Bleeding after Gastric Bypass Surgery: The Possibility of using of Postoperative Balloon Enteroscopy
Received: 07-Feb-2017 / Accepted Date: 22-Dec-2017 / Published Date: 28-Dec-2017 DOI: 10.4172/2161-069X.1000545
Abstract
In the majority of cases late postoperative bleedings are intraluminal ones, showing clinical manifestations of high gastrointestinal hemorrhage. Among all bariatric procedures, this complication develops more commonly after Rouxen- Y gastric bypass. The most likely cause of such bleedings being peptic ulcer, conservative therapy with proton pump inhibitors is well justified at the initial stages of treatment. Upper endoscopy is the treatment of choice for bleeding ulcers localized in the pouch and 80% of bleedings in the pouch or gastroenteroanastomosis can be controlled in this way.
If the bleeding is localized in the remnant stomach or duodenum and small intestine, more advanced endoscopic procedures are needed. Balloon enteroscopy is one of such techniques, although its efficacy in the treatment of bleeding resulting from biliopancreatic limb is extremely variable and depends mainly on specialist’s skills, length of intestinal loop as well as severity of adhesions in the abdominal cavity. The article describes our experience of enteroscopy used to control bleeding from duodenal ulcer after Roux-en-Y gastric bypass intervention.
Keywords: Roux-en-Y gastric bypass; Postoperative bleeding; Gastrointestinal bleeding; Balloon enteroscopy; Peptic ulcer
Introduction
Roux-en-Y gastric bypass (RYGB) is an effective way of obesity surgical treatment. This method is rightfully considered to be one of the leading bariatric techniques carried out today. Like any other surgical intervention, RYGB is associated with possible complications and many of them may become life threatening. Postoperative bleeding is one of such complications, its prevalence being cited as 1-4% [1-4].
Publications show a little higher risk of postoperative bleeding in laparoscopic aproach (1.9%) as compared to open surgery (0.6%) [3-6]. Bleedings after surgery can be specified as early ones developing before the 30th postoperative day and late ones-after the 30th postoperative day [1,2,7]. Besides, they can be intraluminal and intraabdominal. The latter have no significant difference from postoperative bleedings after various abdominal surgical interventions.
In contrast, intraluminal bleedings are of special interest. The changed interaction of anatomical structures essentially aggravates the verification of bleeding source and in certain cases requires quite different diagnosis approach in this cohort of patients. Moreover, such patients are frequently admitted to emergency hospitals where surgeons not conducting bariatric interventions routinely may be rather unfamiliar with technical issues of previous surgery. All mentioned above makes it crucial to discuss diagnosis approach in patients with suspected gastrointestinal bleeding after gastric bypass surgery.
Case Report
Patient S, aged 44, underwent laparoscopic RYGB in one of Saint Petersburg clinics in October 2014. At baseline his BMI was 43 kg/m2 and he had type 2 diabetes mellitus, taking oral antihyperglycemic medications. At one year follow-up postoperatively his % EWL was 81%. He had compensated type 2 diabetes mellitus (HbA1 4.9%), no therapy needed. On 23.01.2016 the patient was brought by ambulance to one of city surgical clinics with gastrointestinal bleeding, complaining of weakness, dizziness and fainting episode after defecation. For the previous week he occasionally had had black stool but did not pay attention to it. The patient presented with hemoglobin 88 g/l, erythrocyte count 2.81 × 1012 and hematocrit rate 25.3%. Upper endoscopy showed insignificant anastomositis without signs of bleeding or stenosis.
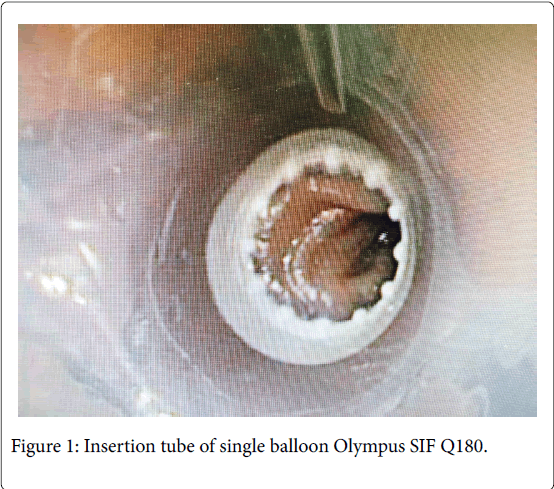
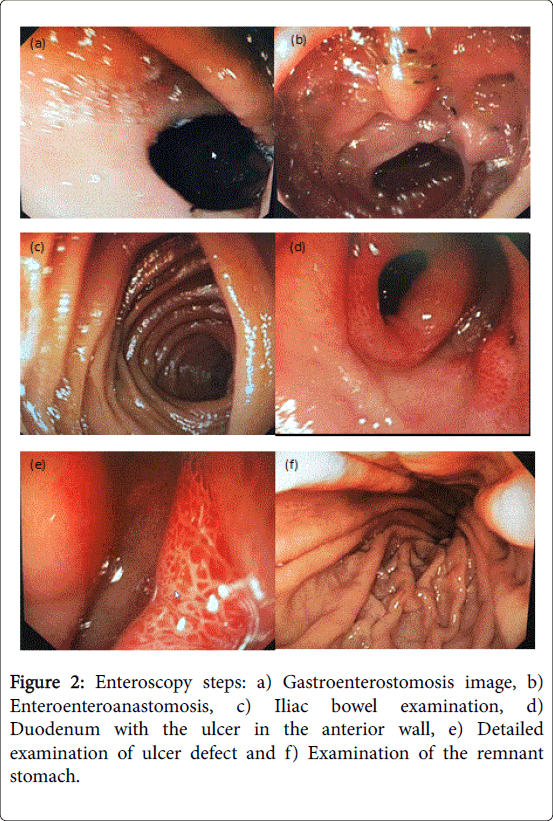
On complete rectal colonoscopy pale mucous membrane and impaired vascular pattern of the bowel were seen. Abnormal lesions were not revealed. Endoscopic examination showed signs of colonic mucosal anemia and internal hemorrhoids without exacerbation. In the hospital the patient was administered haemostatic and gastroprotective therapy as well as blood component transfusion. There was no evidence of any persisting bleeding. The condition of the patient was stabilized and on 29.01.2016 he was transferred to Nikiforov Russian Center of Emergency and Radiation Medicine to verify the source of bleeding. On 2.02.2016 under general anesthesia, enteroscopy was carried out with the use of Olympus SIF-Q180. The evaluation showed the stomach pouch to be of small size, well insufflated by air and having pink mucous membrane (Figures 1 and 2).
