Antenatal Care Service Utilization and its Associated Factors among Mothers who Gave Live Birth in the Past One Year in Womberma Woreda, North West Ethiopia
Received: 05-Aug-2015 / Accepted Date: 10-Sep-2015 / Published Date: 18-Sep-2015 DOI: 10.4172/2161-1165.S2-003
Abstract
Background: Utilization of antenatal care is very low in Ethiopia and there is also urban-rural disparities as more urban-women utilizing the care than rural mothers. Focusing on mothers who gave live birth in the past one year, this study has examined and compared utilization of antenatal care in urban and rural mothers and its determinants in Womberma Woreda, Northwest Ethiopia.
Methods: A comparative community based cross-sectional study was conducted among 930 randomly selected mothers who gave live birth in past one year in Womberma Woreda. Data were entered into Epi data version 3.1 and analyzed using SPSS version 21.0 software. Logistic regression was done to identify the possible factors associated with Antenatal Care utilization.
Result: In this study utilization of antenatal care was slightly higher in urban areas, 213 (69.2%) than in rural areas, 373 (64.3%). Utilization of antenatal care was significantly associated and higher among mothers in rural areas with the age of 30 years or older, three or more live births, had a history of abortion and previous ANC visit (AOR (95% C.I): 1.92 (1.16, 3.18)). Mothers from urban area who were government employed were more likely to the service (AOR (95% C.I): 4.30 (1.88, 9.81)). However, in both urban and rural areas, mothers who had a planned pregnancy and autonomy on health care decision making were found to be significantly associated and higher in utilizing the service.
Conclusion: As compared to government plan the level of antenatal care utilization among mothers who gave live birth in the past one year, both in urban and rural areas of Womberma Woreda was found to be very low. Even though the gap, i.e., utilization of antenatal care in urban and rural women was very low, there is a difference in accessing and utilizing the service in the Woreda.
Keywords: Antenatal care; Pregnant mothers; Skilled maternal care; Ethiopia
167126Background
Ethiopia is a major contributor of maternal deaths in the world with a maternal mortality ratio of 673 per 100,000 live births and 19,000 maternal deaths annually. However, improvements have been reported in regard to infant and child mortality reduction, there has been slow progress regarding achieving Millennium Development Goal 5 [1]. In the Ethiopia the mean maternal mortality burden, measured by Maternal Death Risk Factor Index (MDRFI), is at 3.03 and Somali is with the highest mean maternal mortality burden (mean=3.33) followed by Afar (mean=3.21) regions. Similarly, high MDRFI mean values were found in SNNP (mean=3.11), Amhara (mean=3.09), and Oromia (mean=3.08) regions. The overall maternal mortality burden was in the three most populous regions of the country (SNNP, Oromia and Amhara) constituting over 75% of the country’s population [2].
The 2011 EDHS data showed that the national maternal mortality ratio (MMR) is at 676/100,000 live births and in the five regions of the country the magnitude is higher than the national average. The highest maternal mortality ratio is documented in Somali region (747 per 100,000 live births) followed by Afar (717 per 100,000 live births), SNNP (694 per 100,000 live births), Amhara (690 per 100,000 live births), and Oromia (688 per 100,000 live births) regions [3].
In the year 2009/10, Ethiopia had launched a Community Based Health Care System, i.e., the Health Extension Program with the main focus to improve accessibility of family planning, safe abortions, ANC, skilled delivery and postpartum care in the community where Health Extension Workers are the Frontlines [4]. For rural areas, the Program has 16 packages of interventions categorized into four main areas: ‘hygiene and environmental sanitation’ (seven packages), ‘family health’ (five packages), ‘disease prevention and control’ (three packages), and ‘health education and communication’ (one package). The Health Extension Workers, with regard to maternal health, are expected to provide post-abortion care, family planning, antenatal care, clean delivery and postnatal care. Furthermore, they are responsible for referring women with obstetric complications to higher health institutions where basic and comprehensive emergency obstetric care is available [5].
Antenatal care (ANC) is the care that a pregnant woman receives while she is pregnant through a series of consultations with a trained health care provider, i.e., midwives, nurses, and medical doctors [3,6-9]. The most recent the 2014 Ethiopian Mini Demographic and Health Survey (EMDHS) has revealed that about 40% of women [9]; a noticeable increase from a 34% in 2011 [3], who gave birth in the five years preceding the survey had received antenatal care from a skilled provider for their most recent birth. Urban women are more than twice in receiving antenatal care than rural women; 79.5% women residing in urban areas received ANC from skilled providers as compared to 34.7% of women in rural areas [9]. Similarly, antenatal care from skilled providers ranges from a low of 15% in the Somali region to a high of 94% in Addis Ababa. Education has a direct impact on utilization of antenatal care; 31% of women with no education had received the services as compared to 96% of women with more than secondary education [9].
A trend analysis of the Ethiopian Demographic and Health Survey from 2000 to 2011 showed that there was a significant increase in the proportion of women who had at least one ANC from 27.2% in 2000 to 28.3% in 2005 and 42.5% in 2011. The increase was significant during the period 2005 to 2011 [2]. In the last decade the trend in utilizing antenatal care was significantly different based on urban-rural residence and region [2]. A cross sectional study done in Tigray Region, Ethiopia showed that utilization of antenatal care service was significantly associated with marital status, education, proximity of health facility and husband’s occupation [10]. Another study done in Hadiya Zone, Ethiopia also showed that maternal age, husband’s attitude, family size, maternal education, and perceived morbidity were siginificantly associated with antenatal care service utilization [11].
