An Observational (Analytical) Retrospective cum Prospective Study of Cases of Endoscopic Sinus Surgery in Paediatric Population
Received: 15-Apr-2020 / Accepted Date: 22-Sep-2020 / Published Date: 29-Sep-2020 DOI: 10.4172/2161-119X.1000406
Abstract
Background: Sinus disease is a common source of morbidity for many children. Around 5-13% of all upper respiratory infections are complicated by secondary bacterial infection of the paranasal sinuses. Nasal mass in paediatric population is very rare which can be either congenital or acquired.Surgery in these conditions is challenging because of the risk of anaesthesia and a narrow nasal space.
Objectives
1. To study the etiology of disease of Paranasal sinuses in paediatric population requiring endoscopic sinus surgery.
2. To study intra-operative challenges while performing endoscopic sinus surgery in paediatric age group
Method: A retrospective cum prospective study of 30 pediatric patients (age ranging from 0 to 12 years old children) was conducted at our tertiary care centre from June 2016 to December 2018. After detailed imaging and clinical evaluation, all patients underwent endoscopic sinus surgery.
Result: In our study period, out of 30 patients, Dacryocystitis (total 6), Orbital cellulitis (total 6), Juvenile nasopharyngeal angiofibroma (total 6), and Antrochoanal polyp (total 5) constituted the majority. Three patients had Meningocoele and one each of Ossifying fibroma, Choanal Atresia, Sub periosteal hematoma and orbital floor fracture. All of them were treated endoscopically with good success rate. Only 2 patients had recurrence, which was managed endoscopically. Rest all were fine during follow-up.
Conclusion: Functional endoscopic sinus surgery is minimally invasive, so it is very feasible in paediatric population. A thorough knowledge of anatomy and basic experience in adult endoscopic sinus surgery is mandatory. There is a learning curve; as here, one needs to manipulate instruments within a narrow nasal cavity.
Keywords: Endoscopic; Paediatric; Sinus; Nasal mass; Dacryocystitis; Complication; Challenges; Micro instruments; Anatomy; Imaging
Introduction
Sinus disease is a common source of morbidity for many children. Around 5-13% of all upper respiratory infections are complicated by secondary bacterial infection of the paranasal sinuses. Nasal mass in paediatric population is very rare and can be either congenital or acquired.Young children, being unable to communicate some of the symptoms of sinusitis or nasal mass such as headache, nasal obstruction, and sinus pain/pressure, pose a challenge to clinician, who must rely on parental reporting of symptoms and physical findings to diagnose the condition. Functional endoscopic sinus surgery (FESS) differs in paediatric population. It is quite challenging in view of the size of anatomical landmarks, narrow nasal space in children and the risk of general anaesthesia. The prime need for an operating surgeon is a 3 dimensional concept of the region, which will allow him to approach and clear disease from the narrow recesses of the nose and paranasal sinuses and restore function to near normal. (1)The main goal of sinus surgery in paediatric population is to restore a physiologic pattern of ventilation and normal mucociliary clearance. It is recommended to preserve the normal anatomy and mucosa as much as possible. A detailed knowledge of the possible anatomical variations is essential in order to prevent complications.
Methods
The retrospective cum prospective study was approved by the institutional review board of King Edward Memorial hospital andSeth G.S. Medical College. It included 30 paediatric patients in the age group of infants to 12 years, presented during the time period from June 2016 to January 2018 with complaints of nasal blockage / obstruction, nasal discharge (mucoid / mucopurulent / purulent),bleeding from nose, recurrent rhinitis, loss / decrease / change in sense of smell, headache, Orbital swelling, Post traumatic visual complaint, watering from eyes. All of them underwent endonasal endoscopic approach for their complaints. The follow up period ranged from a minimum of 6 months to 2 years.
Preoperative EvaluationA detailed history regarding presenting complaints, past history and personal history were obtained. Special enquiries were made to rule out systemic illness, bleeding disorders and allergy. History of any previous surgery noted.All the patients were subjected to Computed tomography of Paranasal sinuses with or without contrast. In patients with nasal mass, MRI of paranasal sinuses and brain was done in addition to know the extent of the disease. CT scan provided a road map for surgery. After fitness for general anaesthesia and taking consent from the child’s guardian, an endoscopic approach was planned.
Preoperative Medical Treatment
The aim is to reduce inflammation and optimize the nasal mucosa to reduce bleeding during surgery. Patients were prepared with antibiotics and decongestants, and in case of polyposis, even preoperative steroids were given. Aspirin and other NSAIDs were stopped 2 weeks prior to surgery.
Surgical Technique
1. Nasal cavity was decongested using a mixture of lignocaine and adrenaline solution with close attention to weight based dosing (7mg/kg for 1%lignocaine with 1 in 1, 00,000 epinephrine) in small children. A diagnostic nasal endoscopy was performed. After meticulous decongestion, a 4mm endoscope was used for better visualization. Lamellar principle was used. 1st lamella- uncinate process was addressed. 2nd lamella-anterior ethmoids were cleared. 3rd lamella- ground lamella was entered, and posterior ethmoids were cleared. 4th lamella – anterior phase of sphenoid was opened.
2. The first step is to do an uncinectomy. An incision is made on the uncinate process, starting at the level of the upper attachment of the middle turbinate (axilla region) and ending just above the inferior turbinate. It is then removed with twisting movement to access the infundibulum. The ethmoidal bulla and hiatus semilunaris is exposed. It is important to keep in mind that the ethmoid cavity is narrow in paediatric population.
3. Care must be taken to prevent any injury to middle turbinate to avoid adhesions.
4. The anterior ethmoid cells are opened and cleared.
5. Following this, the maxillary ostium is inspected and widened.
6. Minimally invasive surgery is performed. Unnecessary dissection is avoided. The sinuses and areasthatare not involved are left untouched.
7. This minimal surgery greatly improves the function of the osteomeatal complex and provides good ventilation of the maxillary, ethmoid and frontal sinuses.
8. Postoperatively, a piece of merocel is used as a tamponade.
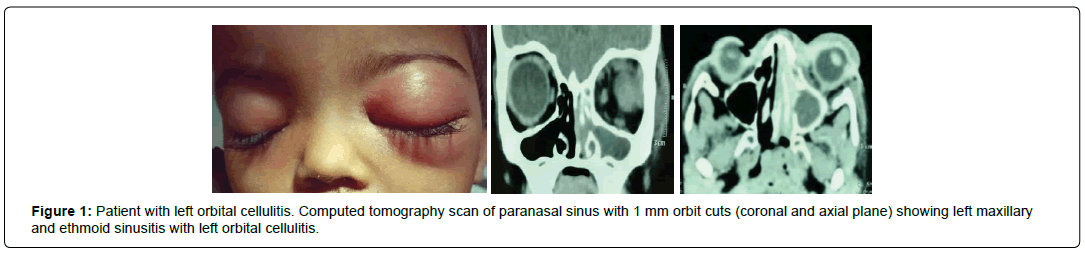
We had six patients with complicated acute sinusitis. There were four males and two female patients in the age group ranging between 6 months to 5 years. All of them presented with periorbital swelling. On enquiry, they had history of severe rhinitis. All patients underwent computed tomography scan of paranasal sinus (plain + contrast) with 1mm orbit cuts to know the extent of disease process.These patients were initially treated with a course of intravenous antibiotics and followed by endoscopic sinus surgery. Uncinectomy was done. The maxillary sinus ostium widened. Anterior ethmoid cells were cleared. Most patients had pus within maxillary sinus which was drained for culture and sensitivity to start appropriate antibiotics. If there was breach in lamina papyracea, it was delineated. All patients were given intravenous antibiotics postoperatively. They were kept under weekly follow-up for a period of one month and then followed up monthly for three months (Figure 1).
