Research Article Open Access
A Multiple Component Intervention to Assist Young Pregnant Smokers to Cease Smoking: A Randomised Controlled Pilot Study
Lucy Lewis1*, Yvonne Hauck1, Fiona Ronchi2, Steve Allsop3 and Dorota Doherty41School of Nursing, Midwifery and Paramedicine, Curtin University, Bentley, Perth, and Department of Nursing and Midwifery Education and Research, King Edward Memorial Hospital, Subiaco, Australia
2Department of Nursing and Midwifery Education and Research, King Edward Memorial Hospital, Western Australia, Australia
3National Drug Research Institute Curtin University, Bentley, Perth, Western Australia
4Women and Infants Research Foundation, Subiaco, King Edward Memorial Hospital, Western Australia, Australia
- *Corresponding Author:
- Lucy Lewis
Midwifery Research Fellow, School of Nursing
Midwifery and Paramedicine, Curtin University
Bentley, Perth, and Department of Nursing and Midwifery Education and Research
King Edward Memorial Hospital, Subiaco, Australia
Tel: 61 8 6458 3024
Fax: +61 8 9340-1590
E-mail: Lucy.Lewis@health.wa.gov.au
Received date: November 17, 2016; Accepted date: January 04, 2017; Published date: January 11, 2017
Citation: Lewis L, Hauck Y, Ronchi F, Allsop S, Doherty D (2017) A Multiple Component Intervention to Assist Young Pregnant Smokers to Cease Smoking: A Randomised Controlled Pilot Study. J Addict Res Ther 8:303. doi:10.4172/2155-6105.1000303
Copyright: © 2017 Lewis L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Addiction Research & Therapy
Abstract
Objective: Australian rates of cigarette smoking are the lowest in the world. Young pregnant smokers are a sub population where smoking remains high. This pilot study assessed the feasibility of a multi-component intervention (Carbon Monoxide testing, motivational interviewing and a non-smoking buddy) to assist young pregnant women to cease smoking. Methods: Between October 2013 and June 2015, this multi-centred West Australian study recruited pregnant smokers aged 16 to 24, attending their first antenatal visit. Women (n=80) were randomised to the intervention and standard smoking cessation advice (n=43) or standard smoking cessation advice alone (n=37). At 36 weeks gestation and six weeks post birth, cessation rates were compared between groups using repeated measures survival analysis and reduction in smoking was examined using repeated measures linear regression on the number of cigarettes smoked. Results: The majority (89%) of women were unemployed or not in education, used illicit drugs (43%) and had experienced sexual abuse (23%). Involvement with child protection services was common (38%). Cigarette initiation occurred at a mean age of 13 years, median number of cigarettes smoked at baseline was 10 in both groups. Smoking cessation in intervention and controls were 17% vs. 14% at 36 weeks and 23% vs. 7% 6 weeks post birth. No significant differences in cessation or smoking reduction between groups were found individually or in the repeated events analysis. Conclusion: Given the low number of participants our findings cannot conclusively rule out this multi-component intervention. We believe it remains possible this intervention may prove effective in a larger group of participants and in another setting. Monitoring trends in this vulnerable, difficult to engage group of pregnant young women is important if we are to continue to devise effective interventions.
Keywords
Smoking cessation; Pregnancy; Young women; Vulnerable populations; Randomised controlled trial; Pilot study.
Introduction
Australian rates of cigarette smoking are the lowest in the world [1]. In 2010 the proportion of the Australian population 14 years and older who identified themselves as tobacco smokers was 15% [1,2]. However, there are a number of sub populations where smoking remains high: the unemployed; socially disadvantaged; those with psychological issues; those who use alcohol and other drugs; and Aboriginal and Torres Strait Islanders [1-9].