Several studies have identified urban-rural disparities in utilizing antenatal care services in different countries [7,12-16]. The higher coverage of antenatal care in urban areas than rural areas worldwide has been due to the inequalities in the number of accessible health facilities [16-18]. Futhermore, utilization of antenatal care services is affected by socio-demographic characteristics. Service fees were an important barrier in utilizing antenatal care [7,13,19]. Distant health facilities and insufficient number of antenatal care providers at various health institutions negatively affect utilization of antenatal care services [14].
A study done in Nigeria showed that the barriers for utilization of antenatal care services were unavailability of transport, lack of money and distant health facilities [20]. In urban areas education of the woman and education of husband was also significantly associated with utilization of antenatal care services [21]. Both in urban and rural settings, women’s education were significantly associated and higher in antenatal care utilization [22].
Despite the enormous efforts that the Ethiopian government made, universal access to maternal health services remains limited. Therefore, this study was aimed to compare antenatal care utilization between urban and rural mothers and its determinants among mothers who gave live birth in the past one year in Womberma Woreda, Northwest Ethiopia.
Materials and Methods
Study area
Womberma woreda is one of the woreda’s in West Gojam zone of Amhara Regional State located at 427 km from Addis Ababa and 172 km from Bahir Dar, capital city of the region. The woreda has a total of 20 kebeles, 19 rural and one urban kebeles. According to the 2014 woreda health office population estimation, the woreda has a total population of 122,068; 109,193 rural and 12,875 urban populations. In the woreda women of reproductive age (15-49 years) account 28,784 (23.58%) of the entire population. The woreda has five health centers, 19 health posts and seven medium private clinics with 100% health service coverage [23].
Study design
A community based comparative cross-sectional study was conducted among mothers who gave live birth in the past one year in rural and urban residents of Womberma woreda.
Sampling
The sample size was determined using a formula for two proportions by taking a 95% confidence interval, 5% level of significance, and the power of 80%. Considering place of residence as a factor for antenatal care utilization; antenatal care utilization among urban resident (p1) of 88.9% [24] and among rural mothers (p2) of 77.4% [25] were taken. A two to one ratio (r) of n2 to n1 was taken and based on the above assumptions, none response rate of 10% and design effect of 2, the final sample size became 930. Therefore, 310 samples from urban women (n1) and 620 samples from rural women (n2) were selected for the study.
The study participants were selected using a multistage sampling technique: at stage one six kebeles were selected from the total 20 kebeles in the woreda. One urban kebele (Shindy Town) was directly taken while five rural kebeles (25% of the 19 rural kebeles) were taken by using simple random sampling method. In the selected six kebeles there were 1,746 households who had mothers who gave live birth in the past one year. Therefore, at stage two 930 households; 310 urban and 620 rural households were selected using a systematic sampling method with proportionate allocation to size in each kebeles. Then in each household one mother who gave live birth within a year preceding the survey were interviewed and two visits were made for absences in the first visits.
In this study all mothers who gave live birth within one year and reside at least 6 months in the woreda preceding the data collection were included. However, those mothers who were sick, mentally ill and who were not able to communicate were excluded from the study.
Data collection
A pretested interview administered structured questionnaire was used. The questionnaire mainly focused on socio-demographic, obstetric and accessibility characteristics, was first prepared in English version and then translated into the local language (Amharic) and finally to English to its consistency. The purpose of the study was briefed about the study participants and data were collected after obtaining written informed consent. The data collection process was facilitated by nine Health Extension Workers and three supervisors with a qualification of public health.
Data quality was assured through careful design of the questionnaire. Data collectors and supervisors were trained for two days about the purpose of the study, including the rights of study participants and the content of the questionnaire in detail as well before the commencement of actual data collection. Data were checked for completeness and consistency after each day of data collection by holding a meeting with the data collectors and supervisors.
Data analysis
Data were entered using Epi Data version 3.1 and analysis was performed using SPSS version 21.0 statistical software. Bivariate and multivariable models were run to assess any relationship between each independent variable and the outcome variable. Crude and adjusted odds ratios were used to any significant associations between the dependent and independent variables while significance was determined at a 95% confidence interval. Independent variables found to have p-value less than 0.05 at the bivariate level were included in a multivariable analysis.
Ethical Consideration
Ethical approval was obtained from Debremarkos University, College of Medicine and Health Sciences Ethical Clearance Committee and approval letter was obtained from the Womberma Woreda Health Office. The purpose of the study was explained to the mothers and written informed consent was obtained from them. Confidentiality of information was maintained by omitting any personal identifier from the questionnaires. The recorded data was stored in a safe place where no one except the principal investigator had access.
Results
Socio-demographic characteristics of respondents
In this study out of 310 and 620 urban and rural mothers, 308 and 580 urban and rural mothers who gave live birth within the past one year were participated obtaining a response rate of 99.35% and 93.55% respectively. The mean age of the urban and rural mothers were 27.54 (±4.33) and 28.48 (±5.87) years respectively. The majority of them, for both urban and rural women, respectively, were within the age group of 25-29 years, 167 (54.2%) and 184 (31.4%). Most of the study participants were Orthodox Christian in religion, 269 (87.3%) of urban and 557 (96.0%) of rural women.
Concerning respondent’s marital status most of them, 292 (94.8%) of urban and 533 (91.9%) of rural women were currently married. Above a quarter of urban women, 87 (28.2%) can read and write while 214 (36.9%) of rural women were illiterate in education. The majority of them, i.e., 132 (42.9%) of urban and 259 (44.7%) of rural women were housewives in occupation.
