A Comparison Between Oncoplastic Breast Conserving Surgery andStandard Wide Local Excision: A UK Experience
Received: 25-Nov-2015 / Accepted Date: 29-Dec-2015 / Published Date: 31-Dec-2015 DOI: 10.4172/2572-4118.1000102
Abstract
Background: The goal of breast conserving surgery is to achieve complete excision of the tumor with adequate surgical margins, while preserving the natural shape and appearance of the breast. This is a retrospective study which compared operative outcomes in oncoplastic (OPS; n=54) versus standard wide local excision (WLE; n=265) populations. A total of 319 consecutive patients were included in the study. The primary outcomes were the size of the tumor, weight of the specimen and margin clearance. The secondary outcomes were patient satisfaction, local recurrence rates and operative time.
Methods: A retrospective comparison of patients undergoing breast conservation from November 2011 to January 2015 was undertaken. This time period was chosen as oncoplastic breast conservation (OPS) was introduced at our breast unit in 2011. The majority of these latter surgeries involved volume displacement methods. Demographic data was collected. Statistical analysis was performed using SPSS software.
Results: Our results demonstrated that OPS excised significantly larger tumors (p<0.05) of greater weights (p<0.05) with little cosmetic penalty. There was no significant difference in margin clearance (p = 0.10) or the number of patients requiring further surgery in both groups (p=0.254).
Conclusion: OPS provides a better cosmetic and oncological result compared to standard wide local excisions based on the weight and size of the tumor. Margin clearance is comparable in both groups. When breast conserving surgery is recommended, oncoplastic methods provide a better outcome in patients requiring a larger excision and can decrease the mastectomy rate in cases of larger tumors.
Keywords: Breast conserving surgery; Oncoplastic breast surgery; Wide local excision; Breast cancer; Cosmesis
Introduction
In women with early stage unifocal breast cancer, breast conserving surgery followed by radiotherapy is the recommended choice. However, in some women, lesions are difficult to excise without the risk of cosmetic deformity or inadequate margin clearance. These women often present with large tumors in relatively small breasts requiring an excision of approximately 15% to 20% of the breast volume or more than 30% in large breasts. Another factor affecting poor cosmesis after breast conserving surgery is tumors located in aesthetically sensitive areas such as the central, medial, and inferior quadrants [1,2].
In recent years, oncoplastic breast conserving surgery (OPS) has increased in popularity. OPS combines the principles of oncologic and plastic surgery techniques to gain oncologically and aesthetically pleasing results [3]. As these techniques become more accepted there is a demand for surgeons to become familiar with the indications and skills required to make oncoplastic surgery safe and effective [4].
The choice between different oncoplastic techniques are determined mainly by the site of the tumor in the breast, tumor characteristics, extent of resection, breast characteristics (size, shape and glandular density), previous surgery, and the expectations and wishes of the patient [5].
OPS can be classified into two main approaches according to the reconstruction technique used. Volume displacement techniques are applied to correct quadrantectomy defects in medium to large breasts [6]. They are of particular benefit to those patients who present with ptotic dense glandular breasts. The breast glandular tissue is advanced, rotated or transpositioned to fill the defect [7]. Since this may result in a smaller sized breast, contralateral surgery may be required. Conversely, volume replacement techniques, in which tissue from another site is used to fill the defect, are mainly indicated in women with small to medium sized breasts and minimal ptosis. These patients cannot afford to lose volume and do not desire a mastectomy or contralateral surgery [8].
Several different approaches have been described, which vary in their choice of replacement flap. These include myocutaneous, myosubcutaneous and adipose flaps. An example of a myocutaneous flap is the use of the latissimus dorsi (LD) muscle. It is of particular value to replace volume in the superior, lateral and inferior aspects of the breasts. These methods often require a longer operating time [9].
The possible benefits of OPS which have been reported include a wider excision of the tumor to achieve clear margins and improved cosmetic outcomes [10]. Additionally as the procedures are performed in an immediate setting, a reduction in the complications related to adjuvant radiotherapy is avoided [11]. Since OPS reduces the amount of breast tissue, radiotherapy delivery may in fact be simplified [12].