Prior to 2008 there were no Australian national data available for smoking in pregnancy. By 2008 data on smoking status in pregnancy were available for seven states and territories [10]. Nationally, 16% of women smoked during pregnancy with 39% of teenage mothers and 51% of Aboriginal or Torres Strait Islander women smoking tobacco during pregnancy [10]. By 2013, 12% of women who gave birth smoked at some time during their pregnancy with the proportion of women smoking under 20 years old being 34% and Aboriginal and Torres Strait Islanders being 47%. However, 22% of those who reported smoking during the first 20 weeks of pregnancy did not continue to smoke after 20 weeks gestation [11].
Tobacco smoking in pregnancy remains one of the few preventable factors associated with complications in pregnancy. Women who continue to smoke through pregnancy are at increased risk of placental abruption [7,12], an infant with low birth weight and preterm birth before 37 weeks gestation [7,13]. Australian evidence suggests the pregnant women least likely to cease smoking are the young, socioeconomically disadvantaged and Aboriginal and Torres Strait Islanders [14]. However, a higher proportion of women stop smoking during pregnancy than at any other time in their lives [15].
The aim of this randomised controlled pilot study was to assess the feasibility of a multi-component intervention to assist young pregnant smokers cease smoking. We hypothesised more women assigned to the intervention group would reduce the number of cigarettes they smoke or cease smoking completely, compared to the control group.
Methods
Patients and recruitment
Pregnant women, who reported smoking tobacco at their first hospital visit for antenatal care, were invited to participate. Inclusion criteria included: a desire to cease smoking; being between 16 and 24 years old; able to speak English; pregnancy between 10 and 28 weeks gestation; having access to a mobile phone; and being able to identify a non-smoking buddy to support with smoking cessation at least twice a week. A research midwife, not involved in clinical care, used verbal and written explanations to recruit and obtain informed consent.
Randomisation
Women in this prospective, allocation concealed, randomised controlled trial were assigned to a multiple component intervention with standard smoking cessation advice or standard smoking cessation advice alone. Standard smoking cessation advice included the 5A’s program which: asks about smoking status; assesses willingness to cease smoking; advises cessation; assists with cessation; and arranges follow up [16]. Women were also offered a referral to the Australian ‘Quit Line’. The multiple component intervention included Carbon monoxide (CO) testing, a non- smoking buddy and motivational interviewing (MI). Blinding participants and staff to group assignment was not possible due to the smoking cessation interventions employed. If a woman missed an antenatal appointment she was telephoned with a new appointment. Women who missed a subsequent appointment and had been identified as vulnerable at their first visit for antenatal care received a home visit from a midwife.
The study was funded through a Healthway Starter Grant (22910). Ethics approval was gained at the two hospital sites (2022/EW and W/ 13/61). Both hospitals were metropolitan public obstetric hospitals in Western Australia (WA), with the majority of women recruited at the sole tertiary obstetric hospital. The study was performed from October 2013 to June 2015.
Interventions
Carbon monoxide testing
A CO test measures the amount of CO in a person’s expired breathe, using a small hand held machine. This non-invasive test offers immediate feedback on an individual’s smoking status via a visual traffic light system (green, amber, red) and auditory beeping, which increases in conjunction with the level of CO measured. In pregnancy, a single CO test enables women to receive feedback on the impact of their tobacco smoking on themselves and their unborn child [12,17]; as such it is used to motivate smoking cessation [18]. Standard clinical practice in both study settings did not include CO testing. In this study CO testing was performed at each antenatal visit or the time of each scheduled antenatal visit if the woman was an inpatient. The study utilised a Bedfont Smokerlyzer (manufactured in Maidstone in the United Kingdom), designed specifically to monitor CO levels in pregnancy.
Non-smoking buddy
Smoking cessation interventions which improve social support are emerging as an effective way for disadvantaged groups to manage their health [19]. A recent review found the use of a non-smoking buddy when combined with individual counselling may more than double the short term smoking cessation/reduction in teenagers [20]. Prior to consent women in this study were asked if they could identify a selfnominated non-smoking buddy to assist with smoking cessation who they could chat with at least twice a week every two weeks from recruitment to six weeks post birth.
