Case Report Open Access
Shortness of Breath: Anyone Consider the Gut?
Ayesha Kanwal1*, Imran Sheikh1, Raja R Shekhar Sappati Biyyani2, Corey Sievers2 and Annette Kyprianou21Division of Hospital Medicine, MetroHealth Medical Center, Case Western Reserve University, Cleveland, Ohio 44109, USA
2Division of Gastroenterology, MetroHealth Medical Center, Case Western Reserve University, Cleveland, Ohio 44109, USA
- *Corresponding Author:
- Ayesha Kanwal DO
Division of Hospital Medicine
MetroHealth Medical Center
Case Western Reserve University
Cleveland, Ohio 44109, USA
Tel: 817 703 8671
E-mail: ayeshakw@hotmail.com
Received date: October 17, 2011; Accepted date: June 25, 2012; Published date: June 28, 2012
Citation: Kanwal A, Sheikh I, Sappati Biyyani RRS, Sievers C, Kyprianou A (2012) Shortness of Breath: Anyone Consider the Gut?. J Gastroint Dig Syst 2:115. doi: 10.4172/2161-069X.1000115
Copyright: © 2012 Kanwal A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Dyspnea is a common complaint that compels patients to seek medical care. Usual etiologies include asthma, chronic obstructive pulmonary disease, myocardial dysfunction and pulmonary embolus. In our case a patient was admitted to our hospital with dyspnea, fatigue and pleuritic chest pain for three weeks. Physical examination and imaging were unremarkable. Labs were only significant for severe microcytic anemia with hemoglobin 2.8 g/dL, hematocrit of 12%, MCV 56, iron <6 mcg/dL, and ferritin 13.9 ng/mL. All the usual causes of iron deficiency anemia were ruled out and patient was diagnosed with celiac disease. The incidence of celiac disease in patients with iron deficiency anemia has been reported to be from 6% to 12%. Among patients whose anemia does not respond to iron therapy the incidence increases to 20%. This case illustrates that when a patient with common complaints of dyspnea and anemia is evaluated celiac disease should always be considered in the differential.
Keywords
Celiac disease; Anemia; Iron deficiency anemia; Dyspnea; Myocardial dysfunction
Introduction
Dyspnea is a very common complaint for which patients seek medical care. In majority of the patients their dyspnea can be attributed to one of the following causes asthma, pneumonia, chronic obstructive pulmonary disease, myocardial dysfunction, pulmonary embolus and deconditioning [1]. Our case here presents an etiology representing a subtle cause of myocardial dysfunction.
Case Presentation
A 39 year old Caucasian male with no past medical history was admitted to an inpatient service for the complaint of dyspnea on exertion and fatigue for three weeks. His exertional capacity had progressively declined from 1000ft to 100ft. He also reported pleuritic chest pain and a dry cough. He denied fevers, chills, hemoptysis, hematemesis, melena, hematuria, hematochezia, decreased appetite, dysphagia, abdominal pain, diarrhea and PICA. He admitted to consuming a balanced diet and denied a surgical or traumatic history, foreign family heritage or history of blood disorders.
His vitals were normal and his examination only remarkable for pallor and cafe au lait macules over his back since birth. Labs revealed severe microcytic anemia, hemoglobin 2.8 g/dL, Hematocrit 12%, MCV 56, iron <6 mcg/dL, TIBC 473 mcg/dL, ferritin 13.9 ng/ mL. Reticulocyte count was 2%, stool for occult blood was negative. LDH, haptoglobin, TSH, folate, vitamin B12, HIV, Parvovirus B19 panel and hemoglobin electrophoresis were all within normal limits.