For those mothers who were currently married, 56 (19.2%) and 153 (28.8%) of urban and rural women’s husbands had attained a primary level of education and can read and write respectively. Concerning their husband’s occupation, 142 (48.8%) and 336 (63.2%) of urban and rural women’s husbands were merchant and farmer respectively. One hundred twenty (39.0%) of urban and 240 (41.4%) of rural women had a monthly expenditure of less than or equal to 2,000 Ethiopian Birr (Table 1).
| Variable | Category | N | Urban (n=308) | N | Rural (n=580) | N | Total% |
|---|---|---|---|---|---|---|---|
| Age | ≤24 years | 69 | 22.2 | 165 | 28.4 | 234 | 26.4 |
| 25-29 years | 167 | 54.2 | 184 | 31.4 | 351 | 39.5 | |
| 30-34 years | 39 | 12.7 | 100 | 17.2 | 139 | 15.7 | |
| ≥35 years | 33 | 10.7 | 131 | 22.6 | 164 | 18.5 | |
| Religion | Orthodox | 269 | 87.3 | 557 | 96 | 826 | 93 |
| Muslim | 27 | 8.8 | 15 | 2.6 | 42 | 4.7 | |
| Protestant | 12 | 3.9 | 8 | 1.4 | 20 | 2.3 | |
| Educational status | Illiterate | 28 | 9.1 | 214 | 36.9 | 242 | 27.3 |
| Read and Write Only | 87 | 28.2 | 128 | 22.1 | 215 | 24.2 | |
| Primary | 77 | 25 | 85 | 14.7 | 162 | 18.2 | |
| Secondary | 34 | 11 | 95 | 16.4 | 129 | 14.5 | |
| Preparatory | 26 | 8.4 | 9 | 1.6 | 35 | 3.9 | |
| 12+ | 56 | 18.2 | 49 | 8.4 | 105 | 11.8 | |
| Educational status of husband | Illiterate | - | - | 111 | 20.9 | 111 | 13.5 |
| Read and Write Only | - | - | 153 | 28.8 | 153 | 18.6 | |
| Primary | 56 | 19.2 | 102 | 19.2 | 158 | 19.2 | |
| Secondary | 44 | 15.1 | 56 | 10.5 | 100 | 12.1 | |
| Preparatory | 44 | 15.1 | 22 | 4.1 | 66 | 8 | |
| 12+ | 148 | 50.7 | 88 | 16.5 | 236 | 28.6 | |
| Occupational status | Housewife | 132 | 42.9 | 259 | 44.7 | 391 | 44 |
| Merchant | 76 | 24.7 | 71 | 12.2 | 147 | 16.6 | |
| Farmer | - | - | 174 | 30 | 174 | 19.6 | |
| Student | - | - | 24 | 4.1 | 24 | 2.7 | |
| Employed | 100 | 32.5 | 52 | 9 | 152 | 17.1 | |
| Occupational status of husband | Farmer | 15 | 5.2 | 336 | 63.2 | 351 | 42.6 |
| Merchant | 142 | 48.8 | 65 | 12.2 | 207 | 25.2 | |
| Employed | 120 | 41.2 | 115 | 21.6 | 235 | 28.6 | |
| Others* | 14 | 4.8 | 16 | 3 | 30 | 3.6 | |
| Marital status | Married | 292 | 94.8 | 533 | 91.9 | 825 | 92.9 |
| Others** | 16 | 5.2 | 47 | 8.1 | 63 | 7.1 | |
| Ethnicity | Amhara | 305 | 99 | 580 | 100 | 885 | 99.7 |
| Tigrie | 3 | 1 | - | - | 3 | 0.3 | |
| Family size | 01-Mar | 191 | 62 | 247 | 42.6 | 438 | 49.3 |
| 04-Jun | 103 | 33.4 | 247 | 42.6 | 350 | 39.4 | |
| 07-Oct | 14 | 4.5 | 86 | 14.8 | 100 | 11.3 | |
| Household | ≤2,000 Birr | 120 | 39 | 240 | 41.4 | 360 | 40.5 |
| Expenditure | 2,001-4,000 Birr | 118 | 38.3 | 210 | 36.2 | 328 | 36.9 |
| (Eth. Birr) | ≥4,001 Birr | 70 | 22.7 | 130 | 22.4 | 200 | 22.5 |
*Student, daily laborer, **Single, divorced, widowed and separated)
Table 1: Socio-demographic characteristics of pregnant mothers and mothers who gave live birth within the past one year in Womberma Woreda, Northwest Ethiopia, 2015 (n=888).
Obstetric characteristics of respondents
Out of the total 308 urban mothers, the mean age of their first age at marriage, pregnancy and delivery was at 21.18 (+2.64), 23.35 (+2.41) and 24.17 (+2.42) years respectively. However, for rural women it was lower than urban counterparts, i.e., 17.87 (+3.12), 20.96 (+2.84) and 21.65 (+2.84) years respectively. Nearly two third of rural women, 379 (65.3%) were engaged in their first marriage before the age of 20 as compared to 61 (19.9%) of urban women. On the other hand, 364 (62.8%) and 355 (54.3%) of rural women and 194 (63.0%) and 130 (42.2%) of urban women were pregnant and gave birth for the first time when they were within the age group of 20-24 years respectively.