The purpose of this study was to confirm whether our breast unit is achieving similar outcomes in OPS compared to findings in other studies. The primary outcomes were the size of the tumor; weight of the specimen and margin clearance. The secondary outcomes were patient satisfaction, local recurrence rates and operative time which have not been frequently reported in the recent literature.
Patients and Methods
All patients who underwent breast conservation were selected from the operative records dated from November 2011 to January 2015. The ones who were excluded were those undergoing palliative wide local excisions for local control; diagnostic breast biopsies, and mastectomies. Patients were not matched for age. Those who underwent a standard WLE included a total of 265 consecutive patients whilst 54 in number underwent OPS. The symptomatic and screening populations with a diagnosis of invasive cancer or DCIS were included.
All patients were operated on by a team of breast surgeons. Appropriate axillary surgery was carried out at the time of the initial procedure. Intraoperative sentinel lymph node analysis was carried out with PCR analysis. If it was reported as macrometastases, axillary lymph node clearance was performed. Intra-operative radiography of the excised specimens confirmed the presence of the lesion and determined that the lesion was clear of the margins. Final pathology results were discussed at the multi-disciplinary meeting.
Patients who underwent a standard WLE were assessed for their suitability for a satisfactory cosmetic outcome. If the tumor to breast volume ratio was estimated to be below 20% in the upper and lateral aspects of the breast or less than 10% for medial tumors, cosmetic outcome was predicted to not be affected. Therefore, in this procedure, no glandular mobilization was performed. According to the NICE guidelines, our criteria for margin clearance was 1mm for an invasive cancer and 2 mm for DCIS.
Patients selected for OPS were the ones who underwent quadrantectomies or were assessed to have a poor cosmetic outcome from a standard excision point of view. This was particularly relevant if the expected breast volume loss was more than 20%. Another indication was resections of tumors in the central, medial and lower pole. Reduction mammoplasty was considered based on the presence of macromastia or on patient preference. Other surgical procedures included local breast advancement methods such as the tennis racquet mammoplasty, vertical scar techinques, Grisotti technique, and the B-plasty. All the procedures were unilateral except for the reduction mammoplasty.
Demographic data and histology results were recorded, using SPSS software, with 2-sided t-test and chi-squared analysis. Final histology included the tumor size, weight and the margin status. Invasive tumors which had a <1 mm clearance and <2 mm margin for DCIS underwent re-excision based on local and national guidelines. A survey concerning cosmesis was conducted in the group of patients undergoing OPS surgery (n=40). This took place either at their most recent routine clinic follow-up or by telephone. The questions utilized are shown in Table 1 and was retrieved from Chan et al. who had published similar questions in the World Journal of Surgery in 2010 [13]. The latter author and prior to this, Al Ghazal [14] had utilized these questions to determine the patient’s perspective on the cosmetic outcome on breast conservation. The survey was conducted after the patients had completed their adjuvant radiotherapy. Operative times were collected from the theatre logbooks. The start time of the procedure was knife to skin, and the end was taken as the application of the dressing (Table 1).
| A.Are you satisfied with your postoperative appearance? |
| 1.Not satisfied |
| 2.Acceptable |
| 3.Satisfied |
| 4.Extremely satisfied |
| B.Compared to the untreated breast, is there a difference in the treated breast? |
| 1.Seriously distorted |
| 2.Very different |
| 3.Some difference |
| 4.Nearly identical |
| C.If you could choose again, would you consider another type of breast surgery? |
| 1.Yes |
| 2.Not certain |
| 3.No |
| D.Would you consider further surgery on reshaping the treated breast? |
| 1.Yes |
| 2.Not certain |
| 3.No |
Table 1: Patient satisfaction questionnaire.
All patients with invasive breast cancer and high grade DCIS underwent postoperative radiotherapy. Adjuvant chemotherapy and endocrine therapy was individualized according to the local protocol. Patients were followed up every 6 months for 2 years and then annually for a further 3 years. Annual mammograms were planned for up to 5 years.
