An Algorithm for CSF Leak Management in a Spectrum of Temporal Bone Pathologies
Received: 19-Apr-2018 / Accepted Date: 11-May-2018 / Published Date: 18-May-2018 DOI: 10.4172/2161-119X.1000348
Abstract
Introduction: A wide spectrum of temporal bone pathology can present with cerebrospinal fluid (CSF) leak. This originates from the defects in the temporal bone that can be spontaneous, traumatic, pathological and iatrogenic. Most common routes are from labyrinthine window dehiscence, along fracture lines, via inner ear malformations or by direct dural invasion due to middle ear pathology. Complications of CSF leak include otogenic meningitis, temporal lobe abscess and otic hydrocephalus.
Methods: This is a case review of three interesting patients, who presented with varied etiology of CSF leaks. Their complex pathology and the rationale in management of CSF leaks are highlighted. Case 1: Post road traffic accident (RTA) bilateral temporal bone fracture with unilateral CSF otorhinorrhea with total facial palsy with profound Sensorineural hearing loss (SNHL). Case 2: Petrous cholesteatoma recurring in a previous mastoid cavity with large tegmen and dural erosion, fungus cerbri and CSF leak. Case 3: Adolescent girl with unilateral cochleovestibular dysplasia presenting with recurrent meningitis due to spontaneous CSF otorhinorrhea.
Results: All patients had successful repair of defects to achieve complete arrest of leak by following meticulous approach with a multi-layered closure and post-operative management with neuro monitoring. Based on our experience we recommend a standard protocol for CSF leak repair in the temporal bone.
Conclusion: CSF otorrhea is a rare entity. Diagnosis is suspected through otorrhea, aural fullness, hearing loss and radiological investigations. Surgery is successful when managed at a tertiary referral centre having an experienced skull base team, using a protocol as suggested here.
Keywords: Skull base defect; Cerebrospinal fluid otorrhea; Transmastoid approach; Multi-layered closure; Algorithm
Introduction
Cerebrospinal fluid (CSF) leakage is a life-threatening condition, requires thorough and timely intervention. It most commonly occurs as a result of trauma and iatrogenic injury, although infectious and neoplastic etiologies are also possible. Spontaneous CSF leaks are due to congenital defects and typically occur in 2 distinct populations: young children and middle-aged adults [1]. Recognition of the source of the leakage and its appropriate treatment are necessary to avoid rhinorrhoea or otorrhea, low-pressure headaches and meningitis, which are known complications of CSF leak. Large size of the defect or an increased intracranial pressure can lead to CSF leak or slow development of a brain hernia into the middle ear [2]. CSF leak occurs when there is a breach of the arachnoid membrane, dura mater, bone and mucosal lining of the mastoid and middle ear. To complete the route of egress there must be a defect in the external auditory canal or perforation of the tympanic membrane. If this defect is not present, CSF, once in the middle ear cleft, can flow down the eustachian tube and present as otorhinorrhoea/ paradoxical CSF rhinorrhea CSF leaks can have a wide etiology and can be broadly classified (Table 1) [3].
| Non-traumatic | Traumatic |
|---|---|
| Spontaneous otorrhea | Trauma (blunt or penetrating) |
| Middle ear disease, extensive cholesteatoma | Iatrogenic otorrhea |
| Neoplastic otorrhea | Post irradiation otorrhea |
| Miscellaneous causes |
Table 1: Etiology of CSF otorrhea.
Detection of CSF leaks is by taking a detailed clinical history and performing a full otorhinolaryngologic and neurologic examination. Otomicroscopy is done to check for signs of trauma, spontaneous discharge. In cases of intact tympanic membrane, diagnostic nasal endoscopy is done to rule out CSF otorhinorrhoea. Audiometry for assessing the hearing and ossicular status. Radiological investigations include HRCT temporal bone (Axial and coronal cuts) and an MRI-T2 MRI for CSF flow. Cisternography is an optional investigation in case of suspected leaks.