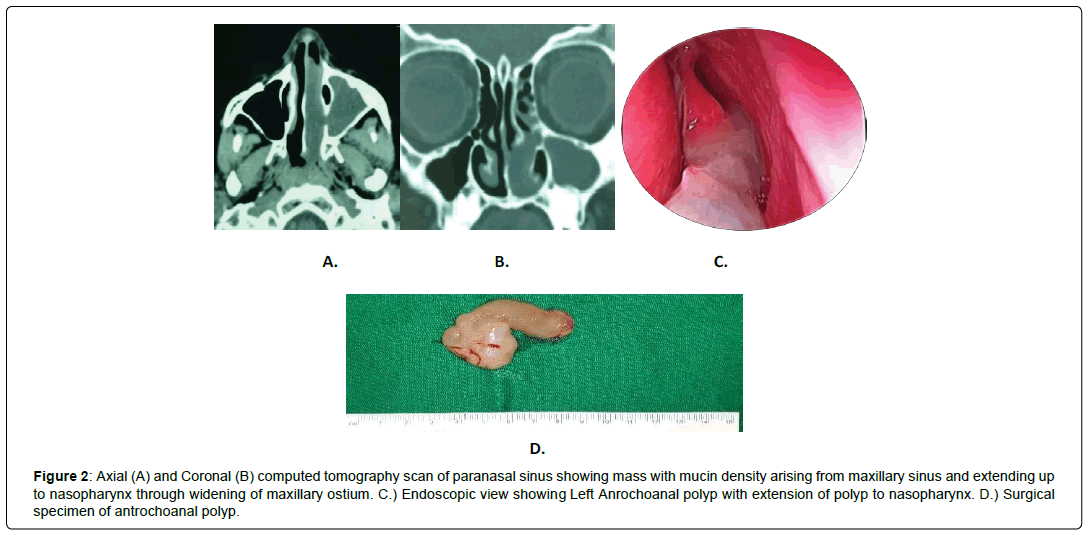
There were five patients with antrochoanal polyp, three male and two female patients (aged 8 years to 11 years). Clinically all had complaints of unilateral nasal obstruction with mucopurulent nasal discharge. A computed tomography scan of paranasal sinus was done preoperatively. Besides 00 degree endoscope, we used angled nasal endoscope (300,450 or 700 degree) to delineate the attachment of polyp from maxillary sinus wall. After uncinectomy, natural ostium of maxillary sinus was widened using ostrum backbiting forceps. Antrochoanal polyp was separated from its attachment from maxillary wall using curved blakesley forcep and delivered transorally. Care was taken to prevent injury to healthy nasal mucosa. Surgical specimen was sent for histopathology examination. Intranasal merocel pack was kept for 48 hours. Of the five patients, only one had recurrence that was managed with revision endoscopic sinus surgery wherein the site of attachment of polyp was found to be at the anterolateral wall of maxilla (Figure 2).
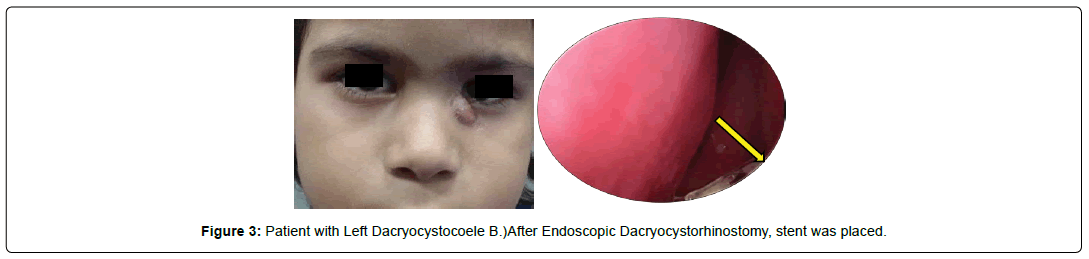
We had six patients of acute dacryocystitis (three male and three female patients, age ranging 1 year to 8 years), all of whom were subjected to endonasal endoscopic dacryocystorhinostomy (DCR). Besides routine blood investigations, ophthalmologic assessment was done. Patients with dacryocystitis were subjected to forced syringing under general anaesthesia with the hope that the block would open up. During forced syringing, the opposite punctum was closed using punctum dilator. After taking incision 3 to 4 mm anterior to uncinate process using insulated 450 ball probe (used in otology surgery) with a monopolar cautery,a posteriorly based flap is elevated. We used a small 1 mm Kerrison’s bone punch to expose the sac by making a wide bone window which is easier to make in children due to a thin bone lacrimal. The sac is exposed. Incision is taken over lacrimal sac and pus is drained out.We use a silastic stent in most of our patients who are over 3 years of age and those who present with a chronic dacryocystocoele. In those with acute symptoms, we avoid using a stent due to fear of creating a false passage. In such patients, we use topical mitomycin instead. Post procedure sac syringing showed free flow into nasal cavity. The parents are instructed to perform local irrigation of the nasal cavity with a saline solution nasal spray to prevent crusting around the stent. Topical antibiotic-steroid eye drops are prescribed for 10 days along with systemic antibiotics. All patients were asymptomatic during their follow up. The patients were followed up at end of 1 week and thereafter at the end of one month and three months.After three months stent was removed endoscopically under general anaesthesia. In our study only one patient had recurrence. She had a congenital abnormality of nasolacrimal duct and during the initial procedure, stent was not kept. She was managed with revision endoscopic procedure and a stent was placed which was removed after 3 months (Figure 3).
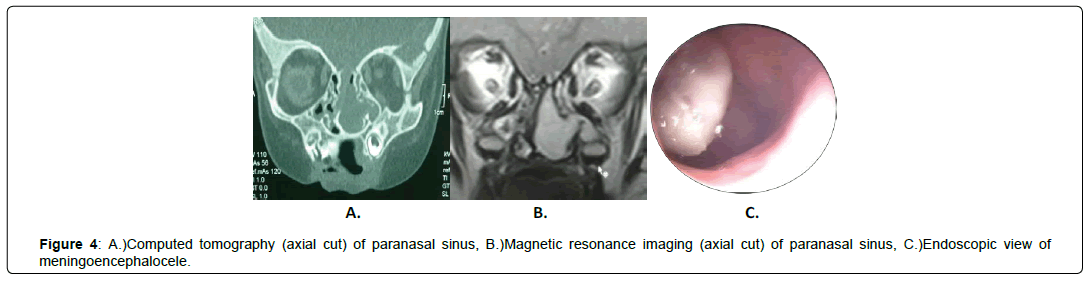
We operated on three patients of meningocoele and meningoencephalocoele (two female and one male), age ranging 1 month to 7 years, without any neurological deficit. All patients were managed successfully by endoscopic technique. Two of the patients showed defect at medial lamella of cribriform plate and one had defect lateral to middle turbinate on MRI. (Figure 4). The main challenge encountered was to operate in a narrow space. To overcome this, otological instruments like crocodile forcep, bellucci scissor, insulated ball probe and malleus head nipper were used. Endoscopy revealed the mass coming from the defect in cribriform plate. The base of the mass was cauterized with bipolar diathermy and meningocoele was excised. Septal cartilage,tensor fascia lata and fat were used to fill the defect. Tissue glue was used to seal it. There was no cerebrospinal fluid (CSF) leak intraoperative and postoperatively. Small sized merocel was kept in the nasal cavity for five to seven days as a tamponade to support the repair. Strict bed rest and precautions to not undergo any strenuous activity including avoiding nose blowing, avoiding straining during stools and coughing for a month was advised. Postoperatively intravenous antibiotics were given for a period of 15 days. Patients were given stool softeners and cough suppressants. All patients were followed up and there were no complaints of recurrence.