Motivational interviewing
Motivational interviewing is a strategy which strengthens an individual’s motivation to change their behaviour [21]. A review of 29 studies including 6000 young smokers found evidence of the efficacy of MI as an effective strategy to assist with smoking cessation [22]. Women in this study received MI every two weeks from recruitment to six weeks post birth and could opt to have their interview incorporated into their antenatal appointment or at an alternative time over the phone. Interviews concentrated on smoking goals, how women were progressing with these goals and identification of situations that triggered their desire to smoke. The research midwife performing the motivational interviews completed motivational interview training.
Data collection
A baseline questionnaire was administered face to face immediately following recruitment and repeated over the phone six weeks post birth. This questionnaire utilised standard questions developed by the American Academy of Paediatrics to assess smoking history and behaviour [23]. Additional information was obtained on partner smoking behaviour, whether their pregnancy had provided motivation to alter their smoking and their baby’s cigarette exposure post birth.
At baseline, 36 weeks gestation and six weeks post birth women were asked how many cigarettes they were smoking daily. Verification of smoking status and baby’s smoke exposure post birth was dependant on self-report and did not include biochemical verification. Post birth information was collected from the women’s medical records in relation to: their demographic data (ethnicity, socioeconomic and employment status); obstetric data (antenatal admission, mode of birth); and infant history (gestation, birth weight, admission to special care nursery, breastfeeding).
Statistical methods
Assuming the prevalence of smoking cessation among pregnant women aged 16 to 24 years was 20%, a sample of 100 women was sufficient to detect a two-fold in smoking cessation from 30% to 60% with 80% power when using a two-sided Fisher exact test of proportion at 0.05 significance level. The large effect size was chosen because the intervention involved a multi-component, time consuming intervention, to assess feasibility.
Means, medians and interquartile ranges were used to summarise continuous data (such as the number of cigarettes smoked). Univariate comparisons between the intervention and control groups were performed using Mann-Whitney tests and Chi square tests. Repeated cessation events were modelled using Cox proportions hazards regression model with each smoking cessation event as an independent event of smoking cessation at 36 weeks gestation and six weeks post birth and while censoring women lost to follow. The effects of the intervention were summarised using hazard ratios (HR) and their 95% confidence intervals (CI).
Supplementary analysis of the self-reported average number of cigarettes smoked at 36 weeks gestation and six weeks post birth was performed using repeated measured linear regression with individual participants modelled as random effects. SPSS statistical software (version 21, IBM SPSS Statistics for Windows, Version 20.0 Armonk, NY: IBM Corp) was used for data analysis. P values <0.05 were considered statistically significant.
Results
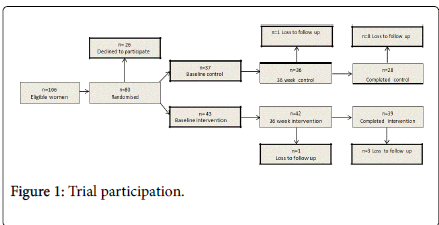
A total of 106 women were approached and 80 (76%) were recruited, 43 were randomised to the intervention and standard smoking cessation advice and 37 to standard smoking cessation advice alone (Figure 1). The most frequent reason for not participating in the study was not wanting to cease or reduce the number of cigarettes smoked (42%; 11of 26). Nine women in the control arm were lost to follow up (seven were unable to be contacted, one had a perinatal loss at 23 weeks gestation and one had her baby apprehended by social services and did not want to continue with the study). Four women in the intervention arm were lost to follow up (two were unable to be contacted and two had their baby apprehended by social services and did not want to continue with the study).