Results
The procedures employed were the tennis racquet technique for upper outer quadrant tumors (n= 19); vertical scar techniques (n=15), Z-plasty techniques (n=13), Grisotti flaps (n=3), intramammary flaps (n=2), B-plasty (n=1) and reduction mammoplasty (n=1). There was a significant difference in the age of the patients (p=0.0003). Our results showed that OPS favored younger patients. Both groups showed a majority of ductal carcinomas, with lobular following second in the OPS group and DCIS in the WLE group. There was no significant difference between both groups in terms of the type (p value=0.2) and grade of the tumor (Table 2).
| Group 1 WLE n=265 | Group 2 Oncoplastic Surgery n=54 | P value | |
|---|---|---|---|
| Mean patient age (years) | 61 (27-86) | 54 (27-77) | 0.0003 |
| Tumor type | 0.247 | ||
| Ductal | 203 | 43 | |
| Lobular | 22 | 7 | |
| DCIS | 27 | 4 | |
| Other | 13 | 0 | |
| Tumor Grade | 0.067 | ||
| I | 66 | 7 | |
| II | 135 | 29 | |
| III | 57 | 18 |
Table 2: Demographic data from oncoplastic and standard wide local excision groups.
OPS excised a significantly larger tumor size compared to the WLE procedure (p<0.05). Significantly heavier specimens were removed from patients undergoing OPS relative to WLE (P<0.05) which is illustrated in Table 3.
| Group 1 WLE n=265 | Group 2 Oncoplastic Surgery n=54 | P value | |
|---|---|---|---|
| Mean specimen weight (grams) | 73.1 grams | 177 grams | <0.05 |
| Size of tumor (mm) | 18.8mm | 32.1mm | <0.05 |
| Mean margin clearance | 3.5mm | 4.7mm | 0.10 |
| Further surgery | 19 | 8 | 0.09 |
Table 3: Primary outcome results *p= <0.05.
The mean margin clearance for the OPS group was 4.7 mm. As for the WLE group, it was 3.5 mm. There was no statistical difference between the margin clearances of both of the groups (p value=0.10). Of the specimens with involved margins, 14 re-excisions and 5 completion mastectomies were performed in the WLE group. A further two completion mastectomies were due to one patient being identified as later having the BRCA1 mutation and another developing complications related to radiotherapy. In the OPS group there was two wider excisions and six completion mastectomies. Out of the six completion mastectomies in the latter group, three of these patients opted for a reconstruction. Two underwent implant based reconstructions, and one underwent a deep inferior epi gastric flap reconstruction. Margin involvement in the OPS group primarily affected those patients with lobular tumors or DCIS extending over 40 mm in size (n=6), while patients with involved margins in the WLE group had ductal carcinoma or in situ disease (n=8).
In relation to the operative times, those patients who underwent a wide local excision (WLE group) spent a shorter time in theatre compared to those who underwent oncoplastic surgery (OPS). This was 62.1 minutes for the WLE versus 91.4 minutes for the OPS group. The difference in the operative times between the two groups was statistically significant with a p value of less than 0.01.
In the WLE group, there was only one immediate postoperative hematoma which was evacuated surgically. In the OPS group, one patient required a hematoma evacuation and two had delayed wound healing. However there was no significant difference in the overall complication rates between the two groups (p=0.254). Neither was there a delay in adjuvant treatment. Adjuvant radiotherapy was required in all cases not having a completion mastectomy.