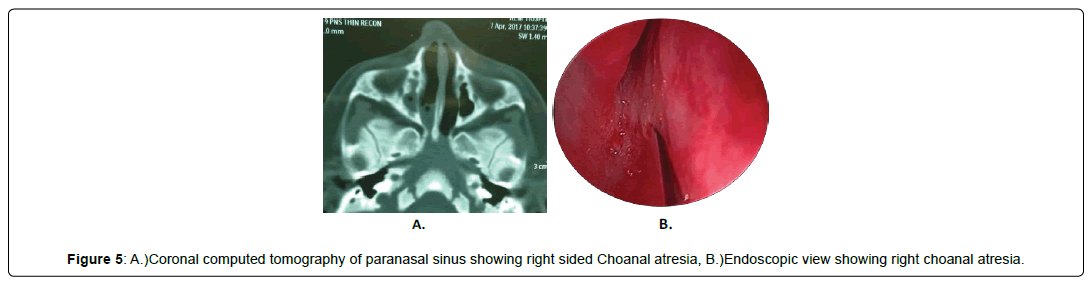
We had one case of membranous choanal atresia. She was a 10 month old female child with history of recurrent right sided nasal discharge and obstruction. There were no associated congenital anomaly. Computed tomography of paranasal sinus was suggestive of right sided membranous choanal atresia. She was managed by endonasal endoscopic surgery. Hopkins zero degree endoscope was used. To deal with narrow nasal space during surgery, otology instruments were used. After making an opening in choana, posterior septectomy was done by using insulated ball probe and malleus head nipper .Use of stent was avoided to prevent formation of granulations. Malleus head nipper was used instead of bone punch. During the entire procedure, care was taken to avoid injury to mucosa and reduce the chance of restenosis. Postoperatively, child was stable and air blast was good on cold spatula test.
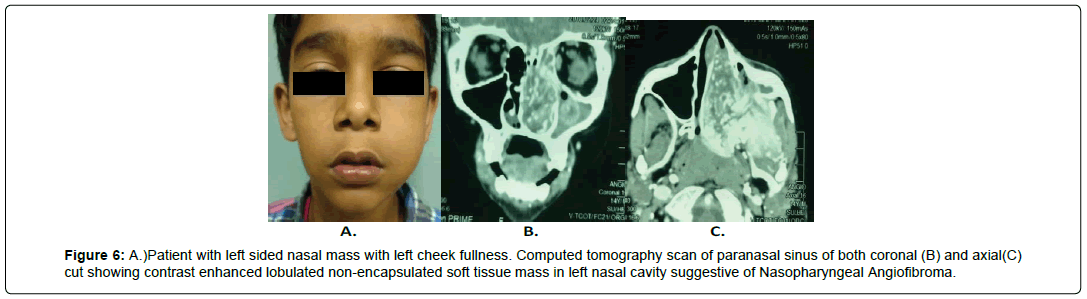
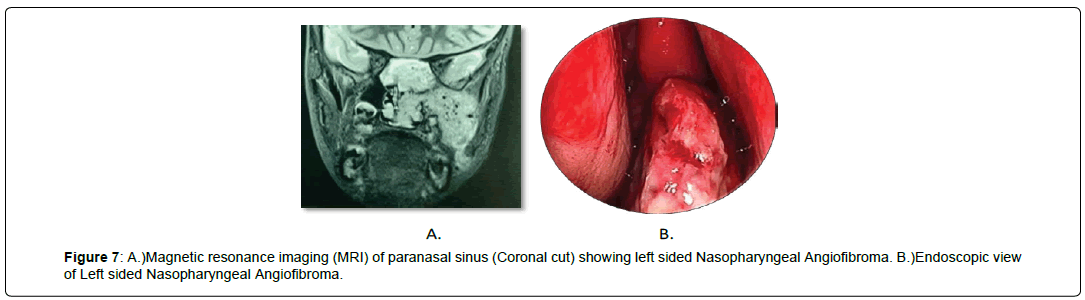
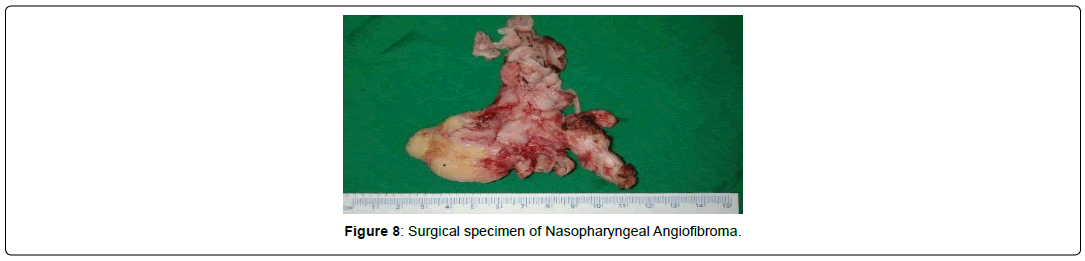
We had six patients of juvenile nasopharyngeal angiofibroma (male aged 10 to 12 years) who were managed endoscopically. Preoperatively, computed tomography scan of paranasal sinus (plain+ contrast) was done for all patients. Magnetic resonance imaging of paranasal sinus was advised for patients with intracranial extension of juvenile nasopharyngeal angiofibroma. Three of the patients were in stage II, two were in stage III and one was in stage IV (modified Andrew Fisch classification). All of them underwent preoperative embolization procedure. The minimum interval between embolization and surgery was 48 hours .Blood grouping and cross matching was done for all patients. The first step of surgery was uncinectomy. Middle turbinate was truncated to obtain better space. Natural ostium of maxillary sinus was widened. The posterior wall of maxillary sinus was removed with the help of Bone punch. Pterygopalatine fossa was then exposed and the lateral extension of tumour was identified. After exposure of tumour it was separated from sphenoid sinus, nasopharynx and pterygoid plate. Intraoperative bleeding was controlled by bipolar cauterization. Most tumours were delivered intraorally in toto and sent for histopathology examination. Intranasal pack was kept for 48 hours. Regular nasal douching was advised at the time of discharge. One patient (aged 12 years) had stage IV nasopharyngeal angiofibroma (with extension into cavernous area) that was managed endoscopically. This patient was subjected to balloon occlusion test and embolization. In this patient, intraoperative bleeding was more, as the tumour was supplied by contralateral ophthalmic division of internal carotid artery and he required two units of blood transfusion. There were no postoperative complications. During follow up, diagnostic nasal endoscopy was done in each patient for postoperative cleaning. There was no recurrence in any patient. They were subjected to postoperative computed tomography of paranasal sinus (plain + contrast) at the end of three months.
We operated on three patients of meningocoele and meningoencephalocoele (two female and one male), age ranging 1 month to 7 years, without any neurological deficit. All patients were managed successfully by endoscopic technique. Two of the patients showed defect at medial lamella of cribriform plate and one had defect lateral to middle turbinate on MRI. The main challenge encountered was to operate in a narrow space. To overcome this, otological instruments like crocodile forcep, bellucci scissor, insulated ball probe and malleus head nipper were used. Endoscopy revealed the mass coming from the defect in cribriform plate. The base of the mass was cauterized with bipolar diathermy and meningocoele was excised. Septal cartilage,tensor fascia lata and fat were used to fill the defect. Tissue glue was used to seal it. There was no cerebrospinal fluid (CSF) leak intraoperative and postoperatively. Small sized merocel was kept in the nasal cavity for five to seven days as a tamponade to support the repair. Strict bed rest and precautions to not undergo any strenuous activity including avoiding nose blowing, avoiding straining during stools and coughing for a month was advised. Postoperatively intravenous antibiotics were given for a period of 15 days. Patients were given stool softeners and cough suppressants. All patients were followed up and there were no complaints of recurrence (Figure 4).