Our Case Series
Case 1
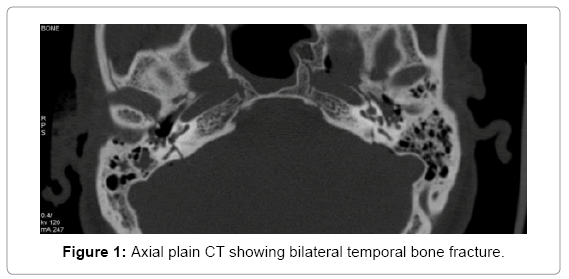
A 23 years young male presented with complaints of watery discharge from left side of nose with bilateral profound hearing loss and right side facial weakness. He had sustained an injury due to road traffic accident (RTA) and had bleeding from the left ear. He had been hospitalized for 8 days elsewhere and started on anti-convulsants, before presenting to our hospital 18 days later. Otomicroscopic examination showed bilateral haemotympanum. On tuning fork tests, no sound was perceived by the patient. There was a House Brackmann grade V facial palsy on the right side. Other cranial nerve examination was normal. Diagnostic nasal endoscopic examination showed clear fluid in the left nasopharynx. CT temporal bones (Figure 1) revealed fractures of the occipital bone extending across the foramen magnum into both temporal bones, involving the right vestibule, lateral semi-circular canal, middle ear cavity and the left cochlea. The fracture was found to traverse the right horizontal facial nerve canal and the left internal auditory canal. The facture line of the left temporal bone was found to be passing through the cochlea and modiolus. Pure tone audiometry (PTA) revealed bilateral profound sensori-neural hearing loss.
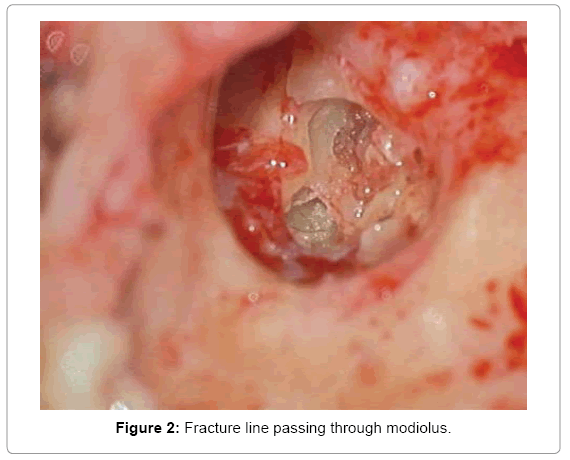
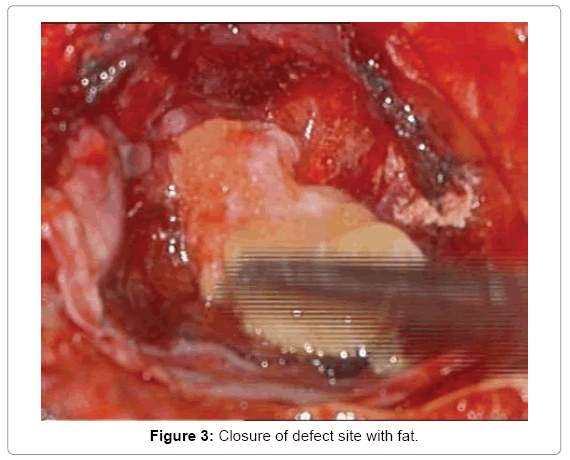
The patient underwent left CSF otorrhea repair, 20 days after the RTA, as the CSF leak was active and not responding to conservative management, in order to prevent meningitis. Transcochlear approach was used to seal the leak. Intra-operatively, transverse fracture line was identified passing through the cochlea (Figure 2). Active CSF leak was seen from the round and oval window. Leak was repaired with temporalis muscle, fascia, fascia latae and fibrin glue. Eustachian tube was plugged with muscle and blind sac closure done (Figure 3).