Concerning gravidity and parity, 64 (22.1%) of urban women and 295 (50.9%) of rural women were pregnant for more than two times; 44 (14.3%) of urban women and 234 (40.3%) of rural women had given more than two births. Thirty six (22.0%) and 115 (29.0%) of urban and rural women had a history of abortion respectively. Mothers who had previous pregnancies (560), 90 (54.9%) and 169 (42.7%) of urban and rural women had previous antenatal care visits respectively. One hundred four (33.8%) and 207 (35.7%) of recent pregnancies were not planned for both urban and rural women’s respectively (Table 2).
| Variable | Urban | Rural | Total | ||||
|---|---|---|---|---|---|---|---|
| N | % | N | % | N | % | ||
| Age at first marriage (n=888) | ≤19 years | 61 | 19.9 | 379 | 65.3 | 440 | 49.5 |
| 20-24 years | 217 | 70.5 | 194 | 33.4 | 441 | 46.3 | |
| ≥25 years | 30 | 9.7 | 7 | 1.2 | 37 | 4.2 | |
| Age at first pregnancy (n=888) | ≤19 years | 32 | 10.4 | 159 | 27.4 | 191 | 21.5 |
| 20-24 years | 194 | 63 | 364 | 62.8 | 558 | 62.8 | |
| ≥25 years | 82 | 26.6 | 57 | 9.8 | 139 | 15.7 | |
| Age at first delivery (n=888) | ≤19 years | 9 | 2.9 | 151 | 26 | 160 | 18 |
| 20-24 years | 130 | 42.2 | 315 | 54.3 | 445 | 50.1 | |
| ≥25 years | 169 | 54.9 | 114 | 19.7 | 283 | 31.9 | |
| Gravidity (n=888) | 01-Feb | 240 | 77.9 | 285 | 49.1 | 525 | 59.1 |
| ≥3 | 68 | 22.1 | 295 | 50.9 | 363 | 40.9 | |
| Parity (n=888) | 1-2 child | 264 | 85.7 | 346 | 59.7 | 610 | 68.7 |
| ≥3 children | 44 | 14.3 | 234 | 40.3 | 278 | 31.3 | |
| History of abortion (n=560) | Yes | 36 | 22 | 115 | 29 | 151 | 27 |
| No | 128 | 78 | 281 | 71 | 409 | 73 | |
| History of still birth (n=560) | Yes | 9 | 5.5 | 21 | 5.3 | 30 | 5.4 |
| No | 155 | 94.5 | 375 | 94.7 | 530 | 94.6 | |
| Recent pregnancy planned (n=888) | Yes | 204 | 66.2 | 373 | 64.3 | 577 | 65 |
| No | 104 | 33.8 | 207 | 35.7 | 311 | 35 | |
| Have previous ANC visit (n=560) | Yes | 90 | 54.9 | 169 | 42.7 | 259 | 46.3 |
| No | 74 | 45.1 | 227 | 57.3 | 301 | 53.8 | |
| Autonomy on Healthcare Decision | Woman | 42 | 13.6 | 58 | 10 | 100 | 11.3 |
| Husband | 133 | 43.2 | 52 | 9 | 185 | 20.8 | |
| Both | 133 | 43.2 | 470 | 81 | 603 | 67.9 | |
Table 2: Obstetric characteristics of mothers who gave live birth within the past one year in Womberma woreda, Northwest Ethiopia, 2015.
Level of antenatal care service utilization
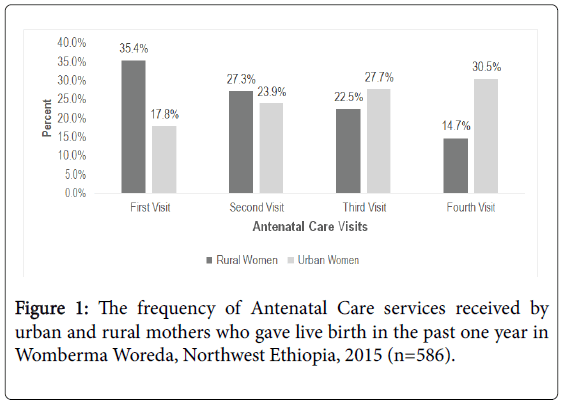
In this study 213 (69.2%) and 373 (64.3%) of urban and rural women had utilized antenatal care services respectively. The majority of urban women, 65 (30.5%) of them had four antenatal care visits while only 55 (14.7%) of rural women had four ANC visits. Concerning the time of first ANC visits, a comparable proportion, i.e., 89 (41.8%) and 151 (40.5%) of urban and rural women had attended antenatal care services for their recent pregnancies during the first trimester respectively (Figure 1).
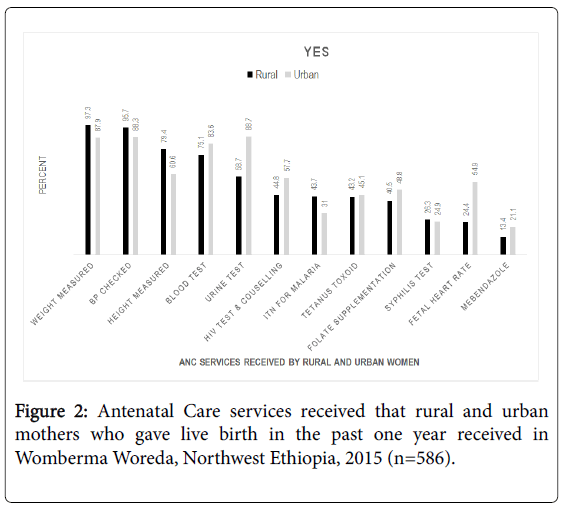
Concerning the services that the mothers received during their recent pregnancies, both women in urban and rural areas, below half of them were provided ITN for malaria, syphilis test, tetanus toxoid, and folate supplementation. However, above half, 57.7% of women in urban centers were counselled and offered for HIV testing as compared to 44.8% of women in rural areas (Figure 2).