We had one case of membranous choanal atresia. She was a 10 month old female child with history of recurrent right sided nasal discharge and obstruction. There were no associated congenital anomaly. Computed tomography of paranasal sinus was suggestive of right sided membranous choanal atresia. She was managed by endonasal endoscopic surgery. Hopkins zero degree endoscope was used. To deal with narrow nasal space during surgery, otology instruments were used. After making an opening in choana, posterior septectomy was done by using insulated ball probe and malleus head nipper .Use of stent was avoided to prevent formation of granulations. Malleus head nipper was used instead of bone punch. During the entire procedure, care was taken to avoid injury to mucosa and reduce the chance of restenosis. Postoperatively, child was stable and air blast was good on cold spatula test (Figure 5).
We had six patients of juvenile nasopharyngeal angiofibroma (male aged 10 to 12 years) who were managed endoscopically. Preoperatively, computed tomography scan of paranasal sinus (plain+ contrast) was done for all patients. (Figure 6).
Magnetic resonance imaging of paranasal sinus was advised for patients with intracranial extension of juvenile nasopharyngeal angiofibroma. Three of the patients were in stage II, two were in stage III and one was in stage IV (modified Andrew Fisch classification). All of them underwent preoperative embolization procedure. The minimum interval between embolization and surgery was 48 hours .Blood grouping and cross matching was done for all patients. The first step of surgery was uncinectomy. Middle turbinate was truncated to obtain better space. Natural ostium of maxillary sinus was widened. The posterior wall of maxillary sinus was removed with the help of Bone punch. Pterygopalatine fossa was then exposed and the lateral extension of tumour was identified. After exposure of tumour it was separated from sphenoid sinus, nasopharynx and pterygoid plate. Intraoperative bleeding was controlled by bipolar cauterization. Most tumours were delivered intraorally in toto and sent for histopathology examination. Intranasal pack was kept for 48 hours. Regular nasal douching was advised at the time of discharge.One patient (aged 12 years) had stage IV nasopharyngeal angiofibroma (with extension into cavernous area) that was managed endoscopically. This patient was subjected to balloon occlusion test and embolization. In this patient, intraoperative bleeding was more, as the tumour was supplied by contralateral ophthalmic division of internal carotid artery and he required two units of blood transfusion. There were no postoperative complications. During follow up, diagnostic nasal endoscopy was done in each patient for postoperative cleaning. There was no recurrence in any patient. They were subjected to postoperative computed tomography of paranasal sinus (plain + contrast) at the end of three months (Figure 7-8).
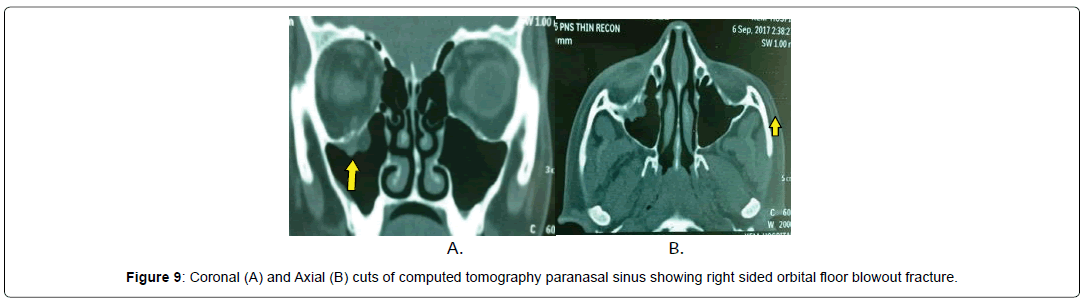
Endoscopic surgery was performed to repair orbital floor fracture (right sided) in a 12 year old male patient with a history of blunt trauma over the right eye while playing. He had complaints of diplopia on downward gaze with normal vision. Forced duction test was positive. Complete ophthalmologic examination was done. Computed tomography of paranasal sinus (axial and coronal) with 1mm orbital cuts (plain and contrast) showed a positive “tear drop” sign, suggestive of orbital floor fracture on the right side (Figure 9).
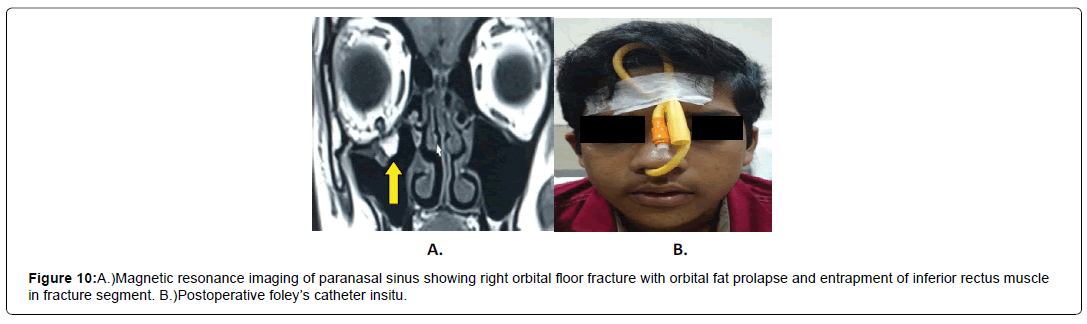
Magnetic resonance imaging of paranasal sinus was done which revealed orbital fat herniation with entrapped inferior rectus muscle in between the fractured bony segment (Figure 10, A). An endoscopic sinus surgery was performed. After uncinectomy, maxillary ostium was widened. Roof of maxilla was inspected using 70 degree endoscope and it was revealed that a part of inferior rectus muscle with orbital fat had prolapsed with orbital floor fracture. Bony spicules were removed. Entrapped muscle fibres released, reposited back and supported with gel foam. Foley’s catheter with its balloon filled with air was used as a tamponade to support the repair. It was kept for two weeks Postoperative diplopia was relieved gradually and completely (Figure 10).
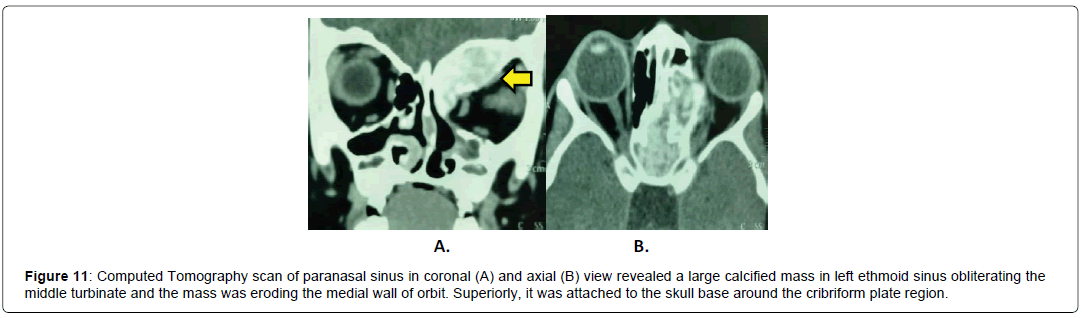
We operated on a three-year-old female child of Left sided ossifying fibroma with a history of proptosis. There was no history of diplopia or reduced vision. She had history of two to three episodes of epistaxis. Endoscopic excision of nasal mass was attempted at a peripheral centre before being referred to our hospital. The histopathology report and repeat CT scan of paranasal sinus were suggestive of ossifying fibroma of left ethmoid sinus and supraorbital region (Figure 11).She underwent revision endoscopic sinus surgery and spongiform bone was removed in a piecemeal fashion. Surgical specimen was sent for histopathological report and it was suggestive of Benign ossifying fibroma (Figure 11).