Case 2
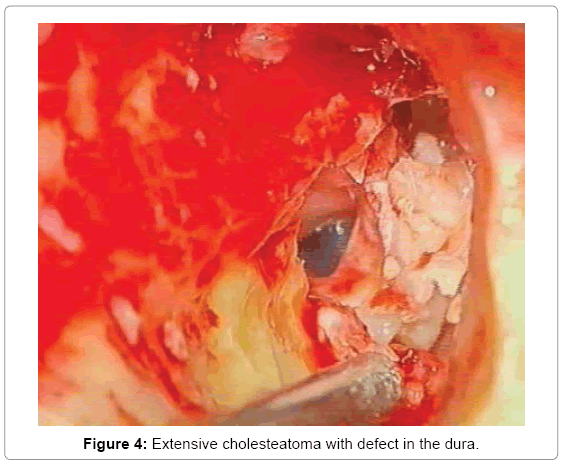
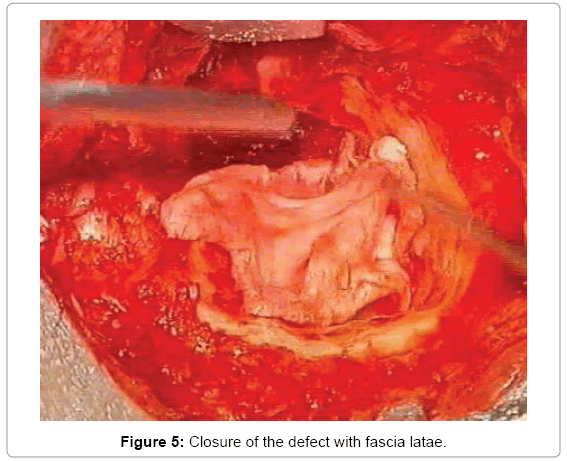
77 years old gentlemen, had presented with complaints of left ear discharge, low grade tinnitus, headache in the left temporal region, intermittent giddiness and hard of hearing on left side. He had history of left ear surgery, four times in the past, for similar complaints. On examination, patient had post aural scar with intact previous blind sac closure. On tuning fork tests, no sound was perceived by the patient, on left side. Facial symmetry was maintained. Right ear examination was normal. Radiological investigations showed soft tissue mass within middle ear cavity, extending into left external auditory canal with bony erosion of attic walls. Erosion of tegmen, all three semi-circular canals, facial nerve and posterior fossa dura were noted on scans. PTA showed left profound sensorineural hearing loss (SNHL). Transmastoid approach was followed. Cholesteatoma seen filling the tympanic cavity, mastoid cavity and extending into the dura. Dural rent was noted in the tegmen (Figure 4). CSF leak was noted from same site. Facial nerve was partially eroded in the horizontal segment. Multi layered leak repair done (Figure 5). Blind sac closure and pressure dressing.
Case 3
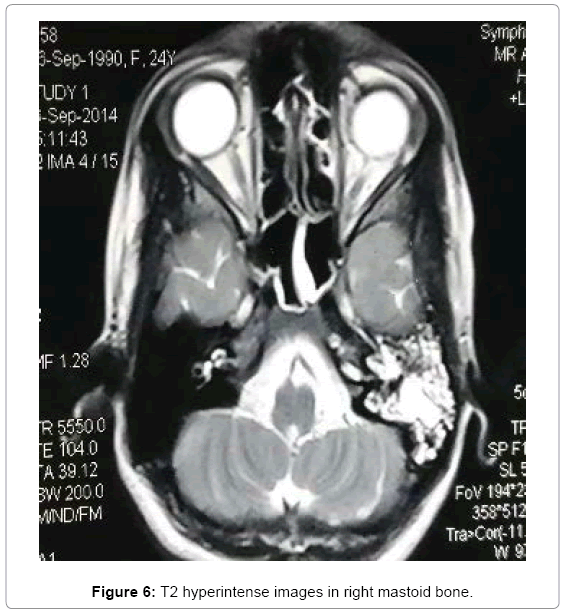
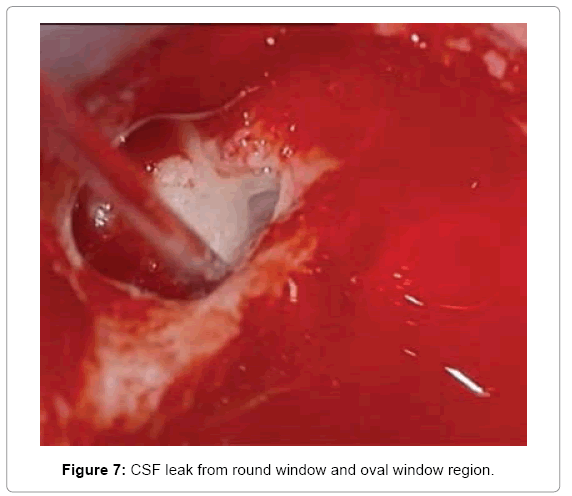
23 years young lady presented with continuous watery discharge from left ear for the past 3 years associated with headache. She had multiple episodes of meningitis in 2014-2015 and severe hard of hearing on left side. She underwent mastoid cavity closure with bone patty for CSF leak, elsewhere. She was started on anti-tuberculous treatment and had finished the course, before presenting at our hospital. There was no history of trauma, ear infections in the past. On examination, she had spontaneous watery discharge from left ear. Post aural scar was noted. Patient had neck rigidity. On lumbar puncture CSF was found to be turbid and cell counts were high. Subsequently, patient was started on intravenous antibiotics. Once the cell counts were normal and the meningeal signs were negative, patient was taken up for surgery. Radiological investigations showed left cochleo-vestibular dysplasia (IP-II Mondini deformity) with dehiscence of labyrinthine part of facial nerve. T2 MRI showed hyperintensity in mastoid and middle ear, suggestive of fluid (CSF) collection (Figure 6). CT Cisternography showed leak around oval and round window. Pure tone audiogram showed left profound SNHL. Transotic approach was used to arrest the spontaneous CSF leak. Partially dehiscent stapes foot plate was noticed.
CSF leak was visualized in superior aspect of oval window and round window (Figure 7). Cochlea was drilled and multilayered packing done. Eustachian tube was plugged. Leak was sealed with fibrin glue followed by blind sac closure.
