Research Article Open Access
Prognostic Factors in Pancreatic Cancer: The Role of Perineural, Vascular and Lymphatic Invasion and of Ca19-9
Berardi R1*, Mandolesi A2, Pellei C1, Maccaroni E1, Onofri A1, Lucarelli A1, Biagetti S2, Alfonsi S2, Caramanti M1, Savini A1, Bearzi I2 and Cascinu S1
1Clinica di Oncologia Medica, Università Politecnica delle Marche, Azienda Ospedaliero-Universitaria Ospedali Riuniti Umberto I - GM Lancisi - G Salesi, Ancona, Italy
2Anatomia Patologica, Università Politecnica delle Marche, Azienda Ospedaliero-Universitaria Ospedali Riuniti Umberto I - GM Lancisi - G Salesi, Ancona, Italy
- *Corresponding Author:
- Rossana Berardi
Medical Oncology Unit
Università Politecnica delle Marche-Azienda Ospedaliero-Universitaria
Ospedali Riuniti Umberto I – Lancisi – Salesi di Ancona
Via Conca 71 - 60126 Ancona - Italy
Tel: +39 071 5965715
Fax: +39 071 5965053
E-mail: r.berardi@univpm.it
Received date: May 20, 2013; Accepted date: August 26, 2013; Published date: August 29, 2013
Citation: Berardi R, Mandolesi A, Pellei C, Maccaroni E, Onofri A (2013) Prognostic Factors in Pancreatic Cancer: The Role of Perineural, Vascular and Lymphatic Invasion and of Ca19-9. J Gastroint Dig Syst 3:134. doi: 10.4172/2161-069X.1000134
Copyright: © 2013 Berardi R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Objective: The aim of our analysis was to investigate the impact of perineural, vascular and lymphatic invasion and of CA19-9 on survival in patients with locally advanced and metastatic pancreatic cancer, with the objective to serve as a tool for a more accurate and rational treatment selection. Methods: We analyzed 181 consecutive patients with locally advanced unresectable pancreatic cancer and metastatic pancreatic cancer who received chemotherapy at our Institution between 2000 and 2010. Results: At univariate analysis CA19-9 represented a prognostic factor (median overall survival if CA19-9 ≤ 37 U/ml vs. >37 U/ml was 18.49 vs. 9.21 months, respectively, p=0,0004), while surprisingly the presence of vascular, lymphatic and perineural invasion was found to be a favorable prognostic factor (median overall survival in patients with invasion vs. without invasion was 27.5 vs. 9.6 months, respectively, p=0.0002).At multivariate analysis the presence of invasion was found to be an independent favorable prognostic factor, while the high level of CA19-9 resulted an independent unfavorable prognostic factor. Conclusion: High values of CA19-9 at the beginning of the first-line chemotherapy represent an independent prognostic factor, therefore it should be taken into consideration to select the treatment. Surprisingly the presence of invasion appeared as an independent favorable prognostic factor in locally advanced and metastatic pancreatic cancer and this result may impact therapy decisions and stratification of future clinical trials.