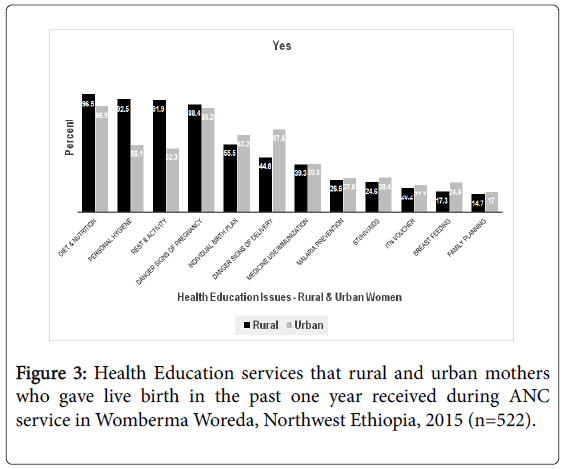
A ten percent more rural mothers, 346 (92.8%) than urban mothers, 176 (82.6%) had received education during their recent Antenatal Care follow up services. Above three quarters of the mothers, both mothers in urban rural areas had received education on diet and nutrition and danger signs of pregnancy. On the other hand, on some issues, stress was not given as below half of the mothers; for instance on prevention of malaria, information and counseling services about STI/HIV, breastfeeding and family planning had received antenatal education. In case of danger signs of delivery complications, about two third, 119 (67.6%) of urban mothers had received education as compared to 155 (44.8%) of women in rural area (Figure 3).
Factors affecting utilization of antenatal care services
In the bivariate analysis; for urban mothers, age of respondent, educational status, occupation, history of abortion, planned recent pregnancy, previous antenatal care visit and had autonomy on health care decision making were found to be significantly associated with ANC utilization. However, in the multiple logistic regressions, age, education and previous ANC visit didn’t show any significant association with ANC service utilization.
Government employed urban resident women were 4.30 times more likely to utilize ANC service compared to housewives and merchants (AOR (95% C.I): 4.30 (1.88, 9.81)). Similarly, urban mothers whose recent pregnancy were planned were 3.54 times more likely to utilize the service than their counterparts (AOR (95% C.I): 3.54 (1.45, 8.67)). Antenatal care service utilization was 7.02 times more likely in a household where women had autonomy on health care decision making (AOR (95% C.I): 7.02 (2.00, 24.60)) than those households where the decision was made by husband only and/or both the couples (Table 3).
| Variable | Category | Utilization of ANC | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Yes n (%) | No n (%) | ||||
| Age Group | ≤24 years | 55 (79.7) | 14 (20.3) | 1 | 1 |
| 25-29 years | 112 (67.1) | 55 (32.9) | 1.93 (0.99-3.77) | 0 | |
| 30-34 years | 29 (74.4) | 10 (25.6) | 1.36 (0.54-3.43) | 0 | |
| ≥35 years | 17 (51.5) | 16 (48.5) | 3.70 (1.50-9.10)** | 0 | |
| Educational | Illiterate | 25 (89.3) | 3 (10.7) | 1 | 1 |
| Status | Read and write only | 61 (70.1) | 26 (29.9) | 3.55 (0.99-12.81) | 1.74 (0.29-10.48) |
| Primary | 54 (70.1) | 23 (29.9) | 3.55 (0.97-12.94) | 1.87 (0.30-11.80) | |
| Secondary | 23 (67.6) | 11 (32.4) | 3.99 (0.99-16.11) | 1.43 (0.18-11.51) | |
| Preparatory | 13 (50.0) | 13 (50.0) | 8.33 (2.01-34.58)** | 2.59 (0.31-21.48) | |
| 12+ | 37 (66.1) | 19 (33.9) | 4.28 (1.14-16.01)* | 0.95 (0.13-6.70) | |
| Occupational | Housewife | 105 (79.5) | 27 (20.5) | 1 | 1 |
| Status | Merchant | 55 (72.4) | 21 (27.6) | 1.49 (0.77-2.86) | 0.81 (0.20-3.29) |
| Government Employed | 53 (53.0) | 47 (47.0) | 3.45 (1.94-6.14)*** | 4.30 (1.88-9.81)** | |
| History of Abortion | No | 197 (73.8) | 70 (26.2) | 1 | 1 |
| Yes | 16 (39.0) | 25 (61.0) | 4.40 (2.22-8.72)*** | 2.60 (0.97-6.96) | |
| Planned recent pregnancy | No | 90 (88.2) | 12 (11.8) | 1 | 1 |
| Yes | 123 (59.7) | 83 (40.3) | 5.06 (2.61-9.837)*** | 3.54 (1.45-8.67)** | |
| Previous ANC Visits | No | 53 (74.6) | 18 (25.4) | 1 | 1 |
| Yes | 53 (57.0) | 40 (43.0) | 2.22 (1.13-4.36)* | 1.52 (0.66-3.55) | |
| Autonomy on Healthcare Decision | Both | 96 (72.2) | 37 (27.8) | 1 | 1 |
| Woman | 13 (31.0) | 29 (69.0) | 5.79 (2.72-12.33)*** | 7.02 (2.00-24.60)** | |
| Husband | 104 (78.2) | 29 (21.8) | 0.72 (0.43-1.27) | 1.75 (0.75-4.05) | |
Significant at *P value <0.05, **P value <0.01 and ***P-value<0.001
Table 3: Factors associated with utilization of ANC among urban mothers who gave live birth within the past one year in Womberma woreda, Northwest Ethiopia, 2015 (n=308).
However, for rural residents’ age, gravidity, parity, history of abortion, planned recent pregnancy, previous antenatal care visit and had autonomy on health care decision making were found to be significantly associated with ANC utilization in the bivariate analysis. In the multiple logistic regressions gravidity didn’t show any significant association with ANC service utilization.
