Letter to Editor Open Access
Isolated Hepatic Recurrence of Pre-B Cell ALL Masquerading as Veno- Occlusive Liver Disease
Russell P. Gollard*
Cancer & Blood Specialists of Nevada, 58 N. Pecos Road, Henderson, NV 89074, USA
- *Corresponding Author:
- Russell P. Gollard, MD
FACP, Cancer & Blood Specialists of Nevada
58 N. Pecos Road, Henderson
NV 89074, USA
Tel: 702 822 2000
E-mail: rgollard@hotmail.com
Received date: September 09, 2011; Accepted date: November 15, 2011; Published date: November 17, 2011
Citation: Gollard RP (2011) Isolated Hepatic Recurrence of Pre-B Cell ALL Masquerading as Veno-Occlusive Liver Disease. J Gastrointest Dig Syst 1:103. doi:10.4172/2161-069X.1000103
Copyright: © 2011 Gollard RP. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
We report a 47-year-old male with relapsed B-cell ALL in his liver, who initially appeared to have hepatic veno-occlusive disease (now known as sinusoidal obstructive syndrome, SOS) of the liver.
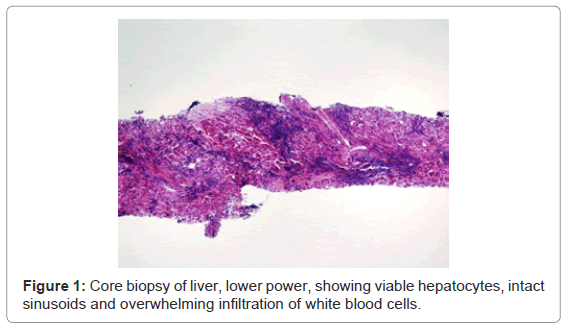
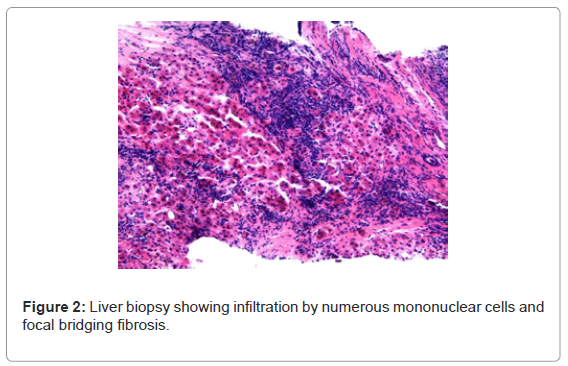
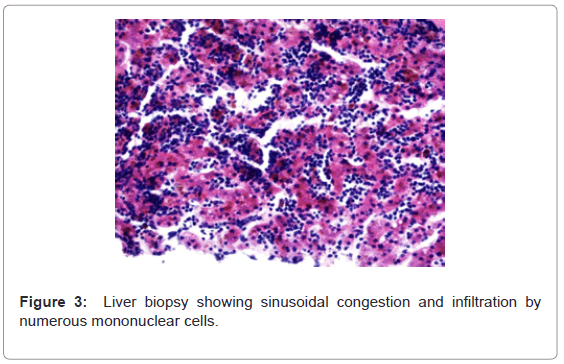
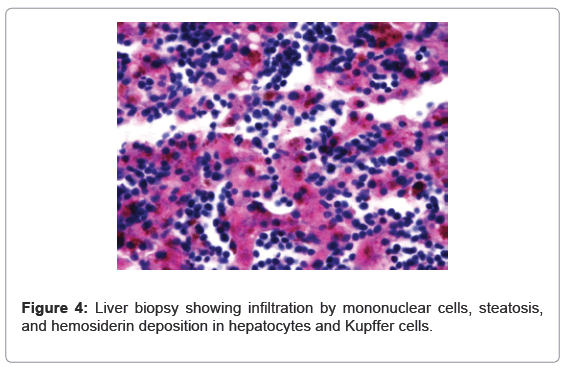
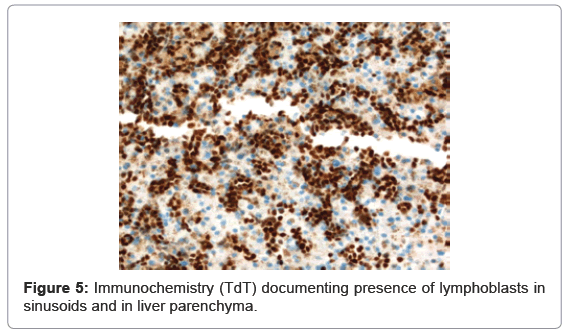
He was diagnosed with pre B-cell ALL. The blasts expressed CD19, CD20, HLADR, CD10, CD34 and intracellular TDT. The patient was treated with hyper CVAD parts A and B for eight cycles, along with intrathecal methotrexate as prophylaxis [1]. At presentation, the patient also had an LDH level of greater than 1200. The patient immediately went into a full remission. He continued to be in remission throughout eight cycles of hyper CVAD but then relapsed two months after his eighth and final cycle. He was then treated on the Larson regimen in preparation for a transplant [2]. Specifically, the patient received reinduction with an asparaginase containing regimen, which also included daunorubicin, vincristine and prednisone. The patient, on day 15 of the cycle, started to develop hyperbilirubinemia as well as swelling in his abdomen; he later developed massive and refractory ascites. There was no portal vein, hepatic vein or inferior cava thrombosis. He had no hepatosplenomegaly at the time of relapse. He was also pancytopenic. He was treated with supportive care, which included hydration, diuretics and transfusions. He received more than 20 paracenteses, and his total bilirubin rose to over 35. With supportive care, the patient’s bilirubin gradually declined to normal levels. Neither the ALT nor the AST nor the alkaline phosphatase was more than twice the upper limit of normal. The patient had bone marrow aspirate and biopsies completed; these were all negative. Combinations of spironolactone and furosemide did not adequately mobilize the patient’s ascites. Finally, the patient underwent a transjugular biopsy of the liver. The patient was found to have involvement of the liver with B-cell ALL (Figure 1-5). There was microvesicular and macrovesicular steatosis, as well as pericellular and focal bridging fibrosis. There was hemosiderin deposition within the hepatocytes and Kupffer cells. The patient subsequently went to inpatient hospice and died of fulminant hepatic failure within 24 hours.