All of our cases as describe above underwent retro auricular transmastoid approach followed by opening of the cochlea or labyrinth depending in the site of the leak. Initial steps of the surgery include examination of external auditory canal and status of tympanic membrane followed by a retroauricular approach to open the mastoid by using ‘C’ shaped incision. Anterior based palva flap was taken in all the cases, which was helpful in covering the surgical site before the skin closure. Mastoid was opened with the keen vision on the tegmen area to identify the site of the leak. The sino dural angle was thinned out in all our cases for better exposure. In case of chronic otitis media, eradication of the disease is must before we proceed further. After the bone work is complete and the pathology is removed, the bone defect is exposed. The operative field is then rinsed with an antibiotic solution. Canal wall was lowered in all our cases, since the site of leak was either in the labyrinth or posterior fossa. Ossicular chain status is noted. Site of leak is identified and also examined for fracture lines and herniated tissue if present. If the site of the leak is not obvious, it is confirmed by Valsalva maneuver (intra op, by bag ventilation). It’s preferable to do a blind sac closure and eustachian tube plugging in all the cases, to prevent secondary infection. The herniated tissue is reduced into intracranial compartment and bony defect is closed. Cavity was sealed by multi-layer technique using fat, tissue glue, temporalis fascia and tensor fascia latae. Wound was closed by continuous interlocking sutures and a tight mastoid dressing.
All the above three patients were given 3rd generation IV cephalasporins in the post-operative period with mannitol, analgesics, laxatives and Diamox. Prophylactic anti-convulsant was given for case 2 patient. All had post aural suture removal on postoperative day 10, followed by regular post op follow up. 2nd follow up was after 2 weeks, as there is a chance for CSF to build up pressure in 2 weeks. Later they were reviewed monthly once for next 6 months followed by once in 6 months. post-operative MRI for CSF flow analysis can be done 2 weeks later in case of suspicious collection of CSF in the cavity, where in patients presents with symptoms of headache and ear pain. Case 1 and Case 2 were symptomatically better till 1 year post surgery follow up. Patient with spontaneous CSF leak (case 3) presented with headache on the 2nd follow up visit. CSF flow analysis MRI was normal and lumbar puncture had normal pressure. She was treated with oral analgesics and symptoms improved over time. None of them had recurrence of leak/ ear discharge.
