About Non-infectious Scrotal Elephantiasis: 5 Cases with Management Algorithm
Received: 19-Sep-2019 / Accepted Date: 29-Nov-2019 / Published Date: 06-Dec-2019 DOI: 10.4172/2165-7904.1000392
Abstract
Introduction: Despite the fact that massive scrotal elephantiasis is relatively uncommon in the Western world, the diagnostic and therapeutic know-how is highly important, since the condition has a huge impact on the patients’ quality of life. In endemic territories it is usually an infection that leads to this chronic, benign anomaly; however, in developed countries, more often than not, it is the aftermath of morbid obesity. The treatment algorithm requires extreme caution and sustained cooperation between the patient’s urologist, dermatologist, and plastic surgeon. Our aim is to demonstrate the process with visual aids.
Case description: In our work, we proudly present 5 cases, where gross scrotal elephantiasis was either idiopathic, or it could only be traced back to morbid obesity. All of our patients have been examined by a urologist, a dermatologist, and a plastic surgeon, and most of the operations were performed in the presence of the latter two.
Results: We could resect the redundant tissue in every case without any significant complications, and no relapse has been seen in the long-term follow-up (79-17, avg 45.4 months). Also, no major complications have occurred either, thanks to the thorough preparation, and pre-operative and intraoperative management.
Discussion: Since morbid obesity is more common today in the Western world than ever before, adiposity-related scrotal elephantiasis is also becoming more frequent in our time.
Conclusion: It is advised to prepare ourselves with the necessary knowledge of diagnosing and treating scrotal elephantiasis.
Keywords: Scrotal; Elephantiasis; Management; Operation; Noninfectious
Introduction
One can think of many reasons for scrotal enlargement: infection, neoplasm, hernia, and many others, however, scrotal elephantiasis will always stand out with its rarity and grotesque appearance. This abnormality stems from lymph stagnation caused by the compression of lymph vessels. It comes with a specific scrotal skin deformity (hence the name: elephant skin-like) and bilateral tumescence. The root cause can be of genetic nature, through the intrinsic failure of the lymphatic system, like in Milroy’s disease. Otherwise – and in most cases – it is a result of secondary problems, such as some form of blockage or compression in the lymphatic system [1,2]. Although this chronic lesion is benign, it has a major impact on the patient’s life, by turning everyday activities into misery to perform with a grossly enlarged scrotum. For a long time, it was uncommon in Europe and the Western world to see anyone with such a bizarre deformity, but we could find plenty of case studies from developing countries. In the endemic areas, it is mostly caused by infectious agents, mostly filarial [3,4]. On the Western hemisphere, this abnormality usually comes from the compression of lymph vessels by a pelvic tumor, a traumatic event, or a postoperative/postirradiation situation, dialysis, congenital causes, or massive obesity. However, only the last one is becoming more frequent nowadays [5,6]. The origin of the condition may differ, and the need for surgical intervention is undeniable in these cases. Therefore, it is essential to be familiar with the management of this disorder.
In our work, we proudly present our contribution to the topic with 5 of our well-documented cases (operated by our team of urologists and plastic surgeons), and general ideas about the treatment.
Case Description
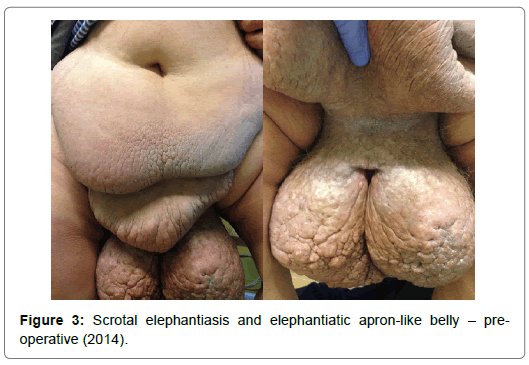
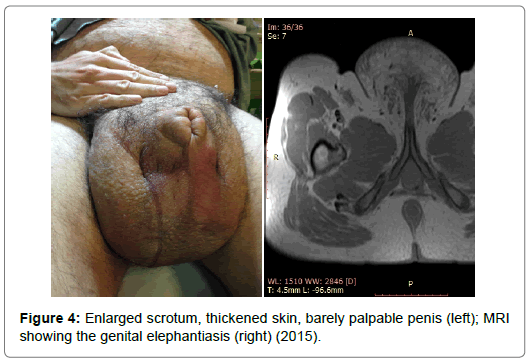
Five young (23-49 years, avg: 39.4 y) males with no significant complaints – other than a massive scrotal enlargement and (with one exception) morbid obesity (BMI>40 kg/m2). None of them had received and treatment previously. The examination protocol always involved the following: First, the patient’s history was taken. After physical examination, weight measurement, and photo documentation we asked the patients about any former dermatological conditions, weight changes, the onset of the problem, and especially about any excursion to any exotic locations - especially Africa, South-East Asia or India. Lab tests were performed to identify any signs of infection. CT and MRI were also performed to see if there were any signs of lymph vein compression by a pelvic tumour or something else. After our initial examinations, we referred each patient to a dermatologist and to a plastic surgeon – although the latter was not always present in the operating theatre, his help in planning and further treatment was indispensable.