Veno-occlusive disease of the liver is oftentimes a diagnosis of exclusion [3]. Onset usually occurs when a patient is pancytopenic, and hence biopsies are not often performed. Rather, there is often strong clinical suspicion with weight gain, hepatosplenomegaly, and ascites. Usually there is a discordant rise in indirect and total bilirubin levels with a relative leveling of elevated transaminase (ALT and AST) and alkaline phosphatase. Elevated alkaline phosphatase can indicate steatosis or infiltrative liver disease, whereas transmaninitis can be a manifestation of hypotensive liver damage. Drug toxicity can be manifested by selective elevation of any of the aforementioned laboratory parameters. Treatment usually consists of transfusion support along with meticulous monitoring of fluid status. Defibrotide, thrombolytic agents, heparin, prostaglandin E1 and antioxidants have all been tried for treatment with varying degrees of success [4,5]. As prophylaxis, heparin, defibrotide, and ursodeoxycholic acid have been studied. SOS is fatal in more than 50% of cases. In this patient’s case, he probably relapsed within a sanctuary site and developed portal hypertension because of the presence of lymphoblasts within the liver. These same lymphoblasts probably caused occlusion of terminal hepatic venules and hepatic sinusoids resulting in SOS. Local effects of immunoblasts within hepatic sinusoids may have mimiced SOS, which is mediated by endothelial cell damage leading to endothelial cell swelling and thrombosis. Isolated relapses of leukemia within the liver should be considered in patients who appear to have VOD. Transjugular biopsies may be accomplished without significant risk of exsanguination when appropriate support with blood products is given.
References
- Kantarjian HM, O'Brien S, Smith TL, Cortes J, Giles FJ, et al. (2000) Results of treatment with hyper-CVAD, a dose-intensive regimen, in adult acute lymphocytic leukemia. J Clin Oncol 18: 547-561.
- Larson RA, Dodge RK, Burns CP, Lee EJ, Stone RM, et al. (1995) A five-drug remission induction regimen with intensive consolidation for adults with acute lymphoblastic leukemia: cancer and leukemia group B study 8811. Blood 85: 2025-2037.
- Cefalo MG, Maurizi P, Arlotta A, Scalzone M, Attinà G, et al. (2010) Hepatic veno-occlusive disease: a chemotherapy-related toxicity in children with malignancies. Paediatr Drugs 12: 277-284.
- Richardson PG, Soiffer RJ, Antin JH, Uno H, Jin Z, et al. (2010) Defibrotide for the treatment of severe hepatic veno-occlusive disease and multiorgan failure after stem cell transplantation: a multicenter, randomized, dose-finding trial. Biol Blood Marrow Transplant 16: 1005-1017.
- Shah MS, Jeevangi NK, Joshi A, Khattry N (2009) Late-onset hepatic venoocclusive disease post autologous peripheral stem cell transplantation successfully treated with oral defibrotide. J Cancer Res Ther 5: 312-314.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14056
- [From(publication date):
December-2011 - Dec 01, 2025] - Breakdown by view type
- HTML page views : 9412
- PDF downloads : 4644