Cigarette initiation occurred at a mean of 13 years, with the mean age women started smoking regularly being a year later. Most (67%) women were Caucasian, with the majority (89%) being unemployed or not in education. Just over half (55%) lived in an area of low socioeconomic status. Most women (77%) had partners who smoked. Illicit drug use was reported by 43% and sexual abuse by 23%. Post birth the majority (82%) of infants were not exposed to cigarette smoke and 38% of women disclosed they were referred to child protection services (Table 1).
| Characteristic | Total n=80 n (%) | Intervention n=43 (54%) n (%) | Control n=37 (46%) n (%) | P Value | ||
|---|---|---|---|---|---|---|
| Demographics | Age | Mean/Median (IQR) [R] | 20/21 (19-22) [16-24] | 20/21 (18-22) [16-24] | 20/21 (19-22) [16-24] | 0.57 |
| Ethnicity | Caucasian | 54 (67) | 27 (63) | 27 (73) | 0.551 | |
| Aboriginal | 22 (28) | 14 (32) | 8 (22) | |||
| âÂ? Other | 4 (5) | 2 (5) | 2 (5) | |||
| Asthmatic | 22 (28) | 16 (37) | 6 (16) | 0.03 | ||
| Tobacco smoking | Age smoked first cigarette | 13/13 (13-15) [4-18] | 13/13 (13-15) [10-18] | 13/13 (13-15) [4-18] | 0.146 | |
| Age smoked regularly | 14/14 (14-16) [9-20] | 14/14 (13-16) [9-20] | 14/14 (14-16) [10-18] | 0.888 | ||
| Number smoked at baseline | 10/10 (4-15) [1-40] | 10/10 (4-15) [1-40] | 11/10 (5-15) [2-30] | 0.796 | ||
| 95% CI number baseline | 8.71-12 | 7.75-12.55 | 8.27-12.92 | 0.789 | ||
| Number smoked 36 weeks | 7/5 (2-11) [0-25] | 7/5 (2-10) [0-25] | 8/7 (2-12) [0-25] | 0.487 | ||
| 95% CI number smoked 36 weeks | 5.63-8.47 | 4.71-8.46 | 5.34-9.83 | 0.487 | ||
| Number smoked post birth | 7/5 (2-12) [0-30] | 7/5 (1-11) [0-30] | 8/7 (3-12) [0-25] | 0.533 | ||
| 95% CI number smoked post birth | 5.43-8.92 | 4.17-9.10 | 5.35-10.47 | 0.475 | ||
| Smoker baseline to 36 weeks | 66 (85) | 35(83) | 31 (86) | 0.765 | ||
| Smoker 36 weeks to post birth | 56 (84) | 30 (77) | 26 (93) | 0.104 | ||
| âÂ?¡Cessation attempts | pregnancy =1 | 17 (27) | 10 (28) | 7 (26) | 0.87 | |
| Continuously | 46 (73) | 26 (72) | 20 (74) | |||
| *Partner smokes | 49 (77) | 25 (78) | 24 (75) | 0.768 | ||
| Psychosocial history | Low socioeconomic status | 44 (55) | 22 (51) | 22 (60) | 0.457 | |
| Unemployed not in education | 71 (89) | 36 (84) | 35 (95) | 0.125 | ||
| Involvement with Child Protection | 30 (38) | 17 (43) | 13 (35) | 0.685 | ||
| Illicit drug use | 34 (43) | 17 (40) | 17 (46) | 0.563 | ||
| Reports sexual abuse | 18 (23) | 8 (19) | 10 (27) | 0.368 | ||
| Obstetric history | Antenatal admission | None | 46 (57) | 25 (58) | 21 (57) | 0.598 |
| = 1 | 34 (43) | 18 (42) | 16 (43) | |||
| ± Mode of birth | Vaginal | 62 (79) | 32 (76) | 30 (81) | 0.598 | |
| Caesarean | 17 (21) | 10 (24) | 7 (19) | |||
| Infant | Gestation a birth | <37 weeks | 22 (27) | 12 (29) | 10 (24) | 0.67 |
| = 37 weeks | 58 (73) | 30 (71) | 28 (76) | |||
| ? Birth weight= 2500 kg | 24 (29) | 14 (33) | 10 (36) | 0.492 | ||
| ? Resuscitation at birth | 32 (39) | 16 (38) | 16 (41) | 0.787 | ||
| ? Special Care Nursery admission | 25 (31) | 13 (31) | 12 (31) | 0.986 | ||
| Breast fed | 65 (82) | 36 (84) | 29 (81) | 0.7 | ||
| No cigarette exposure post birth | 52 (82) | 28 (78) | 24 (89) | 0.157 | ||
Table 1: Characteristics of women and their infants according to randomisation; Outcomes may not add up to 100 due to missing outcomes for some variables; Participants included n=80 at baseline, n=78 at 36 weeks of pregnancy and n=67 postpartum; âÂ? Other ethnicity include Asian, Maori and African; ? Of n=63 who made a quit attempt in pregnancy *Of n=64 who had a partner; ±Of n=62 women who had a vaginal birth, n=53 had a spontaneous vaginal birth and n=9 had an assisted birth. Of n=17 women who had a caesarean, n=7 had an emergency caesarean and n=10 had an elective caesarean. The mode of birth was unknown for 1 woman; ? Includes n=3 sets of twins and excluded n=1 intrauterine death at 23 weeks gestation.