Discussion
Spontaneous CSF leaks presenting during childhood are usually caused by developmental anomalies of the labyrinth such as mondinitype defect or widely patent vestibular and cochlear aqueducts that allow outflow through the oval or round window. Microdehiscences of the temporal bone are seen with patent fallopian canal, defects in the tympanomeningeal fissure of Hyrtl and petromastoid canal related to the subarcuate artery [4]. Spontaneous leaks during childhood can present late in the adulthood due to focal atrophy by normal CSF pressure pulse causing bony erosion, thinning of dura with age. Hearing loss and a sensation of fullness in the ear suggestive of secretory otitis media are the usual symptoms to present with. Presence of high signal within the middle ear cavity on T2-weighted images and low signal on T1-weighted spin echo images of MRI indicate the presence of CSF leak. Second major sub type of spontaneous CSF leak occurs in adults, where the defect can be found in middle cranial fossa or posterior cranial fossa. Patients present either as serous otitis media or in case of intact tympanic membrane, they present as paradoxical CSF rhinorrhea [5]. Surgical intervention is the primary treatment for congenital and spontaneous CSF leak. Transmastoid approach offers access to the posterior fossa and posterior tegmental defects with low risks and complications. Defects that are large, multiple, or recurrent are best addressed by a combined transmastoid and middle fossa approach [2].
Temporal bone fractures occur in approximately 14-22% of all skull injuries. Most of these fractures are unilateral, with bilateral fractures reported in 9% to 20%. Children account for 8-22% of patients with temporal bone fractures. The otic capsule is spared in 90% and is involved in 10%. Common sequelae of temporal bone fractures include tympanic membrane perforation, facial nerve palsy, damage to cochleovestibular apparatus causing sensori-neural hearing loss, conductive hearing loss due to ossicular disruption, tinnitus, vertigo, CSF leak, perilymph fistula, post traumatic endolymphatic hydrops, cholesteatoma, meningocele/encephalocele, meningitis, injuries to lower cranial nerves, vascular injuries i.e. injuries to internal carotid artery and sigmoid sinus [6]. Otic capsule sparing fractures are much more common (>90%) than otic capsule involving and the latter is associated with higher incidence of facial nerve injury (30-50%), SNHL and CSF leak (2-4 times higher than otic capsule sparing). Patients with an otic capsule–violating fracture, are approximately twice as likely to develop facial paralysis, four times as likely to develop cerebrospinal leak, seven times as likely to experience profound hearing loss and more likely to sustain intracranial complications, such as epidural hematoma and subarachnoid haemorrhage, than those with an otic capsule– sparing fracture [7]. While high resolution computed tomography is the standard for evaluating temporal bone fractures, MRI is useful for revealing temporal lobe injuries.
CSF leak occurs in 15-20% of all temporal bone fractures. Fractures involving the otic capsule are associated with higher incidence of CSF leak. Management of cerebrospinal fluid leak begins with conservative measures including bed rest with head elevation, stool softeners, avoidance of nose blowing/sneezing and other forms of straining and, in selected patients, placement of a lumbar drain. Spontaneous resolution with this conservative management occurs in 95% to 100% of patients.
Surgical repair is recommended for those cases that persist 7-10 days after an injury [8]. The method of surgical closure of CSF fistulas after temporal bone fractures depends on the location of the fistula, hearing status of both ears, presence of brain herniation through the tegmen and patency of the external canal.
Chronic otitis media with cholesteatoma has the potential to thin out the dura, which can lead to the formation of meningocele or meningoencephaolocele or temporal lobe herniation. Meningoencephaloceles of the temporal bone is rare and may be misdiagnosed. Autopsy study suggests that 15-34% contain single defect in tegmen of temporal bone [9]. The brain tissue usually becomes necrotic after herniation. These cases tend to develop intra op CSF otorrhea.