Keywords
Lymphatic invasion; Vascular invasion; Perineural invasion; CA19-9; Pancreatic cancer
Introduction
Pancreatic cancer is the fourth and fifth leading cause of cancerrelated death in the United States and Japan, respectively [1,2]. Because of its aggressive growth and early metastatic dissemination, the overall 5-year survival rate for patients with pancreatic cancer remains poor (3-5%) [3]. The mortality rate has not shown any significant improvement for decades. In the light of such poor results, data regarding factors which may influence outcome, are essential also in order to optimize the treatment options for pancreatic cancer patients. Previous studies confirmed that subjects, who show a significant increase of CA19- 9 at the time of diagnosis or onset of chemotherapy, present a worse survival if compared to those in which the marker is within normal range. Furthermore, seriate analyses of CA19-9 during chemotherapy represent useful and specific markers of response to the treatment itself. In fact, some studies showed that a reduction of CA19-9 values by more than 20% from baseline levels (or 50% in some series), during gemcitabine-based chemotherapy (after 6-8 weeks of treatment), is a predictor of response as well as a favorable prognostic factor [4-7]. Another relevant prognostic parameter is the presence of perineural, vascular and lymphatic invasion since angiogenesis and vascular invasion are essential characteristics for tumor growth and dissemination. In general, micro-invasion of perineural and vascular tissues reflects an aggressive cancer phenotype. Perineural invasion, in particular, is considered associated with local recurrence in resected pancreatic cancer and with increasing de-differentiation of pancreatic tumours [8]. Pancreatic tissue itself hosts a large number of neural tissue and ganglia and is in close physical approximation to neural plexi in the retroperitoneum. Therefore perineural infiltration potentially accounts for the main mechanism by which pancreatic cancers infiltrate the retroperitoneum. Several studies examined the impact of perineural invasion on survival in resected pancreatic adenocarcinoma, reporting infiltration as a significant prognostic variable. In fact perineural invasion was associated with poor survival following pancreaticduodenectomy [9-13]. Again, several studies showed that blood vessel invasion was associated with poor outcome in patients with resected pancreatic cancer [11,14,15].
The purpose of our study was to investigate the prognostic role of CA19-9 at the beginning of the first-line chemotherapy as well as the prognostic role of perineural, vascular and lymphatic invasion in a large monocentric series of patients with locally advanced unresectable or metastatic pancreatic cancer, with the aim to serve as a tool for a more accurate and rational treatment selection.
Patients and Methods
Patients selection
The study included 181 patients with a histological or clinical diagnosis of ductal pancreatic cancer who received chemotherapy at the Department of Medical Oncology of Polytechnic University of Marche Region from January 2000 to August 2010 and who was then followed on a regular basis in a specific follow-up program. Recorded patient characteristics and clinical features included: age, sex, weight, risk factors, symptoms, Eastern Cooperative Oncology Group (ECOG) performance status, type of surgery (when performed), histological type, grading, pathological stage of disease (T, N, M), site of disease within the pancreas, pathological features (tumor necrosis, presence of intra-tumoral vascular and neural invasion), value of tumor markers (CA19-9 and CEA), blood tests, dates of chemotherapy, response to chemotherapy and clinical benefit, overall survival (OS) and progression free survival (PFS).
Chemotherapy treatment
Adjuvant chemotherapy with gemcitabine in monotherapy was prescribed, when indicated according to guidelines.
Chemotherapy for locally advanced or metastatic disease included gemcitabine-based regimens (in monotherapy or in combination with cisplatin or oxaliplatin). Second-and third-line regimens included Fluoropyrimidines in combination with irinotecan or mytomicin-C. Toxicity due to chemotherapy was evaluated according to the NCI-CTC (National Cancer Institute - Common Toxicity Criteria), 3.0 version. Objective responses to chemotherapy were evaluated according to the RECIST (Response Evaluation Criteria in Solid Tumors) Criteria, 1.0 version [16]. Clinical progression of disease included occurrence of ascites, worsening of clinical conditions, and significant increase of CA19-9.
Pathologic findings
All the patients underwent biopsies for diagnostic purposes. Pathologic specimens deriving from biopsies were formalin fixed. For each case an adequate tumor sampling was performed and tissue samples were paraffin embedded. From each paraffin block, a 5-μm section was cut and stained with H&E. Histological tumor typing and grading was performed according to the principles of the WHO.
For each case, two expert Pathologists (I.B. and A.M.) evaluated the slides with a double-blind method. The histological examination reported: the total number of lymph node, the number of metastatic nodes and any peri-nodal, vascular and neural invasion.
Statistical analysis
The primary endpoint of this study was to evaluate the prognostic role of clinical and biological factors in patients with advanced pancreatic cancer. OS was defined as the interval between the first day of chemotherapy to death or last follow-up visit. Patients who were not reported to be deceased at the time of the analysis were censored at the date they were last known to be alive.