Median number of cigarettes smoked at baseline was 10 per day in both groups. Smoking cessation in intervention and controls groups respectively were 17% vs. 14% at 36 weeks gestation and 23% vs. 7% at six weeks post birth. No significant differences in cessation or smoking reduction between groups were found individually or in the repeated events analysis (The HR was 2.52 (95% CI 0.83-7.64), p=0.104). Repeated measured linear regression showed no significant differences between the number of cigarettes smoked between the groups overall (p=0.609) and between groups over time (interaction p=0.951).
Of the 43 women randomised to the intervention seven (16%) did not manage to engage a non-smoking buddy; one women asked four people, two women asked two people and four women could only identify one non-smoking buddy in their social sphere. Nineteen women (44%) had one non-smoking buddy during the course of their pregnancy. The 17 women who lost their initial non-smoking buddy were asked to nominate a subsequent buddy. Of those who lost their non-smoking buddy, 11 (26%) had two non-smoking buddies and six (14%) had between three and five non-smoking buddies. Of the 36 women who commenced the study with a non-smoking buddy, nine (25%) did not have a non-smoking buddy post birth.
A total of 172 MI’s were performed in pregnancy, with 149 (87%) completed in antenatal clinic in conjunction with CO monitoring. Women opted to have 23 (13%) MI’s over the telephone. There were 12 (28%) women in the intervention that missed at least one scheduled antenatal appointment.
Discussion
The aim of this pilot study was to test the feasibility of a multiple component intervention (CO monitoring, MI and a non-smoking buddy) to assist young pregnant smokers to cease smoking. Our analysis found no statistically significant differences between groups. Discussion will focus on why the intervention proved ineffective (lessons learnt) and why young women who continue to smoke throughout pregnancy may benefit from targeted assessment of illicit drug use, suicidal ideation, and sexual abuse.
This research was built on the foundation of prior research by members of this team which found women who ceased smoking valued a supportive relationship with someone sensitive to their smoking goals [24]. Additionally our multiple component intervention was evidence based [17,21,22,25] but still failed to produce the large effect hypothesised in the study. Although our results were not statistically significant, there was a clear trend towards higher cessation levels in the intervention group. We believe insufficient statistical power may have resulted in inconclusive evidence to support our hypothesis.
A main objective of this pilot study was to provide information on the feasibility of employing the multi-component intervention in this cohort of vulnerable smokers. However, the study may have been more useful if we had considered the multiple component intervention as three different components rather than one [25]. It is clear many women found it hard to sustain a relationship with one non-smoking buddy. If the relationship with the initial non-smoking buddy ended, it was often difficult for women to identify an alternative non-smoking buddy in a social environment where smoking was the norm [25].
In addition, we assumed from previous evidence that the MI employed would foster an environment in which women were able to freely disclose their cigarette use and work to cease or reduce their cigarette smoking [25,26]. Retrospectively MI could have been individually tailored away from antenatal clinic and in an environment of the woman’s choice. We were also unable to assess to assess the impact of having MI away from the antenatal clinic over the telephone as only a minority of women chose this option.