Management
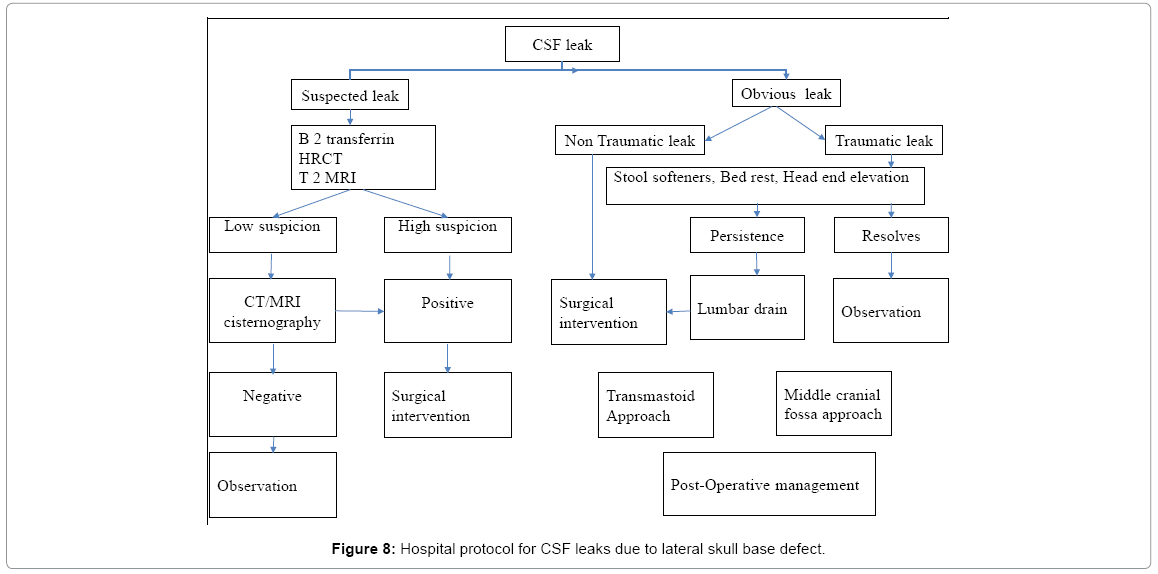
CSF leaks are often challenging to diagnose and manage. Patients typically present with complaints of aural fullness, hearing loss, pulsatile tinnitus, with a unilateral persistent or recurrent middle ear effusion along with post-nasal drip or unilateral watery rhinorrhoea. Clinical presentations may be subtle and may be present for years. The diagnosis ultimately depends on a high degree of clinical suspicion and is sometimes made after myringotomy or tympanostomy tube placement and presenting with persistent clear otorrhea. Investigations available to facilitate the diagnosis include ear discharge biochemistry, beta 2 transferrin assay/Tau-protein analysis [10]. Otoendoscopy and nasal endoscopy to be done when required. B2-transferrin protein is produced by neuraminidase activity in the brain and is unique to CSF, perilymph and aqueous humor. It is detected by immunofixation and silver staining or by immunoblotting [3]. Radiological investigations include, high resolution CT scans for bony landmarks, MRI scan, preferably T2 weighted scan. Low suspicion on radiology can be confirmed by cisternography. The only management for spontaneous leaks is to operate and close the CSF leak site. CSF otorrhea due to trauma (non-iatrogenic trauma), can be initially managed conservatively by bed rests, head end elevation, laxatives and medications to decrease intra-cranial pressure. Prophylactic lumbar drain can be used in traumatic CSF leaks to decrease intra-cranial pressure [11]. Persistence of otorrhea for more than 7 days is associated with a significantly increased risk of meningitis. And traumatic leaks should be taken up for surgery, if the leak persists for more than 7 days, after the start of conservative management [3].
Principles of Surgery
Surgical repair should address the osseous and dural defects and underlying intracranial benign hypertension. Without a secure bony reconstruction, dural herniation and/or fistulization can recur. Defect can be sealed with autologous, heterogenous or alloplastic material or their combination [12]. Kenning et al. [13] have reported the use of autologous calvarial bone, pericranium and intra-dural collagen grafts. All defects need to be repaired in a multilayered fashion using autologous tissue (cortical mastoid bone graft, temporalis fascia, temporalis muscle, conchal or septal cartilage, fascia lata, etc.) as well as allogenic materials (Gelfoam, Surgicel, Duragen, fat, tissue sealant, etc.). Alloplastic synthetic biomaterials like bone cements, bioglass ceramics, acrylic polymers, fluroplastic, composite hydroxyapetite bone paste with methyl methacrylate have also been reported in literature and mainly used as adjunct with bone grafting for larger defects resulting from trauma, surgery, neoplasm and for recurrent defects [1]. Multilayered approach offers better results with less recurrence rates. The optimal placement of the autologous material between the dura and bony tegmen defect margins, in an extra-dural intra-cranial fashion, is critical in stabilizing and securing the repair [14]. Dural defects can be closed primarily and/or bolstered using free autologous tissue, dural substitutes or pedicled local flaps such as the temporo-parietal flap which also provides nutrition and vascularity to the repaired dural defect. Tissue sealant may be critical in the initial post-operative period in preventing leakage of CSF. Intra-operative CSF drainage with a lumbar drain is needed in larger defects of the skull base or in obese patients with raised intracranial pressure and those with significant medical co-morbidities and anesthetic risks [15].