The PFS for each line of chemotherapy was calculated from the start of chemotherapy until the date of progression, or death from any cause or last follow-up in patients who did not progressed. We compared OS among subgroups of patients according to the levels of CA19-9 and to the presence of vascular, neural and lymphatic invasion. The association between categorical variables was estimated by Chi-square test. The Cox multivariate proportional hazard regression model was used to evaluate the effects of the prognostic factors on survival. Survival distribution was estimated by the Kaplan-Meier method. Significant differences in probability of surviving between the strata were evaluated by log-rank test. Hazard ratios and 95% confidence intervals were estimated from regression coefficients. A significant level of 0.05 was chosen to assess the statistical significance. Statistical analysis was performed with MedCalc package (MedCalc® v9.4.2.0).
Results
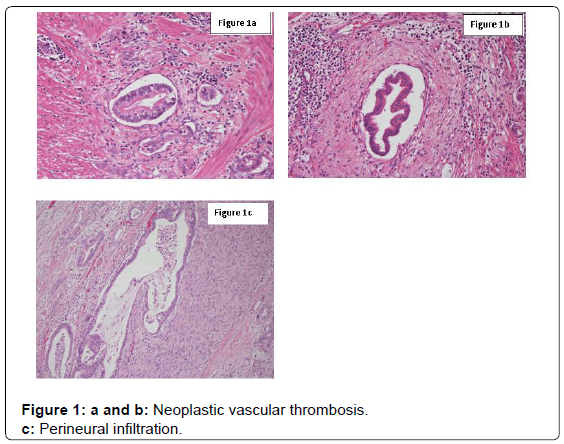
One hundred and eighty-one consecutive patients with locally advanced or metastatic pancreatic cancer were enrolled into this study. Tables 1 and 2 summarize patients’ clinical and pathological characteristics. In 13 tumor samples (7.2%), perineural infiltration was present, while in 11 (6.1%) and in 6 (3.3%) cases vascular and lymphatic infiltration were present, respectively (Figures 1a-1c).
| Patients’ characteristics | Number of patients (%) (Total=181) |
|---|---|
| Sex Male Female |
102 (56,3%) 79 (43,7%) |
| Age Median (Range) |
65 years (38-84) |
| Stage of cancer at first presentation I II III IV Locally advanced vs metastatic at study enrollment |
6 (3,3%) 22 (12,2%) 55 (30,4%) 98 (54,1%) 146/181 (80,7%/19.3%) |
| Site of metastases Liver Lung Peritoneum Loco-regional Other |
66 (67,3%) 4 (4,1%) 12 (12,2%) 13 (3,1%) 3 (13,3%) |
| Performance Status ECOG 0 1 2 3 |
90 (49,7%) 69 (38,1%) 19 (10,5%) 3 (1,7%) |
| Follow up Median (range) | 8,51 months (0,39-66,1) |
| Deaths Yes No |
147 (81,2%) 34 (18,8%) |
Table 1: Patients’ characteristics.
| Tumor characteristics | Number of pazients (%) (Total=181) |
|---|---|
| Istotype Ductal adenocarcinoma Intraductal papillary adenocarcinoma Cystadenocarcinoma Other |
157 (86,7%) 2 (1,1%) 2 (1,1%) 20 (11%) |
| Invasion Perineural Vascular Lymphatic |
13 (7,2%) 11 (6,1%) 6 (3,3%) |
Table 2: Pathological characteristics of cancer.