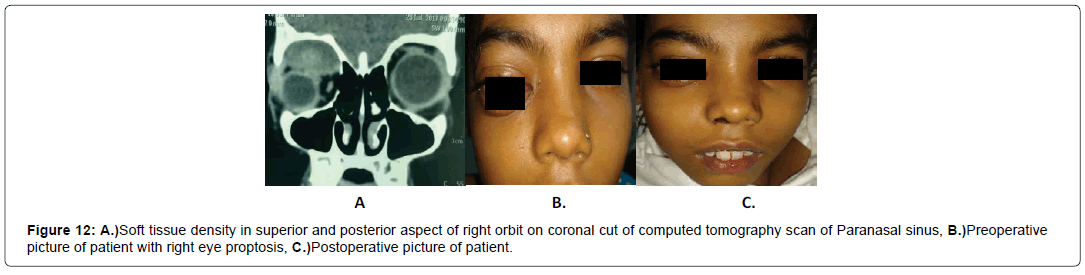
A 9 year old female patient was admitted in pediatric department for gradually increasing right sided orbital swelling (proptosis). She had painful eye movements. There was no history of trauma, nasal obstruction, recurrent rhinosinusitis, epistaxis or reduced vision. There was no ecchymosis, conjunctival congestion or any signs of inflammation. Hence clinically it was thought to be haematoma. All routine blood investigations were within normal limits. Chest x ray and electrocardiogram were also normal. Computed tomography of paranasal sinus with 1 mm orbital cuts was suggestive of right sided sub periosteal collection? hematoma (Figure 12).
Patient was immediately taken up for endoscopic orbital decompression to avoid visual impairment. Uncinectomy was done. Anterior and posterior ethmoidectomy was done. Lamina papyracea was removed for orbital decompression. Hematoma was drained. Postoperative proptosis was relieved in 5 to 7 days.Haemoglobin electrophoresis test was done as suggested by the paediatrician to identify the cause of spontaneous haemorrhage. As suspected, it turned out to be sickle cell anaemia. Here, patient was proved to be HbS homozygous and parents had sickle cell trait.
Postoperative Care
To have a good outcome, meticulous postoperative management is necessary. Aim of postoperative treatment is to treat the inflammation. This can be achieved by giving antibiotics (usually for 2 or more weeks in all patients),nasal saline spray, alkaline nasal douching, topical nasal steroids, tapering dose of oral steroids(in patients with diffuse polyposis), antihistamines, leukotriene inhibitors and avoidance of allergens. Also, post-surgery, older children (10 to 12 years of age group) should be followed up with nasal endoscopy. The first follow up after 7 days and after that, weekly or two weekly basis till healing is achieved is recommended. Any nasal crusts should be removed.
Results and Statistical Analysis
In our study period, out of 30 patients, Dacryocystitis (total 6), Orbital cellulitis (total 6), Juvenile nasopharyngeal angiofibroma (total 6), and Antrochoanal polyp (total 5) constituted the majority. Three patients had Meningocoele and one each of Ossifying fibroma, Choanal Atresia, Sub periosteal hematoma and orbital floor fracture.
Postoperative Care
To have a good outcome, meticulous postoperative management is necessary. Aim of postoperative treatment is to treat the inflammation. This can be achieved by giving antibiotics (usually for 2 or more weeks in all patients),nasal saline spray, alkaline nasal douching, topical nasal steroids, tapering dose of oral steroids(in patients with diffuse polyposis), antihistamines, leukotriene inhibitors and avoidance of allergens. Also, post-surgery, older children (10 to 12 years of age group) should be followed up with nasal endoscopy. The first follow up after 7 days and after that, weekly or two weekly basis till healing is achieved is recommended. Any nasal crusts should be removed.
Results and Statistical Analysis
In our study period, out of 30 patients, Dacryocystitis (total 6), Orbital cellulitis (total 6), Juvenile nasopharyngeal angiofibroma (total 6), and Antrochoanal polyp (total 5) constituted the majority. Three patients had Meningocoele and one each of Ossifying fibroma, Choanal Atresia, Sub periosteal hematoma and orbital floor fracture (Table 1-3).
| Indications | Male patient | Female patient | Total number of patients |
|---|---|---|---|
| 1.)Dacryocystitis | 3 | 3 | 6 |
| 2.)Orbital cellulitis | 4 | 2 | 6 |
| 3.)Juvenile Nasopharyngeal Angiofibroma | 6 | 0 | 6 |
| 4.) Antrochoanal Polyp | 3 | 2 | 5 |
| 5.)Meningocele | 1 | 2 | 3 |
| 6.)Ossifying Fibroma | 0 | 1 | 1 |
| 7.)Choanal Atresia | 0 | 1 | 1 |
| 8.)Non traumatic Orbital sub periosteal Hematoma | 0 | 1 | 1 |
| 9.)Orbital Floor Fracture | 1 | 0 | 1 |
Table 1: Indications of Endoscopic Sinus Surgery in paediatric population during study period.
| Age Distribution | Number of patients |
|---|---|
| 0 to 2 years | 2 |
| 2 to 4 years | 5 |
| 4 to 8 years | 12 |
| 8 to 12 years | 11 |
Table 2: Age distribution in our study period.
| Total | Bleeding | Orbital fat prolapse | CSF leak | Nasolacrimal duct injury | Blindness | Recurrence | |
|---|---|---|---|---|---|---|---|
| 1.) Dacryocystitis | 6 | Yes | No | No | No | No | 1 |
| 2.) Orbital cellulitis | 6 | Yes | No | No | No | No | 0 |
| 3.) Juvenile Nasopharyngeal Angiofibroma | 6 | Yes | No | No | No | No | 0 |
| 4.) Antrochoanal Polyp | 5 | Yes | No | No | No | No | 1 |
| 5.) Meningocele | 3 | Yes | No | No | No | No | 0 |
| 6.) Ossifying Fibroma | 1 | Yes | No | No | No | No | 0 |
| 7.) Choanal Atresia | 1 | Yes | No | No | No | No | 0 |
| 8.) Non traumatic Orbital sub periosteal Hematoma | 1 | Yes | No | No | No | No | 0 |
| 9.) Orbital Floor Fracture | 1 | Yes | No | No | No | No | 0 |
Table 3: List of complications that occurred in each endoscopic sinus surgery intra and post operatively.
Discussion
According to Messerklinger and Stammberger, most common site for chronic sinus disease is anterior ethmoids. The concept of osteomeatal complex was given by Messerklinger. In 1986, Dr. Kennedy introduced the term “functional endoscopic sinus surgery (FESS)” [1]. Initially it was used for adult patients only but Gross et al. applied the FESS procedure for pediatric population [2]. In majority of paediatric cases, conservative management is advised, but there are certain conditions where surgery becomes mandatory. For example, complications of sinusitis, choanal atresia, meningoencephalocele, antrochoanal polyp, etc. From technical point of view endoscopic sinus surgery in pediatric population is challenging due to narrow space, proximity to orbit and dura.