It is important to monitor trends in sub populations of pregnant young women vulnerable to smoking, such as those who experience trauma or violence and those who use illicit drugs, to develop and evaluate program effectiveness [27]. Women who consented to this study wanted to cease smoking but had competing areas of foci which took priority (such as use of illicit drugs and sexual abuse) [8,28]. Our experience was that as a woman’s use of illicit drugs in pregnancy decreased their smoking increased. We also noted the impact of having a child removed by child protection services post birth, contributed to stress which triggered smoking [8]. We acknowledge the multicomponent intervention did not empower women to address these harms individually [25] and suggest this approach is central if health professionals are to develop comprehensive smoking cessation programs for this vulnerable cohort.
Limitations
This pilot study has limitations that should be considered. No specific subpopulation of pregnant smokers was targeted. The study was small and may not be representative of the population of young pregnant smokers in WA. Smoking history was dependant on the women’s personal recall of their smoking behaviour and willingness to disclose their smoking. We did not objectively confirm their nicotine levels. Psychosocial history was dependant on women being willing or able to recount their trauma around sexual assault. The stigma associated with illicit drug use during pregnancy may have made some women reluctant to discuss their drug use history.
Conclusion
It is important to monitor trends in sub populations of pregnant young women vulnerable to smoking, to work out which aspects of cessation programmes work. Although our multi- component intervention was tailored for this cohort, it failed the reality test. We hope the lessons learned and insights gained will assist other health professionals in this field.
References
- Australian National Preventive Health Agency (ANPHA) (2013) Smoking and disadvantage: Evidence brief. Canberra: Australian government. ANPHA.
- Australian Institute of Health and Welfare (AIHW) (2012) AustralianâÂ?Â?s Health. Canberra: AIHW.
- Courtney RJ, Clare P, Boland V, Martire KA, Bonevski B, et al. (2016) Predictors of retention in a randomised trial of smoking cessation in low-socioeconomic status Australian smokers. Addict Behav 64:13-20.
- Stockings E, Bowman J, McElwaine K, Baker A, Terry M, et al. (2013) Readiness to quit smoking and quit attempts among Australian mental health inpatients. Nicotine Tob Res 15: 942-949.
- Hotham ED, Ali RL, White JM, Robinson JS (2016) Ethical considerations when researching with pregnant substance users and implications for practice. Addict Behav 60: 242-243.
- O'Connor A, Lewis L, McLaurin R, Barnett L (2015) Maternal and neonatal outcomes of Hepatitis C positive women attending a midwifery led drug and alcohol service: A West Australian perspective. Midwifery 31: 793-797.
- Taplin S, Richmond G, McArthur M (2015) Identifying alcohol and other drug use during pregnancy: Outcomes for women their partners and their children. Canberra. Australian National Council on Drugs.
- Pateman K, Ford P, Fizgerald L, Mutch A, Yuke K, et al. (2016) Stuck in the catch 22: Attitudes towards smoking cessation among populations vulnerable to social disadvantage. Addiction 111: 1048-1056.
- Passey ME, Longman JM, Robinson J, Wiggers J, Jones LL (2016) Smoke-free homes: What are the barriers, motivators and enablers? A qualitative systematic review and thematic synthesis. BMJ Open 6: e010260.
- Laws P, Li Z, Sullivan EA (2010) AustraliaâÂ?Â?s mothers and babies. Perinatal statistics series no 24. Cat. No PER 50. Canberra, Australia: AIHW National Perinatal Epidemiology and Statistics Unit.
- Laws P, Li Z, Sullivan EA (2015) Australia's mothers and babies. Perinatal statistics series no. 31. Cat. No. PER 72. Canberra: AIHW National Perinatal Epidemiology and Statistics Unit.
- Lumley J, Chamberlain C, Dowswell T, Oliver S, Oakley L, et al. (2009) Interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev 3: CD001055.
- Dahlin S, Gunnerbeck A, Wikström AK (2016) Maternal tobacco use and extremely premature birth- A population-based cohort study. BJOG 123: 1938-1946.