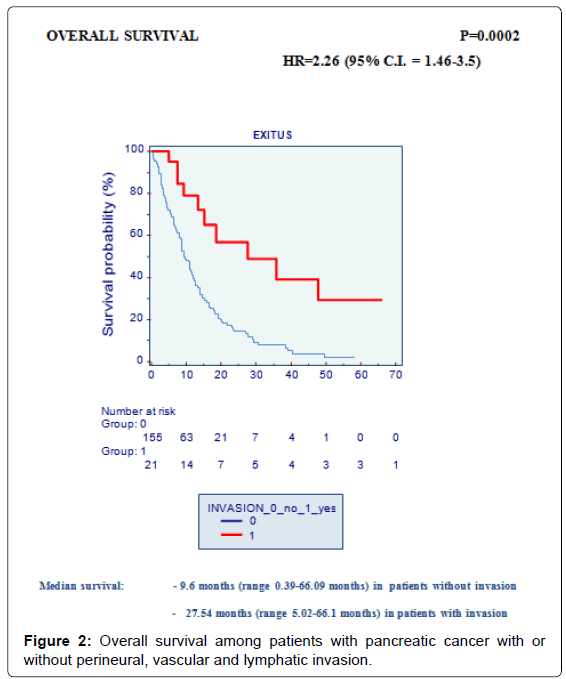
At univariate analysis the three above mentioned factors (perineural, vascular and lymphatic invasion) showed a positive correlation with OS. Surprisingly OS in patients with perineural, vascular and/or lymphatic invasion was significantly increased (p=0.0002). In fact, median OS was 9.6 months (range 0.39 to 66.09 months) in patients without invasion vs. 27.5 months (range 5.02 to 66.1 months) in patients with invasion (Figure 2).
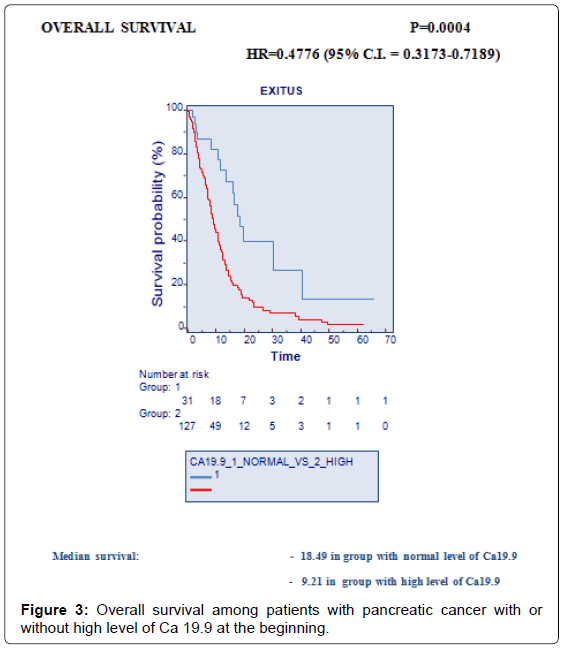
CA19-9 was available for 164 patients: it was above the normal upper limit in 132 patients (72.9%), and it was normal in 32 patients (17.7%). At univariate analysis CA 19-9 was found to be a prognostic factor (≤ 37 U/ml vs. >37 U/ml, median OS=18,49 months vs. 9,21 months, respectively, p=0,0004) (Figure 3).
At multivariate analysis the presence of vascular, lymphatic and perineural invasion surprisingly appeared an independent favorable prognostic factor, while the elevated CA19-9 at onset resulted an independent unfavorable prognostic factor (Table 3).
| Variable | Odds Ratio | 95% CI | p-value |
|---|---|---|---|
| INVASION (absence vs. presence) | 0,2184 | 0,0666 to 0,7166 | 0,01209 |
| Mucinous histotype (absence vs. presence) | 0.9462 | 0,3127 to 2,0954 | 0,9867 |
| SEX | 1,9642 | 0,7932 to 4,8638 | 0,1445 |
| AGE (≤ 65 vs. >65 years) | 0,6422 | 0,2637 to 1,5638 | 0,3294 |
| CA19.9 (normal vs. high) | 5,7195 | 2,2457 to 14,5670 | 0,0002562 |
| CEA (normal vs. high) | 1,2526 | 0,4556 to 3,4441 | 0,6625 |
Table 3: Hazard ratios (H.R.) and 95% confidence limits of the variables included in the multivariate analysis.