Since none of the cases were declared to be of infectological or oncological origin, we pronounced them to be idiopathic or the result of obesity.. The body mass indexes of our patients at the initial examinations were the following: 74 kg/m2, 57 kg/m2, 42 kg/m2, 41 kg/ m2 and 26 kg/m2, meaning four of them were morbidly obese, and one – after significant weight loss – was only slightly overweight.
In the first line, we supplied our clients with lifestyle advices to help them lose the redundant weight. Although all of our patients achieved some level of weight loss, their complaints did not lessen and they were still suffering from their obnoxious condition – a surgery was still needed.
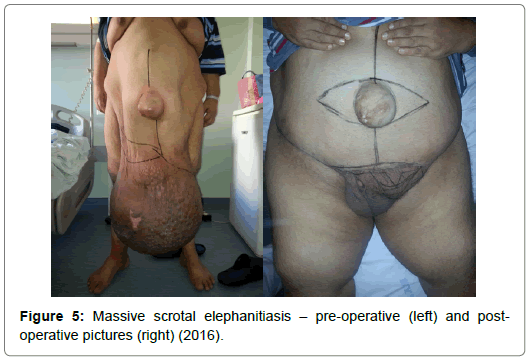
Before we even started planning any kind of surgical intervention, we took additional time to discuss the possible outcomes and complications with the patients. We described the possible complications (such as surgical site infection, wound healing problems, the possible need for transfusion, etc.) in detail, and informed them about the importance of aftercare and the possibility of further operations (like abdominal plastic surgery) as well. Furthermore, we also discussed the potential discrepancy between the expected and the actual optical results of subsequent surgery to prevent any disappointment. Furthermore, the patients received preventive antibiotics (Amoxicillin/Clavulanic acid combination) and were prudently prepared by anaesthesiologists.
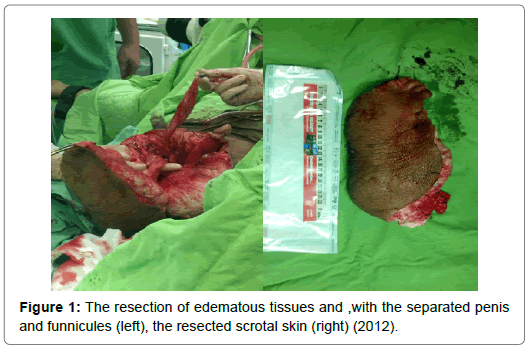
The operations had some similar basic steps we followed each time. First, we cut along the scrotal raphe halving the elephantiatic area. Then, we cut around the lateral, dorsal, and anterior edges of the anomaly, and – parallel with the isolation of the testicles and the penis – we removed the thickened scrotal skin. Not once did we need to use skin flaps or auto transplantation – we always covered the genital organs with preputial skin and residual (non-elephantiatic) scrotal tissue (Figures 1-5). After the resections, drainage tubes were placed in the wounds, and removed on the second postoperative day. During the surgeries, continuous blood pressure monitoring and intraoperative fluid management was especially important, as the massive loss of extra- and intracellular fluid could have caused serious blood- pressure instability. There was no notable intraoperative event, and only one patient had to receive transfusion. Surgical site infection and serious wound healing problems did not occur either, thanks to the appropriate wound care. None of our patients had any complications that would have required reoperation. In the postoperative period, long-term thromboprophylaxis and antibiosis were our major concerns, besides, of course, dietetic and health counselling. The resected tissue (weighing from 5 to 30 kilograms) was sent to pathology in all cases: none of the histology results reported inflammation, infection, or neoplasm. The patients spent an average of 5.7 (4-9) days in hospital bed. The followup time after the primary operation is 45.4 months on average (79-17). Within this time frame, none of the patients had recurrent scrotal or genital elephantiasis. Three of the patients required further operations: two had to go through surgical reduction of their apron-like abdomen. One patient had recurrent edema in the genital region – laparoscopic lymph vein clamping resolved the problem.