Rural mothers whose age was 30-34 years (AOR (95% C.I): 5.10 (1.75, 14.86)) and ≥35 years (AOR (95% C.I): 5.75 (2.06, 16.08)) were 5.10 and 5.75 times more likely to utilize ANC service compared to women below the age of 30 respectively. Rural mothers who gave birth more than two were 5.18 times more likely to utilize ANC services than who had two or one births (AOR (95% C.I): 5.18 (2.72, 9.83)) and mothers with planned recent pregnancy were 3.72 times more likely to utilize ANC service compared to those with no planned recent pregnancy (AOR (95% C.I): 3.72 (2.15, 6.45)).
Furthermore, rural mothers with a history of abortion were 6.01 times more to utilize the ANC service compared to mothers with no history of abortion (AOR (95% C.I): 6.01 (3.01, 11.64)), and had autonomy on health care decision making were 7.16 times more likely to utilize ANC service than where the decision is made by husband and both couples (AOR (95% C.I): 7.16 (2.42, 21.23)). Similarly, those rural mothers who had a previous history of ANC service utilization were 1.92 times more likely to utilize ANC services than their counterparts (AOR (95% C.I): 1.92 (1.16, 3.18)) (Table 4).
| Variable | Category | Utilization of ANC | COR (95% CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Yes n (%) | No n (%) | ||||
| Age Group | ≤24 years | 134 (81.2) | 31 (18.8) | 1 | 1 |
| 25-29 years | 145 (78.8) | 39 (21.2) | 1.16 (0.69-1.97) | 1.67 (0.59-4.7) | |
| 30-34 years | 48 (48) | 52 (52) | 4.68 (2.69-8.15)*** | 5.10 (1.75-14.86)** | |
| ≥35 years | 46 (35.1) | 85 (64.9) | 7.99 (4.70-13.58)*** | 5.75 (2.06-16.08)** | |
| Gravidity | 01-Feb | 229 (80.4) | 56 (19.6) | 1 | 1 |
| ≥3 | 144 (48.8) | 151 (51.2) | 4.29 (2.96-6.21)*** | 0.90 (0.34-2.41) | |
| Parity | 1-2 Child | 267 (77.2) | 79 (22.8) | 1 | 1 |
| ≥3 children | 106 (45.3) | 128 (54.7) | 4.08 (2.85-5.85)*** | 5.18 (2.72-9.83)*** | |
| History of abortion | No | 179 (63.7) | 102 (36.3) | 1 | 1 |
| Yes | 41 (35.7) | 74 (64.3) | 3.17 (2.02-4.98)*** | 6.01 (3.01-11.64)*** | |
| Planned recent pregnancy | No | 164 (79.2) | 43 (20.8) | 1 | 1 |
| Yes | 209 (56.0) | 164 (44.0) | 2.99 (2.02-4.43)*** | 3.72 (2.15-6.45)*** | |
| Previous ANC Visits | No | 147 (64.8) | 80 (35.2) | 1 | 1 |
| Yes | 74 (43.8) | 95 (56.2) | 2.36 (1.57-3.55)*** | 1.92 (1.16-3.18)* | |
| Autonomy on Healthcare Decision | Both | 318 (67.7) | 152 (32.3) | 1 | 1 |
| Woman | 22 (37.9) | 36 (62.1) | 3.42 (1.95-6.02)*** | 7.16 (2.42-21.23)*** | |
| Husband | 33 (63.5) | 19 (36.5) | 1.21 (0.66-2.19) | 1.69 (0.73-3.90) | |
Significant at *P value <0.05, **P-value <0.01 and ***p-value<0.001
Table 4: Factors associated with utilization of ANC among rural mothers who gave live birth within the past one year in Womberma woreda, Northwest Ethiopia, 2015 (n=580).
Discussion
In this study, even though the gap was small, mothers in urban areas had utilized antenatal care service than those mothers in rural areas. Mothers in rural areas of a higher age group, had three or more births, history of abortion, recent planned pregnancy, previous ANC visit and had autonomy on healthcare decision making were more likely to have antenatal care services. However, government employed mothers, had recent planned pregnancy and autonomy on health care decision making were more likely to utilize antenatal care services in urban centers.
Above three quarters of urban resident women had utilized antenatal care services in Womberma Woreda. However, this finding was slightly lower than the 2011 EDHS [3] and the 2014 Mini EDHS [9] of the country. In contrast to urban women’s ANC utilization, more rural mothers had utilized the service than the two EDHS studies, i.e., the 2011 [3] and 2014 [9]. The increase in service utilization in rural areas might be due to the increased availability of infrastructure, i.e., construction of health facilities and the shorter distance to this facilities, construction of roads and transportation access. In addition, this might be due to the fact that nowadays the government has given great attention in closing the gap on maternal health care services both in urban and rural areas though there is still a gap in utilizing the service.
Among urban resident women utilization of antenatal care service was significantly associated and higher among mothers who were 30 years and older. This finding was supported by a study done in Jimma town as age of women was significantly associated with utilization of antenatal care services [26]. This might be due to as the age of the mother advances, they might have a better knowledge and experience of pregnancy, and pregnancy complications might be more severe in the later ages of women influencing them to use the service
Rural mothers who gave three or more births were more likely to utilize antenatal care services than their counterparts. This finding was supported by another study done in rural areas of India where women who had one or more births utilized the service than those who had any live births [27]. This might be due to the fact that women with a higher parity might faced previous pregnancy and birth complications. In addition, they might have previous antenatal visits which might motivate them to use the service for the other time.