Discussion
In patients with locally advanced or metastatic pancreatic cancer several prognostic factors can be detected: local vs. metastatic stage of disease, tumor necrosis [17,18], grading [19], CA19.9, CEA [20], age [21], ECOG [4]. In the present analysis, we found a statistically significant difference in OS between pancreatic cancer patients presenting perineural, vascular and lymphatic infiltration when compared with patients with no perineural, vascular and lymphatic invasion. Furthermore we analyzed the prognostic impact of a high value of CA19.9 vs. a normal value at the beginning of the first-line chemotherapy. In particular, perineural, vascular and lymphatic invasion, was found to be an independent prognostic factor positively correlated with prognosis. In fact, OS was significantly increased if compared to the group of patients in whom no invasion was detected (median survival=27.5 vs. 9.6 months, p=0.0002). This finding is in contrast to what has been previously reported in the literature in resected patients. The study of Nitecki et al. reported a most favorable 5-year survival rate in the subset of patients with negative nodes and no duodenal or perineural invasion [22]. This was confirmed by the study of Ozaki et al. on 193 patients who underwent curative resection of pancreatic cancer; in fact, in the group of patients without nodal metastasis, the 5-year survival rate for those without perineural invasion was 75% versus only 29% for those with perineural invasion. Again, in the group of patients with nodal metastasis, the 5-year survival rate for those without perineural invasion was 17%, and that for those with perineural invasion was 10% [12]. Furthermore in the study of Meyer et al., the perineural invasion contributes to a poor long-term survival [11]. Recently, Badger et al., in 126 surgically resected pancreatic cancer patients, showed that lymphatic vascular and perineural invasion, together with the grading, are important predictors of outcome and their presence is associated with a reduced survival [23]. In particular, perineural invasion has a crucial role in the local recurrence of disease after surgery. Perineural space is known to be an important route of pancreatic cancer invasion. Pancreatic cancer cells invade the neural plexus distributed in pancreatic parenchyma and spread through perineural space to reach extra-pancreatic nerves, such as the celiac plexus or the supra-mesenteric artery plexus. Cancer cell invasion into the neural plexus often results in non-curative resection and, therefore, retroperitoneal recurrence. According to another theory, however, the neural invasion of pancreatic cancer is related to the concept of pancreatic cancer “neurotropism”. This concept was developed by Kenmotsu et al., who reported that advanced pancreatic cancer with neural invasion expressed numerous types of neuroendocrine markers, including S-100, Synaptophysin, Substance-P, Enkephalin, and NCAM [24-26].
Hirai et al. showed that perineural invasion is greater if the cancer becomes less differentiated and if there is a large accumulation of interstitial connective tissue. Although perineural invasion by the glandular structures is often continuous, sometimes the progression may be discontinuous. Thus, even if the margin of surgical resection is free of disease, tumor cells may have already reached distant locations. For that reason additional precautions are recommended, such as the removal of retroperitoneal and peri-pancreatic tissue [8]. This approach is also justified by the study of Mitsunaga et al., who observed that 20-40% of surgeries for apparently resectable pancreatic cancer are really non-curative, because of perineural infiltration already present at the resection margins. Furthermore a study performed by Mitsunaga et al., showed that the nerve plexus invasion and the infiltration of lymphatic vessels are important prognostic and predictive factors. These parameters seem to be more significant than the presence of intrapancreatic nerve invasion or lymph node metastases. Then, this study showed that a long distance between the invasion of pancreatic nerve plexus and pancreatic margin is an important prognostic factor in patients with pancreatic adenocarcinoma: in fact a distance greater than 2500 μm between the two structures is significantly associated with poor survival [27,28]. A systematic review evaluating the impact of vascular invasion and perineural infiltration on median survival performed by Garcea et al. showed that in tumors with vs. without perineural infiltration the median survival was respectively of 16 months vs. 18.4 months and in tumors with vs. without vascular invasion the median survival was respectively of 11.9 months vs. 20.6 months. It was also evident that, although vascular invasion is less frequent than perineural infiltration, it has a more severe impact on survival. This is due to the fact that vascular invasion is responsible