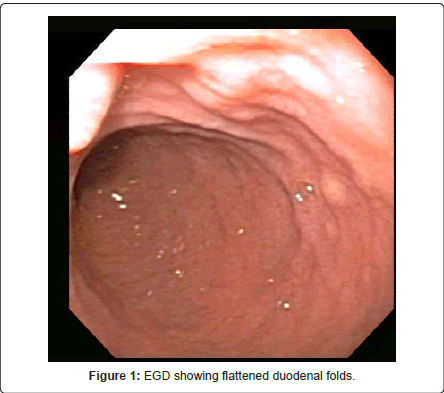
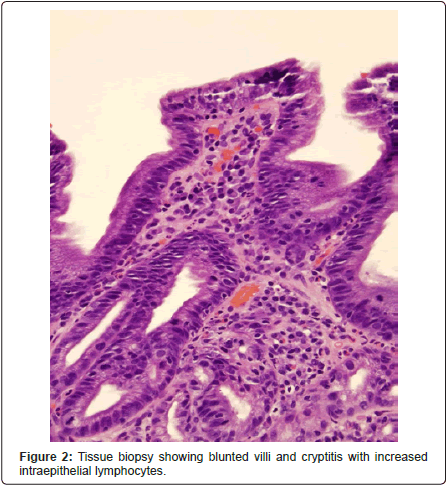
A celiac antibody panel performed to further evaluate the showed 124 Transglutaminase IgA Abs, 46 Gliadin IgG Abs, >30 Gliadin IgA Abs, Quantitative IgA 344 mg/dL, 9 Transglutaminase IgG Abs. Levels of >30 are positive and suggest celiac disease. An EGD showed flattening of duodenal folds and distal esophagitis. Random biopsies were consistent with celiac disease (Figure 1, Figure 2).
Discussion
The fundamental factor in determining this patient’s cause of dyspnea is severe iron deficiency, which in the USA is mostly secondary to occult blood loss [2]. But more and more studies now are pointing towards celiac disease as a frequent cause of iron deficiency. One study reports that 12% of 93 patients with iron deficiency anemia had findings compatible with celiac disease on small bowel biopsy [3]. Another study reports the incidence as 6% (85 patients) and the incidence increases to 20% in the subset of anemic patients that are unresponsive to iron therapy [4]. It remains unclear whether a component of blood loss contributes to iron deficiency in celiac disease [5-7].
The diagnosis of celiac disease often requires serological testing and small bowel biopsy, both of which are recommended while patients are on a gluten-containing diet [5]. The exception to a small bowel biopsy is biopsy-proven dermatitis herpetiformis [6]. A positive IgA tissue transglutaminase or endomysial antibody test is considered highly specific, whereas standard antigliadin antibody tests have lower diagnostic accuracy and are falsely positive up to 20% of the time [5]. The hallmark histology of small bowel biopsy is the presence of villous atrophy. Several biopsies in the second and third portion of the duodenum should be obtained to maximize the likelihood of detecting villous atrophy [7].
As our case illustrates the differential for SOB is not just limited to pulmonary and cardiac disease processes but gastrointestinal diseases as well. Celiac disease should now be considered in all patients with iron deficiency anemia and may help us identify this disease process earlier on.
References
- Pratter MR, Curley FJ, Dubois J, Irwin RS (1989) Cause and evaluation of chronic dyspnea in a pulmonary disease clinic. Arch Intern Med 149: 2277-2282.
- Cook JD, Skikne BS (1989) Iron Deficiency: definition and diagnoses. J Intern Med 226: 349-355.
- Ackerman Z, Eliakim R, Stalnikowica R, Rachmilewitz D (1996) Role of small bowel biopsy in the endoscopic evaluation of adults with iron deficiency anemia. Am J Gastroenterol 91: 2099-2102.
- Carroccio A, Iannitto E, Cavataio F, Montalto G, Tumminello M, et al. (1998) Sideropenic anemia and celiac disease: one study, two points of view. Dig Dis Sci 43: 673-678.
- Harper JW, Holleran SF, Ramakrishnan R, Bhagat G, Green PH (2007) Anemia in celiac disease is multifactorial in etiology. Am J Hematol 82: 996-1000.
- Fine KD (1996) The prevalence of occult gastrointestinal bleeding in celiac sprue. N Engl J Med 334: 1163-1167.
- Logan RF, Howarth GF, West J, Shepherd K, Robinson MH, et al. (2003) How often is a positive faecal occult blood test the result of coeliac disease? Eur J Gastroenterol Hepatol 15: 1097-1100.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 21933
- [From(publication date):
August-2012 - Dec 22, 2025] - Breakdown by view type
- HTML page views : 17113
- PDF downloads : 4820