Complications associated with sinusitis in pediatric population commonly involves orbit in the form of periorbital or orbital cellulitis, sub periosteal or orbital abscess. It constitutes about 90% of all complications. In sinusitis, infection mostly spreads from ethmoid sinuses to orbital contents across lamina papyracea which is a very thin and porous bone and separates the nasal cavity from the orbit. Infection can also spread through roof of maxillary antrum or floor of frontal sinus. Valveless communication between orbital and frontal venous plexuses with cranial venous sinus system is responsible for indirect spread of infection [3-5]. According to Chandler’s classification there are 5 stages of periorbital inflammation and infection [6]. Stage 1.) Inflammatory oedema (preseptal cellulitis), Stage 2.) Orbital cellulitis, Stage 3.) Sub periosteal abscess, Stage 4.) Orbital abscess, and Stage 5.) Cavernous sinus thrombosis. In our study two patients had preseptal cellulitis while three had sub periosteal abscess and only one had intraorbital abscess.Clinically patients have complaints of localized nasal symptoms like nasal obstruction and purulent anterior or posterior nasal drainage. But along with these symptoms, patients with complicated sinusitis have features of cellulitis and abscess, proptosis and decreased ocular mobility. All our patients had proptosis but in none,extra ocular movement was affected,and no patient had decreased vision. Ophthalmological examination is a must for documentation in all cases of complicated sinusitis by means of vision assessment, extra ocular movements and pupillary reaction. Contrast-enhanced computed tomography (CT) scan of paranasal sinus plays the best role for identifying bony landmarks and anatomical variations. Garrett et al, studied 100 CT scans of paediatric population having complicated sinusitis and all of them had dehiscent lamina papyracea [7]. Oxford and McClay proposedmedical management if pupil and vision is normal. In endoscopic technique, by removing anterior ethmoid sinuses and lamina papyracea, drainage of sub periosteal abscess can be performed successfully and releases the pressure on the orbit [8]. In our study all 6 paediatric patients presented with acute sinusitis and orbital swelling [9-12]. All of them were subjected to orbital decompression. During surgery pus was drained through anterior ethmoids in most of the cases while in one case maxillary sinus was the culprit which was drained via endoscopic technique.
Antrochoanal polyp is a polypoidal mass, mostly unilateral, arising from ostium (main or accessory) of maxillary antrum. Classically it has 3 parts: antral, nasal and choanal part. From surgical point of view, uncinectomy is mandatory to unveil the natural ostium of maxillary sinus and it is widened using back biting forcep. Intraoperatively, if polyp is seen arising from accessory ostium, it is mandatory to join it with natural ostium in order to prevent recirculation of mucus. For its complete removal and better visualization, an angled endoscope (45 or 70 degree), angled blakesley forcep and angled microdebrider is required. Sometimes the choanal part is large enough to be delivered transorally. Hence, Boyle Davis mouth gag can be used for delivery of antrochoanal polyp from oral cavity. According to Mendelson and Gross widening of ostia to 3 to 5 times its normal size is required to prevent recurrence [13]. Maxillary attachment (lateral, inferior, medial or posterior wall) should be removed completely. Mohammad Eladl et al. studied 12 children (retrospective study) with unilateral recurrent Antrochoanal Polyp (5 left-sided, 7 right-sided) [14]. In his study, average age of patients with clinical symptoms was 9.3 years. All cases were treated by endoscopically with wide middle meatal antrostomy. In our study all patients were managed by endoscopic surgery with the help of 00 and angled (450 or 700) endoscope and of which one had a recurrence where the lateral most attachment was not removed completely.
Acute dacryocystitis in paediatric population may present with Dacryocystocoele which may sometimes get infected and form lacrimal abscess. It may get complicated leading to orbital cellulitis, orbital abscess and meningitis. The most common pathology is congenital nasolacrimal duct obstruction. Clinically it presents with inflammation and tenderness of medial canthal region and on applying pressure over lacrimal sac area mucopurulent material is exuded. Most of the time it is diagnosed by history and clinical examination but in case of post traumatic aetiology with suspected sinusitis, patient requires CT scan paranasal sinus with orbital cuts to know the bony landmarks. In paediatric patients, initial management consists of massaging in the region of lacrimal sac for at least 3-4 weeks. If it is not settled, then forced syringing under general anaesthesia is attempted and if that fails then probing can be done. The main indication for Dacryocystorhinostomy is recurrent attacks of dacryocystitis that are refractory to conservative management.Technically, Paediatric Endoscopic Dacryocystorhinostomy is similar to that performed in an adult. The importance of endoscopic DCR in paediatric population is that it is cosmetically safe and can be performed in an acute stage too. Postoperatively, patients have decreased morbidity. Studies by Cunningham and Woog showed that endonasal endoscopic Dacryocystorhinostomy prevents external scar formation and maintains the pump mechanism of tearing by avoiding injury to medial palpebral ligament and orbicularis oris muscle [15]. Kominek et al, reported 87.9% success rate [16]. In our study success rate was 84%. Hence, it can be safely concluded that endoscopic DCR is safe and effective in pediatric population. Of the 6 patients in our series that were managed endoscopically, one had recurrence which was managed endoscopically with ophthalmological assistance for localizing the lacrimal sac area that was found to be fibrosed. The child is on follow up with no complications till date.
Patients with meningocoele present with nasal mass, nasal blockage and rhinitis. In paediatric population, it is usually due to a congenital defect in cribriform plate. Meningocoele is a cerebrospinal fluid (CSF) filled hernial sac which is covered by meninges while meningoencephalocele additionally contains brain tissue or glial matter. Clinically only a mass is seen in the nasal cavity. Imaging in the form of CT scan which shows the defect in cribriform area and MRI are required to confirm the diagnosis. In our study, meningocoele was arising from a defect in the medial lamella of the cribriform plate. Endoscopic excision of meningocoele is done by using bipolar cautery with cauterization of its base. After excision, the defect is closed in multiple layers using septal cartilage, tensor fascia lata graft and fat. The repair is further strengthened usingtissue glue. The nasal cavity is then packed with polyvinyl oxycellulose for tamponade effect. Banhawy and Halaka in 2008 approached endonasally with different angled endoscopes to excise right nasal meningoencephalocoele and repair the defect by using posterior two third of ipsilateral inferior turbinate [17]. Schlosser in 2005, successfully repaired intranasal encephalocoele in 23 months old child by Trans nasal endoscopic approach. Hamlin and Kubba in 2007, treated nasal mening oencephalocele in a 6 month old infant by endoscopic technique [18]. In our study bipolar diathermy was used to remove the attachment of nasal meningocoele and encephalocoele. Combination of miniaturized instruments and a 4-mm 00 nasal endoscope gave excellent visual field and an adequate working space. Septal cartilage was harvested to repair the remaining defect. The surgery proved to be successful in 100% of our cases.
Choanal atresia is a rare condition. Its incidence is 1 in 5000. It may be unilateral or bilateral. The unilateral form is more frequent, but a bilateral presentation occurs in 30-40% of cases. As children are obligatory nasal breathers, bilateral choanal atresia is always an emergency. Clinically patients have complaints of breathing difficulty, feeding difficulty, cyanosis, and severe hypoxia. As described by Hall, it may be associated with other congenital anomalies like CHARGE syndrome (Coloboma, Heart disease, Atresia of choana, renal anomalies, Growth retardation, Ear defects) [19]. Our patient had unilateral choanal atresia. She had no associated anomaly.
When unilateral or bilateral atresia is suspected, the diagnosis can be confirmed at the bedside by the inability to pass catheter through the nose into the nasopharynx. Imaging is confirmatory. CT scan paranasal sinus in both axial and coronal view are helpful to differentiate bony from membranous choanal atresia. There are various approaches for surgical intervention to correct choanal atresia including trans-nasal, trans-septal, trans-palatal, trans-antral and sub labial approaches. But in recent years, Transnasal Endoscopic approach proves to be the best [20-22]. Larzer and Younis studied choanal atresia in 10 children and corrected it using transnasal endoscopic approach and suggested that key to success is to avoid raw area thereby preventing formation of granulations [22]. In endoscopic procedure, it is of utmost importance to respect the mucosa in nasal cavity to prevent granulation tissue formation surrounding raw area. One can use stent to prevent restenosis. In our centre we prefer to do posterior septectomy to prevent closure of the opening. In our study period only one patient of choanal atresia was treated endoscopically in whom otology instruments and insulated ball probe were used to create opening and posterior septectomy was performed to prevent restenosis and provide large choana. Posterior septectomy was performed to create space.