Kenning et al. [13] proposed in their treatment paradigm that after tegmen repair, to prevent recurrence of leak, a ventriculoperitoneal shunting should be considered for patients with any combination of the following high-risk factors-spontaneous CSF leak causing high-volume leaks or high CSF opening pressure and impairment of CSF absorption like meningitis, intracranial hemorrhage, significant closed head injury, etc.
Selection of Surgical Approach
Surgical approaches include transmastoid, middle cranial fossa approach and combined approach [16]. The middle cranial fossa approach offers a direct route and improved exposure of the entire tegmen and petrous apex from above and potentially less trauma to the ossicles. However, the middle fossa craniotomy approach is associated with greater morbidity and the risk of neurological complications. The transmastoid approach avoids these complications that may occur secondary to temporal lobe retraction, but potential disadvantages here include decreased exposure of the defect, lower initial success rate and increased risk of hearing loss. Conductive hearing loss in these cases is secondary to the CSF effusion and sometimes due to an encephalocele abutting the ossicular chain [12]. Many neurootologists recommend a combined transmastoid-middle fossa approach, especially in cases of large, multiple, or medial defects, or revision surgery for recurrent CSF leaks [17].
Proposed hospital algorithm for managing cases with cerebrospinal fluid leaks due to temporal bone pathologies (Figure 8).
Transmastoid approach
This is a simple and direct way to the lateral cranial base and can address defects in both the middle and posterior fossae with minimal morbidity (Table 2) [18].
| Advantages | Disadvantages |
|---|---|
| Easy to perform | Removing ossicles for anterior tegmen defects, can compromise hearing |
| Safe procedure with fewer risks and complications | Not ideal for large meningoencephaloceles or multiple CSF leaks |
| Ideal approach for posterior fossa defects | Recurrence may need cavity obliteration with blind sac closure |
Table 2: Trans-mastoid approach to tegmen defect.
Middle fossa approach
The vast majority of spontaneous CSF leaks take place through the tegmen plate, rather than through a posterior fossa defect. Traumatic leaks are more unpredictable and many have both posterior fossa and middle fossa components. Better outcomes are achieved with defects sealed via the middle fossa approach to the tegmen plate when this is the site of the problem [18].
Combined trans-mastoid with middle fossa approach
The combined approach offers higher success rate than single approaches in recurrent or large defects. It is important to pay particular attention to exploring the tegmen via the mastoidectomy route, prior to placement of the middle fossa craniotomy for optimal access to the defect from both above and below [18].
Post-operative care with neuro-ICU monitoring is mandatory. Ample bed rest with head elevation and secure mastoid bandage, antibiotic cover, thrombo-embolic prophylaxis, avoidance of straining and sneezing, stool softeners and cough suppresants are all essential and help to prevent displacement of the graft. Persistent monitoring till second post-operative week is necessary, as the CSF builds up pressure within two weeks of closure [15].
Conclusion
Surgery for CSF leaks is challenging and needs multidisciplinary team input. A judicious choice of approach is necessary to achieve success. Literature has shown safe and reliable outcomes in recent times due to the improved precision in diagnostics, intra-operative navigational support, use of safer biomaterials for sealing defects, better post-operative neuro-care and long-term surveillance for recurrence. This type of surgery needs to be performed in high volume tertiary referral centres with skull base units, where all the expertise and infrastructure is available in their armamentarium to comprehensively manage this entity. All complications comprehensively manage this entity. All complications pre-operative and post-operative, like meningitis should be addressed. Multilayer repair with autologous materials and intensive post monitoring offers the best results.
References
- Goddard JC, Meyer T, Nguyen S, Lambert PR (2010) New considerations in the cause of spontaneous cerebrospinal fluid otorrhea. Otol Neurotol 31: 940-945.