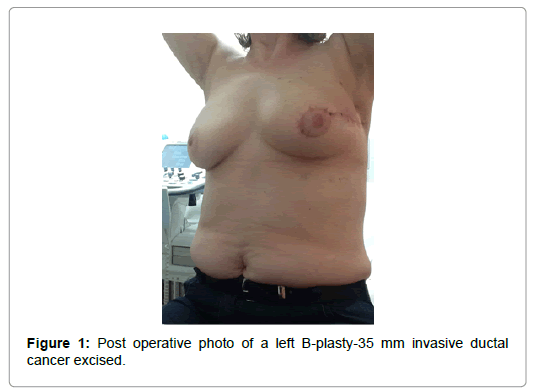
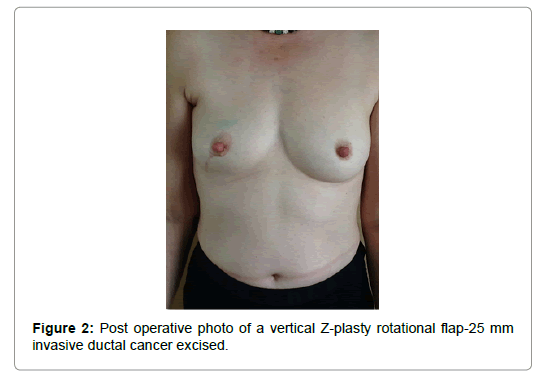
Concerning the cosmetic outcome, the results are illustrated in Table 4. Ninety three percent of the oncoplastic patients were satisfied with their postoperative appearance. Twenty percent of the OPS group felt that the untreated breast was nearly identical. Overall, patients felt that there was only a slight difference. Only one patient in the OPS group considered the operated breast to be seriously distorted. Over 95% of the patients responded that they would not consider another kind of surgery. Finally, over 90% of the patients would not consider further surgery for reshaping the treated breast. Figures 1 and 2 are photos of patients who underwent oncoplastic procedures Table 4.
| Are you satisfied with your postoperative appearance? OPS (n=40) |
| 1.Not satisfied 1 |
| 2.Acceptable 2 |
| Satisfied 37 |
| Extremely satisfied 0 |
| Compared to the untreated breast, is there a difference in the treated breast? |
| Seriously distorted 1 |
| Very different 0 |
| Some difference 31 |
| Nearly identical 8 |
| If you could choose again, would you consider another type of breast surgery? |
| Yes 1 |
| Not certain 1 |
| No 38 |
| Would you consider further surgery on reshaping the treated breast? |
| Yes 1 |
| Not certain 0 |
| No 39 |
Table 4: Results of the patient satisfaction.
The mean length of follow up for the WLE group was 21 months and 17 months for the OPS group. In the WLE group, there was 4 local recurrences. One patient developed recurrent DCIS in another quadrant of the breast. The other patient presented with a recurrent grade 3 infiltrating ductal cancer with her risk factor being heavy nodal disease at her initial surgery. The last two patients who recurred had tumors which were over 4 centimeters in size at initial presentation. Four patients died of metastatic disease during the follow up period. As for the OPS group, out of the 54 patients, one patient developed a local recurrence of the same grade 3 invasive ductal cancer during her adjuvant chemotherapy. Her initial histology had reported a grade 3 triple negative invasive ductal carcinoma measuring 47 mm in diameter. The margin clearance was over 5 mm. Two patients died of metastatic disease in this group.
Discussion
We found that OPS was being performed on significantly larger tumors than those treated with a WLE (32.1 mm vs. 18.8 mm; p<0.05). This was similarly the case where the weight of the tumor was concerned (177 grams vs. 73.1 grams; p<0.05). Hence, some patients underwent a quadrantectomy which is not a routine practice in the UK. These procedures resulted in a decrease in the number of mastectomies we would have performed in these circumstances. The findings from our study are in agreement with the existing literature on operative outcomes in OPS surgery. Clough [15] and Down et al. [16] have previously reported a preference for OPS in managing larger tumors. An average tumor size of 32 mm in a series of 101 therapeutic mammoplasties was reported by the former study, while the latter reported an average size of 23.9 mm in 37 OPS patients. Similarly, previous studies have reported specimen weights for therapeutic mammoplasty ranging from 222-236 g [1,17].