Juvenile nasopharyngeal angiofibroma is a benign nasal mass seen in 9 to 19 years of male patients most commonly. Friedberg coined the term angiofibroma. Patients present with unilateral or bilateral nasal obstruction with painless continuous nasal bleeding. Sometimes patient may present with cheek fullness and nasal twang of voice. Imaging in form of CT scan of paranasal sinus (plain+contrast) plays a crucial role to know the extent of tumour and for staging purpose. MRI can be considered if tumour has intracranial or orbital extension. Numerous approaches have been advocated for the surgical excision of Juvenile Nasopharyngeal Angiofibroma including lateral rhinotomy, midface degloving, transpalatal, transzygomatic, transhyoid, transpterygoidandtransmandibular approaches. Kamel proposed Transnasal Endoscopic approach for limited juvenile nasopharyngeal angiofibroma. Carrau, Snyderman, Kassam, Jungreis approached endoscopically for juvenile nasopharyngeal angiofibroma excision in pediatric patients age of 11 and 12 years [23,24]. Preoperative embolization is necessary to decrease bleeding intraoperative and for a better surgical field while operating thereby improving outcome [25,26]. Endoscopic approach is minimally invasive, precise and avoids external scar. It avoids distortion of facial skeleton. It allows early recovery and shortens hospitalisation. However one needs to understand its spread and master the art of operating this vascular tumour. There is a big learning curve. In case of difficulty, surgeon must be well versed with external approach if the need be.
Injury to orbit may cause fracture of bony orbital vault. Most common site of fracture is medial wall and floor of the orbit. It causes prolapse of orbital content into paranasal sinuses which may result in extaocular muscle entrapment, diplopia or enophthalmos. Sometimes visual loss can occur due to optic nerve injury. Fujino and Makino gave the concept of buckling mechanism for “trap door variety” of orbital floor fracture and most common extaocular muscle to be involved is inferior rectus and inferior oblique [27]. Rowe et al. suggested that orbital blow out fracture is of trapdoor variant [28]. To identify the exact location and extent of orbital floor fracture, contrast enhanced computed tomography is a must. 50% of orbital floor fracture is associated with increased orbital volume. Traditionally orbital floor fracture was managed through subciliary and transconjunctival incisions. But certain disadvantages were seen like postoperative lid malposition, entropion, ectropion and lid shortening [29,30]. The Caldwell Luc approach for repair of orbital floor fracture was described by Walter in 1972. With the help of endoscopic technique, repair of orbital floor fracture can be done [31]. It provides better visualization, less postoperative morbidity and greater patient acceptance. Strong et al. used endoscopic approach to repair the orbital floor after widening the maxillary ostium [32]. Endoscopic approach allows removal of fractured bony chip and reduction of prolapsed soft tissue involving muscle. After fracture reduction, one can use balloon catheter, implan (silicone or polypropylene) or titanium micromesh to maintain reduction in position [33-35]. We had one patient of orbital floor fracture. He had entrapment of inferior rectus muscle. In addition to Computed tomography of paranasal sinus with 1 mm orbital cuts, we also did magnetic resolution imaging of paranasal sinus to confirm prolapse of the muscle and fat. He was treated endoscopically. After widening maxillary ostium, angled endoscope was used to reduce the fracture and remove the loose bony fragments. Prolapsed muscle was identified and reduced which was supported by a piece of gelfoam. The entire repair was supported by inflated balloon of Foley’s catheter to provide stability of fractured segment after reduction. Patient’s diplopia improved gradually over three weeks.
Fibrous dysplasia is a slow progressive idiopathic benign condition where normal bone is replaced by immature woven bone and fibrous tissue. There is abnormal growth of osteoblastic mesenchymal tissue. In 1927, Montgomery coined the term ossifying fibroma. Fibrous dysplasia term was given by Lichtenstein and Jaffe [36]. When orbit is involved it may present with diplopia, proptosis, epiphora and diminution of vision. According to Schwartz and Alpert, there is a 0.5% risk of malignant transformation. Computed tomography of paranasal sinus gives a better idea regarding nature of tumour, size, and growth with adjacent orbital extension and also acts as a road map while performing surgery [37]. Role of Magnetic resonance imaging is limited. Surgery is to be avoided till the age of 18 years unless there is complication in form of decreased vision. Pasquini et al. managed successfully a child with fibrous dysplasia with aneurysmal bone cyst of maxillary sinus through endoscopic approach [38]. Kutluhan et al managedan11- year-old male boy who was diagnosed with ethmoidal fibrous dysplasia and complete removal of tumour by endoscopic approach [39]. We had one patient of fibrous dysplasia of left ethmoids, who was managed with endoscopic sinus surgery. During follow up her orbital swelling (proptosis) decreased. It usuallytakes a long time for the bone to remodel.
Nontraumatic sub periosteal orbital hematoma also known as spontaneous orbital haemorrhage, idiopathic orbital haemorrhage or orbital hematoma. It includes all types of bleeding in the orbit in the absence of trauma. According to McNab and Franzco, the causes of nontraumatic orbital hematoma are vascular malformation, increased cranial venous pressure, bleeding disorders or as a complication of sinusitis, scurvy and barotrauma. Haemoglobin electrophoresis test can detect abnormal levels of HbS, type of haemoglobin associated with sickle cell disease, as well as other abnormal haemoglobin related blood disorders, such as thalassemia and haemoglobin C.Hemoglobinopathy in form of Sickle cell disease is responsible for sub periosteal bleeding and orbital bone infarction [40]. In sickle cell “crises” red blood cells change to crescent shape and becomes relatively rigid which leads to vasoocclusion .The bone of orbital roof and greater wing of sphenoid suffer ischemia and infarction resulting in collection of blood in sub periosteal space. At times, proptosis can be painful. In our case it was painless proptosis. Besides clinical features radiological imaging tools like CT scan and MRI also play an important role in diagnosis and management. Computed tomography scan of Paranasal sinus (axial and coronal) with 1mm orbit cuts helps in confirming fluid level and exact site of collection. Khouri et al, studied a case of bilateral nontraumatic sub periosteal orbital haemorrhage in a patient with sickle cell disease who had also vitamin C deficiency [41]. Endoscopic sinus surgery is helpful in orbital decompression by draining the hematoma. This helps in reducing pressure on the optic nerve and decreasing proptosis. Stankiewickz dealt with a case of orbital hematoma in an 8 year old patient and used the endoscopic approach to drain it [42]. We had one patient of right sided nontraumatic sub-periosteal orbital hematoma who presented to us with proptosis and was managed successfully with endoscopic drainage of hematoma and orbital decompression. Haemoglobin electrophoresis test was used to confirm Sickle cell anaemia as a cause.
Conclusion
Endoscopic sinus surgery in pediatric population is feasible. Despite being technically challenging to operate in a narrow space with smaller instruments , endoscopic approach offers the advantage of reduced postoperative pain, avoidance of scar over face, a shortened hospital stay, decreased recovery period and a prompt return to normal activities. The use of fine and delicate otology instruments prevent excessive mucosal trauma and bleeding, thereby allowing a more meticulous surgery and an improved surgical outcome. Since the endonasal approach is minimally invasive with high success rate, we highly recommend it for paediatric population needing sinus surgery. A thorough knowledge of anatomy and basic experience in adult endoscopic sinus surgery is mandatory. There is a learning curve; as here, one needs to manipulate instruments in narrow nasal cavity. Miniaturisation of instruments in the form of otology set allows use of standard 4 mm endoscope which give excellent vision in the nasal cavity.
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethical Approval
The study was approved by the institutional review board of King Edward Memorial Hospital.
Statement of Human and Animal Rights
This study was performed in compliance with the Declaration of Helsinki.