of metastatic recurrence of disease and thus related to a greater impact on survival, while the nerve invasion is responsible of local recurrence of disease which is not directly related to patient death [29]. It is important to notice that all the above mentioned studies evaluated perineural, vascular and lymphatic invasion in groups of patients who underwent surgery for pancreatic cancer, thus analyzing the impact on recurrence of disease and on survival. In this context, vascular, perineural and lymphatic invasion resulted as unfavorable factor and this may represent an expression of biological malignancy of the disease. Our study, instead, evaluated the same parameters in patients with advanced pancreatic cancer (unresectable or metastatic cancer) and it represents the first experience in this setting in a large monocentric series. In our opinion, the different results found in the localized and in the advanced setting, could be explained by the fact that in advanced pancreatic cancer, the presence of histological parameters known to be expression of malignancy of the tumor, may result in a better response to antiblastic treatments, causing an improvement of prognosis in the subgroup of patients presenting these features. This result implies some considerations: in patients with advanced pancreatic cancer the use of an aggressive chemotherapy (i.e. FOLFIRINOX or a combination of several chemotherapeutic drugs), may be preferable. Furthermore, a treatment with a single agent (i.e. gemcitabine) is not absolutely recommended and this approach should be adopted even in patients who appear to have better prognosis. In addition, in the advanced setting, vascular invasion seems to be a favorable factor because it allows to select tumors that have a rich angiogenesis with a different prognosis in respect to pancreatic tumors with extensive desmoplastic reaction. With the advances in molecular biology, newer biologic agents such as bevacizumab and sorafenib are adding some benefit to the conventional cytotoxic agents. Unfortunately, these agents have failed to report a significant improvement in overall survival in patients [30-33]; probably because there was not a previous selection of patients which expressed specific histological characteristics of invasion. Focusing on the clinical and biochemical parameters, this study also confirmed the prognostic role of CA19-9: the group of patients with elevated levels of CA 19-9 at onset, in fact, presented a significantly reduced survival if compared to the others (9.2 vs. 18.5 months, p=0.0004). Thus, CA19-9 may be an additional parameter in order to select the most appropriate treatment, suggesting the use of combination chemotherapy when CA19-9 is high at the beginning, according to what has been previously published in the literature. In fact, previous studies showed that subjects who present a significant increase of CA19-9 at the time of diagnosis or onset of chemotherapy, have a reduced survival compared to those in which the marker is normal [5].
A recent study of Kang et al. on 102 patients shows that pre-operative CA19-9 is also useful for estimating the risk of recurrence in patients undergoing surgical resection for pancreatic cancer as well as for the choice of therapeutic strategies. Nevertheless, further prospective studies are needed to evaluate the outcomes of these strategies based on the values of CA19-9 [34].
In conclusion, the results of our study, on a large series of patients with locally advanced unresectable pancreatic cancer or metastatic pancreatic cancer, suggest the importance of a few parameters: perineural, vascular and lymphatic invasion and CA19-9. Although the relatively small sample size of the group of patients with pathologically detected perineural, vascular and lymphatic invasion, the role of these parameters (which are commonly available) may be relevant in the clinical practice in order to identify subgroups of patients with unfavorable or favorable prognosis before the first-line chemotherapy treatment and then to guide treatment choices. In patients with invasive and stage III-IV pancreatic cancer, the use of a more aggressive chemotherapy, which is based on the scheme FOLFIRINOX or on the combination of several chemotherapeutic drugs, should be preferred when histological examinations reveal the presence of perineural, vascular and lymphatic invasion. At the same time any possibility of treatment with a single agent such as gemcitabine should be excluded. Prognosis for locally advanced or metastatic pancreatic cancer is still poor nowadays and despite the interesting advance provided by combinations, survival results remain disappointing. Further research focused on new combinations, incorporating the new targeted therapies and identifying potential predictive factors of response, also confirming the ones analyzed in the present study, are required to be able to offer effective tailored therapies to our patients.