- Leslie K, Clayton E, Edward ED (2014) Transmastoid approach to spontaneous temporal bone cerebrospinal fluid leaks: Hearing improvement and success of repair. Otolaryngol Head Neck Surg 150: 472-478.
- Christopher R (2005) Diagnosis and management of otologic cerebrospinal fluid leak. Otolaryngol Clin North Am 38: 5830-595.
- Jackler RK (2009) Fractures of the cranial base, encephalocele of the middle fossa floor, cerebrospinal fluid leak. In: Jackler RK (Eds.) Atlas of Skull Base Surgery and Neurotology. Thieme; New York, pp: 181-193.
- Lee YS, Ku CH, Park SY, Seo YJ (2015) Assessment and treatment of spontaneous temporal bone meningoencephalocele for hearing gain. Int J Otorhinolaryngol 2: 3.
- Natarajan K, Madhav K, Saraswathi AV, Kameswaran M (2018) Bilateral temporal bone fractures: A case report. Int J Otorhinolaryngol Head Neck Surg 4: 271-275.
- Dahiya R, Keller JD, Litofsky NS, Bankey PE, Bonassar LJ, et al. (1999) Temporal bone fractures: Otic capsule sparing versus otic capsule violating-clinical and radiographic considerations. J Trauma 47: 1079-1083.
- Brodie HA, Thompson TC (1997) Management of complications from 820 temporal bone fractures. Am J Otol 18: 188-197.
- Brown NE, Grundfast KM, Jabre A, Megerian CA, O’Malley BW Jr, et al. (2004) Diagnosis and management of spontaneous cerebral fluid middle ear effusion and otorrhoea. Laryngoscope 114: 800-805.
- Schlosser RJ, Woodworth BA, Wilensky EM, Grady MS, Bolger WE (2006) Spontaneous cerebrospinal fluid leaks: A variant of benign intracranial hypertension. Ann Otol Rhinol Laryngol 115: 495-500.
- Amit A, Nitish B, Deshmukh PT (2011) Combined middle cranial fossa and trans-mastoid approach for the management of post-mastoidectomy csf otorrhoea. Indian J Otolaryngol Head Neck Surg 63: S142–S146.
- Patel NS, Canopy E, Sheykholeslami K (2012) Transmastoid management of temporal bone tegmen defects, encephaloceles and CSF leaks. J Otol Rhinol 2: 1-5.
- Kenning TJ, Willcox TO, Artz GJ, Schiffmacher P, Farrell CJ, et al. (2012) Surgical management of temporal meningoencephaloceles, cerebrospinal fluid leaks and intracranial hypertension: Treatment paradigm and outcomes. Neurosurg Focus 32: 1-8.
- Zanetti D, Garavello W, Gaini L (2011) Transmastoid repair of temporal meningoencephaloceles and cerebrospinal fluid otorrhea. Otorhinolaryngol Clin Int J 3: 31-41.
- McCutcheon BA, Orosco RK, Chang DC, Salazar FR, Talamini MA, et al. (2013) Outcomes of isolated basilar skull fracture: Readmission, meningitis and cerebrospinal fluid leak. Otolaryngol Head Neck Surg 149: 931-939.
- Pelosi S, Bederson JB, Smouha EE (2010) Cerebrospinal fluid leaks of temporal bone origin: Selection of surgical approach. Skull Base 20: 253-259.
- Agrawal A, Baisakhiya N, Deshmukh PT (2011) Combined middle cranial fossa and trans-mastoid approach for the management of post-mastoidectomy CSF otorrhoea. Indian J Otolaryngol Head Neck Surg 63: S142-S146.
- Richard MI, Raghunandhan SK (2018) Surgical management of temporal bone meningoencephalocele and CSF leaks. J ENT Masterclass.
Citation: Madhav K, Kumar RS, Natarajan K, Anand Kumar RS, Kameswaran M (2018) An Algorithm for CSF Leak Management in a Spectrum of Temporal Bone Pathologies. Otolaryngol (Sunnyvale) 8: 348. DOI: 10.4172/2161-119X.1000348
Copyright: © 2018 Madhav K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 11254
- [From(publication date): 0-2018 - Dec 12, 2025]
- Breakdown by view type
- HTML page views: 10116
- PDF downloads: 1138