There was non-inferiority in the OPS group compared to the WLE group concerning margin clearance (4.7 mm vs. 3.5 mm p value=0.10). It is not surprising therefore that the number of re-excisions in the OPS group was lower than those recorded for the WLE group (8 versus 19 patients). However, an overall comparison of the further surgeries required between the two groups did not reveal a significant difference (p = 0.09). In those patients whose margins were found to be positive following OPS, six underwent completion mastectomies. There was only two re-excisions in this group. This is in contrast to the WLE group, where incomplete margins were managed with five completion mastectomies and fourteen re-excisions. This could be explained by the fact that patients undergoing OPS had a large resection at the initial surgery. In fact, one of the two patients in the OPS group who did undergo a wider excision reported in the patient satisfaction questionnaire that she was unhappy with the size of the breast. She is now contemplating a contralateral equalization surgery. The only option in most of these cases was a completion mastectomy on the second occasion. Interestingly, half of these patients opted for a reconstruction alluding to higher aesthetic expectations in this group. Those undergoing a wide local excision initially were more amendable for a wider excision
The definition of adequate margins remains controversial. Some studies have reported that more than 2 mm can be accepted, while others reported >5 mm clearance is acceptable. This controversy is discussed in the study by Giacalone, comparing OPS patients to quadrantectomy [18]. Hamdi [19] also compared the outcomes of patients who underwent either a quandrantectomy or tumorectomy (n=126) with those undergoing therapeutic mammoplasty (n=5) or mini flap reconstruction (n=21). Their OPS patients were younger with large tumors and considerably smaller breasts. Their margin clearance was greater than 2 mm for all patients.
In our study, the operating time was longer in the OPS group because of the larger number of axillary clearances involved. This would be expected given the larger size tumors in the OPS group resulting in a higher incidence of nodal disease. Follow up in both groups revealed two recurrences in the WLE group and one in the OPS group. Previously, there had been a concern that large tumors over 4 centimeters in size could result in a higher rate of local recurrence after breast conservation surgery. However, many retrospective analyses have indicated that tumor diameter is not a predictive factor for local recurrence free survival [20]. A number of studies have reported OPS is not associated with higher rates of disease recurrence or lower survival rates than standard techniques. Their conclusions are that these procedures are oncologically safe as the imperative factors are resection free margins and adjuvant radiotherapy [1,20]. Clough reported a 9.4% recurrence rate over a 5 year period for those treated with OPS [1]. Rietjens also noted local recurrence rates of 3% over a mean follow up of 74 months [21]. Likewise, we confirmed a low recurrence rate in the OPS group. The single patient recurred while on adjuvant chemotherapy for a surgically treated triple negative breast cancer with clear margins of more than 5 mm. This occurrence could be related to the tumor biology.
Our study had a number of limitations. Primarily, it is difficult to interpret our findings in the context of the general population. Patients were reviewed retrospectively from pre-specified surgical samples that had already been stratified according to their individual suitability to a particular surgery. There was a significant difference observed between our test groups in age and tumor type. It appears that OPS patients are on average younger. Seventy four percent of the OPS population was available for the questionnaire. As this was a retrospective study, we were unable to get all the patient’s input on their cosmetic satisfaction survey. The outcomes, though, would not have been dramatically affected if the further 28% in the OPS group had scored the questionnaire. Additionally, we did not collect data on the surgeon’s perspective of the cosmetic result as the retrospective nature of the study limited this aspect.
Conclusion
Our study has confirmed that oncoplastic breast resections provide non inferior results when compared with wide local excision while ensuring good levels of breast cosmesis. OPS was performed in patients with larger tumors suggesting it should be considered. There was no significant difference in the complication rates. In conclusion, we have found that OPS present an acceptable technique for patients with larger breast tumors desiring breast conserving therapy. Our study has demonstrated acceptable cosmetic outcomes and low recurrence rates.
References
- Clough KB, Lewis JS, Couturaud B, Fitoussi A, Nos C, et al. (2003) Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg 237: 26-34.
- Dillon MF, Hill AD, Quinn CM, McDermott EW, O'Higgins N (2006) A pathologic assessment of adequate margin status in breast-conserving therapy. Ann SurgOncol 13: 333-339.
- Munhoz AM, Aldrighi CM, Ferreira MC (2007) Paradigms in oncoplastic breast surgery: a careful assessment of the oncological need and esthetic objective. Breast J 13: 326-327.
- Franceschini G, Terribile D, Magno S, Fabbri C, Accetta C, et al. (2012) Update on oncoplastic breast surgery. Eur Rev Med PharmacolSci 16: 1530-1540.