Rural residents of the study area, women who had utilized ANC for their previous pregnancy were more likely to utilize antenatal care services than those who had no previous ANC visit. It is evident that a positive and constructive patient and health care provider interaction improves patient compliance with health care services [28,29]. This might be due to the fact that health care providers might provide necessary information and advice about the importance of attending antenatal care, thereby enhancing women’s knowledge, promoting their empowerment or autonomy to make informed health care decisions and achieve better antenatal care compliance.
Moreover, rural mothers who had a history of abortion were more likely to utilize the antenatal care service compared to those who had no history of abortion. Similarly, mothers who considered pregnancy as a risky event were utilizers of the service [11]. This might be because of the perceived risk of losing their pregnancy and the complications associated with it. Furthermore, mothers with a history of abortion might feel that their abortion was related to poor utilization of ANC service.
Both mothers in rural and urban areas where their recent pregnancies were planned were more likely to utilize antenatal care services than those who had no planned pregnancies. This finding was supported by other studies done in Ethiopia as those women who had planned and wanted pregnancy were more likely to utilize the ANC service than those who had unplanned and unwanted pregnancy [11,24]. The possible justification for this finding might be due to the fact that mothers who plan to have a child might want to have a healthy pregnancy and its outcome and thus they might give a great attention for antenatal care service.
In this study, both urban and rural women who are able to decide on spending their self ’s healthcare were more likely to utilize antenatal care services than those women where the decision was made by both the couple and/or their husband only. This finding was supported by another study where women’s autonomy on health care spending was found to have a significant association with the utilization of antenatal care services [30]. Women’s decision making power can have a significant effect on their ability to seek healthcare and/or even delay in accessing and receiving the services where they are readily available [31]. This might be due to when resources are controlled by others; women might not have the freedom to use the service whenever they need it. Moreover, autonomy might be related to women’s education and occupation as both of which are factors that might increase the likelihood of the use of antenatal care services.
Urban women who were government employed were more likely to use antenatal care service than those who were housewives and merchants. Similarly, women who had a job were more likely to use the ANC services [30]. Women who are employed and working earned money, they might have a better understanding of the ANC and thus they can have the economic ability to pay for the service.
Strength and limitations of the study
Being a comparative community based study done among urban and rural women who gave birth in the past one year explored the different independent variables made it strong. However, due to its cross-sectional nature of the study, it is difficult to establish causal relationship between the dependent and independent variables. In addition, it was not a mixed method study where the qualitative study will try to explore in-depth reasons why women didn’t utilize the service.
Conclusion
The level of antenatal care service utilization among mothers who gave live birth in the past one year, both in urban and rural areas of Womberma Woreda was found to be very low as per government need. Despite the gaps of ANC service utilization among urban and rural residents was getting close, still the degree of utilization across residence is still there. In this study occupation of the mother, had a planned recent pregnancy and autonomy in health care decision making in urban area and age of mothers, parity, had a history of abortion, planned recent pregnancy, previous ANC visit and autonomy in health care decision making in rural areas were found to be significantly associated with antenatal care service utilization. It is well documented that antenatal care has the potential in reducing maternal morbidity and/or mortality and in improving newborn’s health. Inadequate as well as late few antenatal care visits are related with poor pregnancy outcome and are less likely to be assisted by a skilled birth attendant during childbirth. Therefore, each and every pregnant mother should receive the recommended WHO antenatal care visits as it is important in identifying risk factors for adverse pregnancy outcomes, both for the mother and the newborn and in providing preventive and promotive health services.
Authors Information
Getasew Mulat earned an MPH, in 2015, from Joint MPH program, i.e., GAMBY College of Medical Sciences and Debre Markos University, College of Medicine and Health Sciences. He is working at Womberma Woreda Health Office, West Gojam Zone, Shindy Town, Ethiopia.
Teketo Kassaw earned an MPH, in 2013, from Addis Ababa University, College of Health Sciences, School of Public Health and lecturer at Debre Markos University, College of Medicine and Health Sciences, Public Health department.
Mekonnen Ayichiluhm Bishaw from GAMBY College of Medical Sciences, Bahir Dar, Ethiopia.
Acknowledgement
We would like to appreciate and thank Joint MPH program, GAMBY College of Medical Sciences and Debre Markos University for technical support. We would like to thank our data collectors and the supervisors for their invaluable effort; without them this study would not have come to be completed. Our deep gratitude also goes to our study participants who volunteered and took their time to give us all the relevant information for the study. Last but not least, we would like to thank the Womberma Woreda Health Office for their cooperation and help during the data collection.
Authors Contributions
Getasew Mulat wrote the proposal, participated in data collection, analyzed the data and drafted the paper. Mekonnen Ayichiluhm and Teketo Kassaw approved the proposal with some revisions, and participated in data analysis. Teketo Kassaw had written the manuscript. We revised drafts of the paper. All authors read and approved the final manuscript.
Funding
Funding and consideration for this study was provided by the Nigerian Federal Ministry of Health.
References
- Accorsi S, Bilal NK, Farese P, Racalbuto V (2010) Countdown to 2015: comparing progress towards the achievement of the health Millennium Development Goals in Ethiopia and other sub-Saharan African countries. Trans R Soc Trop Med Hyg 104: 336-342.
- Trends in Maternal Health in Ethiopia (2012) Challenges in Achieving the MDG for Maternal Mortality. In-depth Analysis of the EDHS 2000-2011. United Nations Population Fund (UNFPA), December 2012 Addis Ababa.
- Â (2012) Central Statistical Agency [Ethiopia], ICF international: Ethiopia demographic and health survey 2011. Addis Ababa, Ethiopia and Calverton, Maryland, USA: Central statistical agency and ICF international.