- Passmore E, McGuire R, Correll P, Bentley J (2015) Demographic factors associated with smoking cessation during pregnancy in New South Wales, Australia, 2000-2011. BMC Public Health 15: 398.
- Chamberlain C, O'Mara-Eves A, Oliver S, Caird JR, Perlen SM, et al. (2013) Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database Syst Rev CD001055.
- Naughton F, Prevost AT, Sutton S (2008) Self-help smoking cessation interventions in pregnancy: A systematic review and meta-analysis. Addiction 103: 566-579.
- National Institute of Clinical Excellence (2010) Quitting smoking in pregnancy and after childbirth. NICE public health guidance PH26.
- Sloan M, Campbell KA, Bowker K, Coleman T, Cooper S, et al. (2016) Pregnant Women's Experiences and Views on an "Opt-Out" Referral Pathway to Specialist Smoking Cessation Support: A Qualitative Evaluation. Nicotine Tob Res 18: 900-905.
- Ford P, Clifford A, Gussy K, Gartner C (2013) A systematic review of peer-support programs for smoking cessation in disadvantaged groups. Int J Environ Res Public Health 10: 5507-5522.
- Bauld L, Bell K, McCullough L, Richardson L, Greaves L (2010) The effectiveness of NHS smoking cessation services: A systematic review. J Public Health (Oxf) 32: 71-82.
- Connery HS, Albright BB, Rodolico JM (2014) Adolescent substance use and unplanned pregnancy: Strategies for risk reduction. Obstet Gynecol Clin North Am 41: 191-203.
- Stanton A and Grimshaw G (2013) Tobacco cessation interventions for young people. Cochrane Database Syst Rev 8: CD003289.
- American Academy of Pediatrics (2016) Julius B. Richmond Center of Excellence. Surveys, questions and assessment tools.
- Hauck Y, Ronchi F, Lourey B, Lewis L (2013) Challenges and enablers to smoking cessation for young pregnant Australian women: A qualitative study. Birth 40: 202-208.
- Greaves L, Poole N, Okoli C, Hemsing N, Qu A, et al. (2011) Expecting to quit: A best practices review of smoking cessation interventions for pregnant and postpartum women. (2nd ed), Vancouver: Centre of Excellence for WomenâÂ?Â?s Health.
- Bottorff JL, Poole N, Kelly MT, Greaves L, Marcellus L, et al. (2014) Tobacco and alcohol use in the context of adolescent pregnancy and postpartum: A scoping review of the literature. Health Soc Care Community 22: 561-574.
- Twyman L, Bonevski B, Paul C, Bryant J (2014) Perceived barriers to smoking cessation in selected vulnerable groups: A systematic review of the qualitative and quantitative literature. BMJ Open 4: e006414.
- MacArthur G, Harrison S, Caldwell D, Hickman M, Campbell R (2016) Peer-led interventions to prevent tobacco, alcohol and/or drug use among young people aged 11-21 years: A systematic review and meta-analysis. Addiction 111: 391-407.
Relevant Topics
- Addiction Recovery
- Alcohol Addiction Treatment
- Alcohol Rehabilitation
- Amphetamine Addiction
- Amphetamine-Related Disorders
- Cocaine Addiction
- Cocaine-Related Disorders
- Computer Addiction Research
- Drug Addiction Treatment
- Drug Rehabilitation
- Facts About Alcoholism
- Food Addiction Research
- Heroin Addiction Treatment
- Holistic Addiction Treatment
- Hospital-Addiction Syndrome
- Morphine Addiction
- Munchausen Syndrome
- Neonatal Abstinence Syndrome
- Nutritional Suitability
- Opioid-Related Disorders
- Relapse prevention
- Substance-Related Disorders
Recommended Journals
Article Tools
Article Usage
- Total views: 3791
- [From(publication date):
February-2017 - Aug 28, 2025] - Breakdown by view type
- HTML page views : 2842
- PDF downloads : 949