Statement of Informed Consent
A full informed consent was obtained from all the participants.
References
- Stammberger HR, Kennedy DW, Anatomic Terminology Group. (1995) Paranasal sinuses: anatomic terminology and nomenclature. Ann Otol Rhinol Laryngol Suppl. 167: 7-16.
- Gross CW, Gurucharri MJ, Lazar HR, Long TE. (1989) Functional endonasal sinus surgery (FESS) in the pediatric age group. Laryngoscope 99: 272-275.
- Swift AC, Charlton G. (1990) Sinusitis and the acute orbit in children. J. Laryngol. Otol. 104: 213-216.
- Wald ER, Pang D, Milmore GJ. (1981) Sinusitis and its complications in paediatric patients. Paediatr. Clin. North Am. 28: 777–796.
- Uzcategui N, Warman R, Smith A. (1998) Clinical practice guideline for the management of orbital cellulitis. J Paediatr Opthalmol Strabismus 35: 73–79.
- Chandler JR, Langenbrunner DJ, Stevens ER. (1970) The pathogenesis of orbital complications in acute sinusitis. Laryngoscope 80: 1414–1428.
- Garrett MGJ, Elmaraghy CA, Jatana KR. (2012) Radiographic findings in pediatric periorbital cellulitis. American Society of Pediatric Otolaryngology (ASPO).
- Oxford L E, Mc Clay J. (2006) Medical and surgical management of subperiosteal orbital abscess secondary to acute sinusitis in children. Int J Pediatr Otorhinolaryngol 70: 1853-1861.
- Bhargava D, Sankhla D, Ganesan A. (2001) Endoscopic sinus surgery for orbital subperiosteal abscess secondary to sinusitis. Rhinology 39: 151–155
- Page EL, Wiatrak BJ. (1996) Endoscopic vs external drainage of orbital subperiosteal abscess. Arch Otolaryngol Head Neck Surg. 122: 737–740.
- Kessler A, Berenholz LP, Segal S. (1998) Transnasal endoscopic drainage of a medial subperiosteal abscess. Eur Arch Otorhinolaryngol 255: 293–295.
- Younis RT, Lazar RH. (1996) Endoscopic drainage of subperiosteal abscess in children: a pilot study. Am J Rhinol 10: 11–15.
- Mendelson MG, Gross CW. (1997) Soft-tissue shavers in pediatric sinus surgery. Otolaryngol Clin North Am 30: 443-9.
- Eladl HM, Shawky M. (2011) Endoscopic surgery in pediatric recurrent antrochoanal polyp. Int J Pediatr Otorhinolaryngol 75: 1372-1375.
- Michael JC, John JW. (1998) Endonasal Endoscopic Dacryocystorhinostomy in Children. Arch of otolaryngol Head Neck Surg 124: 328-333
- Kominek P, Cervenka S, Matousek P, Pniak T, Zelenik K. (2010) Diagnosis of extraesophageal reflux in children with chronic otitis media with effusion using Peptest. Int J Pediatr Otorhinolaryngol 74: 661-664.
- Omar AE, Halaka AN, Hekma El. (2009) Endoscopic Management of Congenital Intranasal Meningocele in 3-Month Old Infant. J Pediatr Otorhinolaryngol Extra 4: 66—71
- Hamlin K, Kubba H. (2007) Endoscopic excision of a nasal meningoencephalocoele in an infant. Int J Pediatr Otorhinolaryngol Extra 2: 92—94.
- Hall BD. (1979) Choanal atresia and associated multiple anomalies. J Pediatr 95: 395-398.
- El-Guindy A, El-Sherif S, Hagrass M. (1992) Endoscopic endonasal surgery of posterior choanal atresia. J Laryngol Otol 106: 528-529.
- Kamel R. (1994)Transnasal endoscopic approach in congenital choanal atresia. Laryngoscope 104: 642-646.
- Lazar RH, Younis RT. (1995) Transnasal repair of choanal atresia using telescopes. Arch Otolaryngol Head Neck Surg 121: 517-520.
- Kamel RH. (1996) Transnasal endoscopic surgery in juvenile nasopharyngeal Angiofibroma. J Laryngol Otol 110: 962-968.
- Carrau RL, Snyderman CH, Kassam AB, Jungreis CA. (2001) Endoscopic and Endoscopic-Assisted Surgery for Juvenile Angiofibroma. Laryngoscope 111: 483–487.
- Marshall AH, Bradley PJ. (2006) Management dilemmas in the treatment and follow-up of advanced juvenile nasopharyngeal angiofibroma. ORL J Otorhinolaryngol Relat 68: 273-278.
- Wormald PJ, Van Hasselt A. (2003) Endoscopic removal of juvenile angiofibroma. Otolaryngol Head Neck Surg 129: 684-691.
- Fujino T, Makino K. (1980) Entrapment mechanism and ocular injury in orbital blowout fracture. Plast Reconstr Surg 65: 571-576.
- Rowe NL. (1968) Fractures of facial skeleton in children. J Oral Surg 26: 505-515.
- Appling WD, Patrinely JR, Salzer TA. (1993) Transconjunctival approach vs subciliary skin muscle flap approach for orbital fracture repair. Arch Otolaryngol Head Neck Surg 119: 1000–1007.
- Walter WL. (1972) Early surgical repair of blowout fracture of the orbital floor by using the transantral approach. South Med J 65: 1229–1243.
- Strong EB, Kim KK, Diaz RC. (2004) Endoscopic approach to orbital blowout fracture repair. Otolaryngol Head Neck Surg 131: 683-695.
- Farwell DG, Strong EB. (2006) Endoscopic Repair of orbital floor fracture. Facial Plast Surg Clin North Am 14: 11–16.
- Jordan DR, Allen LH, White J. (1998) Intervention within days for some orbital floor fractures: The white-eyed blowout. OPhthal Plast Reconstr Surg 14: 379-90.
- Chen CT, Chen YR. (2001) Endoscopically assisted repair of orbital floor fractures. Plast Reconstr Surg; 108: 2011–2018.
- Montgomery AH. (1927) Ossifying fibroma of the jaw. Arch Surg 15: 30-44.
- Schwartz DR, Alpert MA. (1964) The malignant transformation of fibrous dysplasia. Am J Med Sci 274: 1-20.
- Pasquini E, Compadretti GC, Sciarretta V, Ippolito A. (2002) Transnasal endoscopic surgery for the treatment of fibrous dysplasia of maxillary sinus associated to aneurysmal bone cyst in a 5-year-old child, Int J Pediatr Otorhinolaryngol 11: 59-62.
- Kutluhan A, Kiroglu AF, Yurttas V, Arslan H, Ozen S. (2004) Monostotic fibrous dysplasia originating from ethmoid bone: treatment with endoscopic approach, Ann Otol Rhinol Laryngol 113: 139-141.
- McNab AA. (2014) Nontraumatic orbital haemorrhage, Surv Ophthalmol 59: 166-184.
- Khouri LM, Kersten RC, Kulwin DR. (2002) Bilateral subperiosteal orbital hematomas in a child with sickle cell disease. J Pediatr Ophthalmol Strabismus 39: 182-4.
- Stankiewicz JA, Chow JM. (1999) Two faces of orbital hematoma in intranasal (endoscopic) sinus surgery. Otolaryngol Head Neck Surg 120: 841-847.
Citation: Marfatia HK, Goyal P, Madhavi A, Ashwathy KP (2020) An Observational (Analytical) Retrospective cum Prospective Study of Cases of Endoscopic Sinus Surgery in Paediatric Population. Otolaryngol (Sunnyvale) 10: 406. DOI: 10.4172/2161-119X.1000406
Copyright: © 2020 Marfatia HK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3610
- [From(publication date): 0-2020 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 2754
- PDF downloads: 856