- Federal Ministry of Health in Ethiopia (2010) Annual Performance Report 2002 EFY (2009/2010). Addis Ababa: Federal Ministry of Health.
- Federal Ministry of Health in Ethiopia (2012) Health extension programme implementation guidelines. Addis Ababa: Federal Ministry of Health; 2011/12.
- Â (2013) Federal Ministry of Health N (FMoH). National HIV/AIDS and Reproductive Health and Serological Survey, 2012 (NARHS Plus). Abuja, Nigeria: Federal Ministry of Health; 2013.
- Lincetto O, Mothebesoane-anoh S, Gomez P, Munjanja S (2010) Antenatal Care: Opportunities for Africaâ™ Newborns.
- (2014) National Population Commission (Nigeria) and ICF International: Nigeria Demographic and Health Survey 2013. Abuja, Nigeria.
- Central Statistical Agency [Ethiopia]. 2014. Ethiopia Mini Demographic and Health Survey 2014. Addis Ababa, Ethiopia.
- Tsegay Y, Gebrehiwot T, Goicolea I, Edin K, Lemma H, et al. (2013) Determinants of antenatal and delivery care utilization in Tigray region, Ethiopia: a cross-sectional study. Int J Equity Health 12: 30.
- Abosse Z, Woldie M, Ololo S (2010) Factors influencing antenatal care service utilization in hadiya zone. Ethiop J Health Sci 20: 75-82.
- Ajayi IO, Osakinle DC (2013) Socio demographic factors determining the adequacy of antenatal care among pregnant women visiting ekiti state primary health centers. Authors. Online J Heal Allied Sci 12: 1-6.
- Arthur E (2012) Wealth and antenatal care use: implications for maternal health care utilisation in Ghana. Health Econ Rev 2: 14.
- Dairo M, Owoyokun KE (2010) Factors affecting the utilization of antenatal care services in Ibadan, Nigeria. Benin J Postgrad Med 12:1-6.
- Vecino-Ortiz AI (2008) Determinants of demand for antenatal care in Colombia. Health Policy 86: 363-372.
- Gage AJ (2007) Barriers to the utilization of maternal health care in rural Mali. Soc Sci Med 65: 1666-1682.
- Omo-Aghoja LO, Aisien OA, Akuse JT, Bergstrom S, Okonofua FE (2010) Maternal mortality and emergency obstetric care in Benin city south-south Nigeria. J Clin Med Res 2: 55-60.
- Titaley CR, Dibley MJ, Roberts CL (2010) Factors associated with underutilization of antenatal care services in Indonesia: results of Indonesia Demographic and Health Survey 2002/2003 and 2007. BMC Public Health 10: 485.
- Fagbamigbe AF, Idemudia ES (2015) Barriers to antenatal care use in Nigeria: evidences from non-users and implications for maternal health programming. BMC Pregnancy Childbirth 15: 95.
- Alam AY, Qureshi AA, Adil MM, Ali H (2004) Factors affecting utilization of Antenatal Care among women in urban slum areas of Islamabad. Rawal Med J 29: 71-75.
- Rahman M, Islam R, Islam AZ (2008) Rural-urban differentials of utilization of antenatal health care services in Bangladish. Health Policy and development, 6.
- (2014) Womberma Woreda Health Office Annual Health Service Delivery Report 2014.
- Berhe KK, Welearegay HG, Abera GB, Kahsay HB, Kahsay AB (2014) Assessment of Antenatal Care Utilization and its Associated Factors Among 15 to 49 Years of Age Women in Ayder Kebelle, Mekelle City 2012/2013; A Cross Sectional Study. American Journal of Advanced Drug Delivery, 2.
- Regassa N (2011) Antenatal and postnatal care service utilization in southern Ethiopia: a population-based study. Afr Health Sci 11: 390-397.
- Fekede B, Mariam A (2007) Antenatal care services utilization and factors associated in Jimma Town (south west Ethiopia). Ethiop Med J 45: 123-133.
- Chandhiok N, Dhillon BS, Kambo I, Saxena NC (2006) Determinants of antenatal care utilization in rural areas of India: A cross-sectional study from 28 districts (An ICMR task force study). J Obstet Gynecol India 56:47-52.
- Ciccone MM, Aquilino A, Cortese F, Scicchitano P, Sassara M, et al. (2010) Feasibility and effectiveness of a disease and care management model in the primary health care system for patients with heart failure and diabetes (Project Leonardo). Vascular Health and Risk Management 6:297-305.
- Cecere A, Scicchitano P, Zito A, Sassara M, Bux F, et al. (2014) Role of Care Manager in Chronic Cardiovascular Diseases. Ann Gerontol Geriatric Res 1: 1005.
- Tarekegn SM, Lieberman LS, Giedraitis V (2014) Determinants of maternal health service utilization in Ethiopia: analysis of the 2011 Ethiopian Demographic and Health Survey. BMC Pregnancy Childbirth 14: 161.
- Ahmed S, Creanga AA, Gillespie DG, Tsui AO (2010) Economic status, education and empowerment: implications for maternal health service utilization in developing countries. PLoS One 5: e11190.
Citation: Mulat G, Kassaw T, Aychiluhim M (2015) Antenatal Care Service Utilization and its Associated Factors among Mothers who Gave Live Birth in the Past One Year in Womberma Woreda, North West Ethiopia. Epidemiology (sunnyvale) S2:003. DOI: 10.4172/2161-1165.S2-003
Copyright: © 2015 Mulat G, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 20223
- [From(publication date): 0-2015 - Sep 03, 2025]
- Breakdown by view type
- HTML page views: 14747
- PDF downloads: 5476