Acknowledgements
Source of support: The study was supported by authors’ University Fundings (Università Politecnica Marche).
References
- Siegel R, Naishadham D, Jemal A (2013) Cancer statistics, 2013. CA Cancer J Clin 63: 11-30.
- Center for Cancer Control and Information Services, National Cancer Center Japan, Cancer statistics in Japan.
- Hruban RH, Pitman MB, Klimstra DS (2007) Ductal adenocarcinoma. In: AFIP Atlas of Tumor Pathology. Tumor of the pancreas (4thedn) ARP Press: Washington, DC.
- Boeck S, Hinke A, Wilkowski R, Heinemann V (2007) Importance of performance status for treatment outcome in advanced pancreatic cancer. World J Gastroenterol 13: 224-227.
- Maisey NR, Norman AR, Hill A, Massey A, Oates J, et al. (2005) CA19-9 as a prognostic factor in inoperable pancreatic cancer: the implication for clinical trials. Br J Cancer 93: 740-743.
- Saad ED, Machado MC, Wajsbrot D, Abramoff R, Hoff PM, et al. (2002) Pretreatment CA 19-9 level as a prognostic factor in patients with advanced pancreatic cancer treated with gemcitabine. Int J Gastrointest Cancer 32: 35-41.
- Halm U, Schumann T, Schiefke I, Witzigmann H, Mössner J, et al. (2000) Decrease of CA 19-9 during chemotherapy with gemcitabine predicts survival time in patients with advanced pancreatic cancer. Br J Cancer 82: 1013-1016.
- Hirai I, Kimura W, Ozawa K, Kudo S, Suto K, et al. (2002) Perineural invasion in pancreatic cancer. Pancreas 24: 15-25.
- Shimada K, Sakamoto Y, Sano T, Kosuge T (2006) Prognostic factors after distal pancreatectomy with extended lymphadenectomy for invasive pancreatic adenocarcinoma of the body and tail. Surgery 139: 288-295.
- Bouvet M, Gamagami RA, Gilpin EA, Romeo O, Sasson A, et al. (2000) Factors influencing survival after resection for periampullary neoplasms. Am J Surg 180: 13-17.
- Meyer W, Jurowich C, Reichel M, Steinhäuser B, Wünsch PH, et al. (2000) Pathomorphological and histological prognostic factors in curatively resected ductal adenocarcinoma of the pancreas. Surg Today 30: 582-587.
- Ozaki H, Hiraoka T, Mizumoto R, Matsuno S, Matsumoto Y, et al. (1999) The prognostic significance of lymph node metastasis and intrapancreatic perineural invasion in pancreatic cancer after curative resection. Surg Today 29: 16-22.
- Takahashi T, Niino N, Ishikura H, Okushiba S, Dohke M, et al. (1997) Predictive factors for long-term survival in patients with pancreatic carcinoma. Hepatogastroenterology 44: 1463-1468.
- Sierzega M, Popiela T, Kulig J, Nowak K (2006) The ratio of metastatic/resected lymph nodes is an independent prognostic factor in patients with node-positive pancreatic head cancer. Pancreas 33: 240-245.
- Kedra B, Popiela T, Sierzega M, Precht A (2001) Prognostic factors of long-term survival after resective procedures for pancreatic cancer. Hepatogastroenterology 48: 1762-1766.
- Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, et al. (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92: 205-216.
- Bristow RG, Hill RP (2008) Hypoxia and metabolism. Hypoxia, DNA repair and genetic instability. Nat Rev Cancer 8: 180-192.
- Couvelard A, O'Toole D, Leek R, Turley H, Sauvanet A, et al. (2005) Expression of hypoxia-inducible factors is correlated with the presence of a fibrotic focus and angiogenesis in pancreatic ductal adenocarcinomas. Histopathology 46: 668-676.