- Masetti R, Di Leone A, Franceschini G, Magno S, Terribile D, et al. (2006) Oncoplastic techniques in the conservative surgical treatment of breast cancer: an overview. Breast J 12: S174-180.
- Losken A1, Hamdi M (2009) Partial breast reconstruction: current perspectives. PlastReconstrSurg 124: 722-736.
- Anderson BO, Masetti R, Silverstein MJ (2005) Oncoplastic approaches to partial mastectomy: an overview of volume-displacement techniques. Lancet Oncol 6: 145-157.
- Franceschini G, Magno S, Fabbri C, Chiesa F, Di Leone A, et al. (2008) Conservative and radical oncoplasticapproches in the surgical treatment of breast cancer. Eur Rev Med PharmacolSci 12: 387-396.
- Hernanz F, Regaño S, Redondo-Figuero C, Orallo V, Erasun F, et al. (2007) Oncoplastic breast-conserving surgery: analysis of quadrantectomy and immediate reconstruction with latissimusdorsi flap. World J Surg 31: 1934-1940.
- Kijima Y, Yoshinaka H, Hirata M, Mizoguchi T, Ishigami S, et al. (2011) Immediate reconstruction using a modified thoracodorsaladipofascial cutaneous flap after partial mastectomy. Breast20: 464-467.
- Gray JR, McCormick B, Cox L, Yahalom J (1991) Primary breast irradiation in large-breasted or heavy women: analysis of cosmetic outcome. Int J RadiatOncolBiolPhys 21: 347-354.
- Moody AM, Mayles WP, Bliss JM, A'Hern RP, Owen JR, et al. (1994) The influence of breast size on late radiation effects and association with radiotherapy dose inhomogeneity. RadiotherOncol 33: 106-112.
- Chan SW, Cheung PS, Lam SH (2010) Cosmetic outcome and percentage of breast volume excision in oncoplastic breast conserving surgery. World J Surg 34: 1447-1452.
- Al-Ghazal SK, Fallowfield L, Blamey RW (1999) Patient evaluation of cosmetic outcome after conserving surgery for treatment of primary breast cancer. Eur J SurgOncol 25: 344-346.
- Clough KB, Kroll SS, Audretsch W (1999) An approach to the repair of partial mastectomy defects. PlastReconstrSurg 104: 409-420.
- Down SK, Jha PK, Burger A, Hussien MI (2013) Oncological advantages of oncoplastic breast-conserving surgery in treatment of early breast cancer. Breast J 19: 56-63.
- Yang JD, Lee JW, Cho YK, Kim WW, Hwang SO, et al. (2012)Surgical techniques for personalized oncoplastic surgery in breast cancer patients with small to moderate sized breasts (part 2). J Breast Cancer 15: 7-14.
- Giacalone PL, Roger P, Dubon O, El Gareh N, Rihaoui S, et al. (2007) Comparative study of the accuracy of breast resection in oncoplastic surgery and quadrantectomy in breast cancer. Ann SurgOncol 14: 605-614.
- Hamdi M, Sinove Y, DePypere H, Van Den Broucke R, Vakaet L, et al. (2008) The role of oncoplastic surgery in breast cancer. ActaChirBelg 108: 666-672.
- Fitzal F1, Riedl O, Wutzl L, Draxler W, Rudas M, et al. (2007) Breast-conserving surgery for T3/T4 breast cancer: an analysis of 196 patients. Breast Cancer Res Treat 103: 45-52.
- Rietjens M, Urban CA, Rey PC, Mazzarol G, Maisonneuve P, et al. (2007) Long-term oncological results of breast conservative treatment with oncoplastic surgery. Breast 16: 387-395.
Citation: Khawaja S, Saiyed A, Thayabaran D, Udayasankar S, Dias J, et al. (2015) A Comparison Between Oncoplastic Breast Conserving Surgery and Standard Wide Local Excision: A UK Experience. J Blood Lymph 1:102. DOI: 10.4172/2572-4118.1000102
Copyright: © 2015 Khawaja S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 15378
- [From(publication date): 3-2016 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 14227
- PDF downloads: 1151