Discussion
Scrotal elephantiasis, the result of the chronic insufficiency of lymph drainage, is easily characterized by the intracutaneous fluid retention, edema, and hardened skin in the genital region. The entity can either be congenital (primary) or acquired (secondary) through the compression or blockage of lymph veins. Although this condition has various origins, it is becoming more frequent (in the Western hemisphere) as a result of morbid obesity (BMI>40 kg/m2) [7]. As gross abdominal adiposity compresses the lymph veins inhibiting the natural flow of chyle, it is only a matter of time when the edema and the consequent fibrosis appears, followed by cutaneous hyperkeratosis and dryness [8]. The major complaint –appearing in our patients only years after the onset emerged – is the massive size and weight of the lesion.
In our experience, the treatment of each case should start with examining the patient’s physical condition and their history. After the general assessment, it is advised to search for possible root causes (like oncological, dermatological, infectological, etc.) and rule them out. If the imaging studies and lab results show no abnormalities, weight loss can be advised, although it may not help with the scrotal enlargement.
Whilst the connection between weight loss and scrotal lymphedema is not very well understood (and according to some, it is even reciprocal), weight loss is still advisable for patients with major scrotal elephantiasis: first of all, by losing weight, the compression on the lymphatic system might be reduced, and by that, the edema might decrease as well. Secondly, a patient who is less overweight may face less peri- and postoperative complications and wound healing disorders [9].
After consulting a plastic surgeon (preferably with considerable experience on the field), the next step is surgical intervention, with proper anaesthesiological assistance. Wound care, antibiosis (preferably amoxicillin or other penicillin-type agents) and close attention to fluid balance is necessary. We’d also like to add, that in our practice we refrained from using any kind of skin grafts or mobilized flaps which, according to our opinion, could have led to a whole new set of problems and probably contributed to the higher rate of complications in other departments [10,11]. In case of the recurrence of the edema, the closing of local lymph veins can be recommended.
Conclusion
Conservative treatment and weight loss rarely (if ever) offer a solution. Surgery must be performed with the complete resection of elephantiatic skin, with penile and scrotal reconstruction, with attentive infection control and volume management. The presented cases demonstrate how meticulous examination, profound treatment planning, and close collaboration with plastic surgeons, dermatologists, and anaesthesiologist guarantee short- and long-term success.
References
- Anonymous (1830) Elephantiasis of the Scrotum and Labia Pudendi. Med Chir Rev 12: 505-509.
- Shaitelman SF, Cromwell KD, Rasmussen JC, Stout NL, Armer JM, et al. (2015) Recent progress in cancer-related lymphedema treatment and prevention. CA Cancer J Clin 65: 55-81.
- Dandapat MC, Mohapatro SK, Patro SK (1985) Elephantiasis of the penis and scrotum. A review of 350 cases. Am J Surg 149: 686-690.
- Geshere Oli G, Tekola Ayele F, Petros B (2012) Parasitological, serological and clinical evidence for high prevalence of podoconiosis (non-filarial elephantiasis) in Midakegn district, central Ethiopia. Trop Med Int Health 17: 722-726.
- Abraham G, Blake PG, Mathews R, Bargman JM, Izatt S, et al. (1990) Genital swell- ing as a surgical complication of continuous ambulatory peri- toneal dialysis. Surg Gynecol Obstet 170: 306-308.
- Porter W, Bunker C (2001) Chronic penile lymphedema: a report of 6 cases. Arch Dermatol 137: 1108-1110.
- Champaneria MC, Workman A, Kao H, Ray AO, Hill M (2013) Reconstruction of massive localised lymphoedema of the scrotum with a novel fasciocutaneous flap: A rare case presentation and a review of the literature. J Plast Reconstr Aesthet Surg 66: 281-286.
- Mehrara BJ, Greene AK (2014) Lymphedema and obesity: Is there a link? Plast Reconstr Surg 134: 154e-160e.
- Singh V, Sinha RJ, Sankhwar SN, Kumar V (2011) Reconstructive surgery for penoscrotal filarial lymphedema: A decade of experience and follow-up. Urology 77: 1228-12231.
- Malloy TR, Wein AJ, Gross P (1983) Scrotal and penile lymphedema: Surgical considerations and management. J Urol 130: 263-265.
Citation: Romics M, Jósvay J, Regőczi T, Nyirády P (2019) About Non-infectious Scrotal Elephantiasis: 5 Cases with Management Algorithm. J Obes Weight Loss Ther 9:392. DOI: 10.4172/2165-7904.1000392
Copyright: © 2019 Romics M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 11388
- [From(publication date): 0-2019 - Feb 20, 2026]
- Breakdown by view type
- HTML page views: 10105
- PDF downloads: 1283