- Lüttges J, Schemm S, Vogel I, Hedderich J, Kremer B, et al. (2000) The grade of pancreatic ductal carcinoma is an independent prognostic factor and is superior to the immunohistochemical assessment of proliferation. J Pathol 191: 154-161.
- Blumenthal RD, Hansen HJ, Goldenberg DM (2005) Inhibition of adhesion, invasion, and metastasis by antibodies targeting CEACAM6 (NCA-90) and CEACAM5 (Carcinoembryonic Antigen). Cancer Res 65: 8809-8817.
- Zhang Y, Dang C, Ma Q, Chen W, Nagata K (2007) Predictors of systemic chemotherapy contraindication in pancreatic cancer patients with distant metastasis. Hepatogastroenterology 54: 254-259.
- Nitecki SS, Sarr MG, Colby TV, van Heerden JA (1995) Long-term survival after resection for ductal adenocarcinoma of the pancreas. Is it really improving? Ann Surg 221: 59-66.
- Badger SA, Brant JL, Jones C, McClements J, Loughrey MB, et al. (2010) The role of surgery for pancreatic cancer: a 12-year review of patient outcome. Ulster Med J 79: 70-75.
- M. Kenmotsu (1990) Relationship Between Perineural Invasion and Expression of Neuro-endocrine Markers and Neural Cell Adhesion Molecule in Human Pancreatic Carcinoma. The Japanese Journal of Gastroenterological Surgery 23: 2580-2585.
- Nagai H, Kuroda A, Morioka Y (1986) Lymphatic and local spread of T1 and T2 pancreatic cancer. A study of autopsy material. Ann Surg 204: 65-71.
- Kameda K, Shimada H, Ishikawa T, Takimoto A, Momiyama N, et al. (1999) Expression of highly polysialylated neural cell adhesion molecule in pancreatic cancer neural invasive lesion. Cancer Lett 137: 201-207.
- Mitsunaga S, Hasebe T, Iwasaki M, Kinoshita T, Ochiai A, et al. (2005) Important prognostic histological parameters for patients with invasive ductal carcinoma of the pancreas. Cancer Sci 96: 858-865.
- Mitsunaga S, Hasebe T, Kinoshita T, Konishi M, Takahashi S, et al. (2007) Detail histologic analysis of nerve plexus invasion in invasive ductal carcinoma of the pancreas and its prognostic impact. Am J Surg Pathol 31: 1636-1644.
- Garcea G, Dennison AR, Pattenden CJ, Neal CP, Sutton CD, et al. (2008) Survival following curative resection for pancreatic ductal adenocarcinoma. A systematic review of the literature. JOP 9: 99-132.
- Rivera F, López-Tarruella S, Vega-Villegas ME, Salcedo M (2009) Treatment of advanced pancreatic cancer: from gemcitabine single agent to combinations and targeted therapy. Cancer Treat Rev 35: 335-339.
- Chames P, Kerfelec B, Baty D (2010) Therapeutic antibodies for the treatment of pancreatic cancer. ScientificWorldJournal 10: 1107-1120.
- Stathis A, Moore MJ (2010) Advanced pancreatic carcinoma: current treatment and future challenges. Nat Rev Clin Oncol 7: 163-172.
- Starling N, Watkins D, Cunningham D, Thomas J, Webb J, et al. (2009) Dose finding and early efficacy study of gemcitabine plus capecitabine in combination with bevacizumab plus erlotinib in advanced pancreatic cancer. J Clin Oncol 27: 5499-5505.
- Kang CM, Kim JY, Choi GH, Kim KS, Choi JS, et al. (2007) The use of adjusted preoperative CA 19-9 to predict the recurrence of resectable pancreatic cancer. J Surg Res 140: 31-35.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 16581
- [From(publication date):
October-2013 - Nov 19, 2025] - Breakdown by view type
- HTML page views : 11703
- PDF downloads : 4878