Kalichman SC, Simbayi LC (2003) HIV testing attitudes, AIDS stigma, and voluntary HIV counselling and testing in a black township in Cape Town, South Africa. Sex Transm Infect 79:442-447.
- Uganda Bureau of Statistics and ORC Macro, Uganda Demographic and Health Survey 2000-2001 (2001) Uganda Bureau of Statistics and ORC Macro: Calverton.
- TASO (Uganda) (1994) The Inside Story, Participatory Evaluation of HIV/AIDS Counseling, Medical and Social Services, 1993-1994.
- Were W, Mermin J, Bunnell R, Ekwaru JP, Kaharuza F (2003) Home-based model for HIV voluntary counselling and testing. Lancet 361:1569.
- Kaleebu P, Kamali A, Seeley J, Elliott AM, Katongoleâ€Mbidde E (2015) The Medical R esearch C ouncil (UK)/U ganda Virus Research Institute Uganda Research Unit on AIDS ‘25 years of research through partnerships’. Tro Med Int Health 20:1.
- Evening K (2001) HIV/AIDS and Gender-An Awareness Raising Folder, Norwegian Working Group on HIV/AIDS and Gender, Oslo, Norway.
- Matovu JK, Kigozi G, Nalugoda F, Wabwireâ€Mangen F, Gray RH (2002) The Rakai Project counselling programme experience. Trop Med Int Health 7:1064-1067.
- Bwambale FM, Ssali SN, Byaruhanga S, Kalyango JN, Karamagi CA (2008) Voluntary HIV counselling and testing among men in rural western Uganda: Implications for HIV prevention. BMC Public Health 8:1-2.
- Peltzer K, Nzewi E, Mohan K (2004) Attitudes towards HIV-antibody testing and people with AIDS among university students in India, South Africa and United States. Indian J Med Sci 58:47-60.
- Serwadda D, Sewankambo NK, Carswell JW, Bayley AC, Tedder RS, et al. (1985) Slim disease: A new disease in Uganda and its association with HTLV-III infection. The Lancet 326:849-852.
- UNSS (Uganda National Sero-Surveillance survey) (2008) Uganda National Sero-Survey (UNSS of 2004/2005).
- UNDP (United Nations Development Partner) (2008) Macro-economy HIV/AIDS assessment in Uganda.
- Epstein H (2007) The invisible cure: Africa, the West, and the fight against AIDS. Macmillan.
- Horizons HI (2001) voluntary counseling and testing among youth: Results from an exploratory study in Nairobi Kenya and Kampala and Masaka Uganda. Washington: Population Council.
Citation: Aduk MA, Atama IM, Dayo LD, Kizza CN, Musinguzi BC, et al. (2022) Voluntary HIV Counselling and Testing (VCT): Knowledge, Attitudes, Hindrances, and Practices of Adults Seeking Treatment at Gulu Regional Referral Hospital on the Spread of HIV in Northern Uganda. A Cross-Sectional Study. J Infect Dis Ther S6:002
Copyright: © 2022 Aduk MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 3053
- [From(publication date): 0-2021 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 2416
- PDF downloads: 637