Gastroenteroanastomosis proved to be elastic, easily passable. Alimentary intestinal loop demonstrated no abnormality. At the distance of more than 1 m from gastroenteroanastomosis, side-to-side enteroenteroanastomosis was easily passable with no signs of obstruction. Distal 2.5 m deep evaluation of the small intestine revealed no abnormality. Proximal evaluation of the small intestine, duodenum and unchanged remnant of the stomach was performed. On the anterior wall of the duodenal bulb, 1.0 cm cicatrizing ulcer without any signs of bleeding was found.
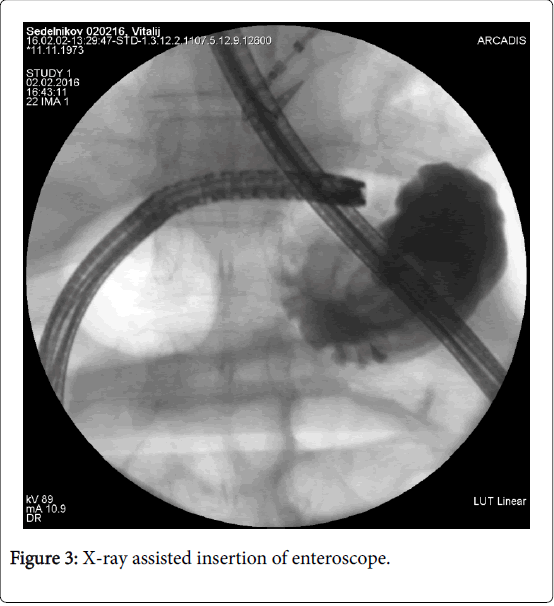
Next day the patient was discharged and his condition was satisfactory. Gastroenterologist follow-up was recommended. Antiulcer therapy was administered. During follow-up period there was no recurrence of bleeding (Figure 3).
Discussion
Publications show the proportion of early postoperative bleedings among all bleedings after RYGB to vary from 53% to 73.7% [1,7]. As a rule, these are intraabdominal bleedings which develop for the first 24 hours after surgery. The most common source of early bleedings is revealed in the stapling area: 40% in the stapling line of the remnant stomach, 30% in gastrojejunoanastomosis and 30% in the area of jejunojejunal junction. Much less frequently, the bleedings are caused by iatrogenic injuries of the liver and spleen or trocar wounds. The majority of late postoperative bleedings are intraluminal [5,7]. They may develop several months and even years after surgery, being most commonly caused by ulcers in gastrojejunoanastomosis or the remnant stomach and duodenum [1,4,6,7]. In late postoperative period about 20% of patients develop ulcers [8,9].
Pathophysiological mechanisms of such ulcer occurence still remain not completely studied but most probable factors responsible are ischemia, the impact of hydrochloric acid, the response to foreign bodies (sutures and staples) as well as the tension of tissues in the area of formed anastomoses [7,9]. The choice of treatment approach in patients with gastrointestinal bleeding depends largely on the character and timing of clinical manifestations. The bleeding which starts 6 hours postoperatively and is accompanied by hematocrit rate reduction is usually the evidence of continuous bleeding, in most cases requiring urgent surgical intervention. On the contrary, if gastrointestinal bleeding occurs 48 hours after surgery and hematocrit rate is not significantly changed there is no need for active surgical manipulations [3,5].
Diagnosis and treatment activities are determined by the character of clinical manifestations in gastrointestinal bleeding. They may be just limited by proton pump inhibitors administration and observing the patient for any changes in his condition or perhaps blood component transfusion, diagnosis and treatment endoscopy as well as active surgical intervention will be needed [1,7].
At the early stages of gastrointestinal bleeding diagnosis, the use of upper endoscopy proved to be of doubtless value. Simultaneously, one can perform endoscopic hemostasis and evacuate blood clots, when the source of bleeding is found in the area of the pouch or gastroenteroanastomosis. However, if the source is not verified by upper endoscopic evaluation, selecting further management could be difficult. Bleeding ulcers localized in the remnant stomach, duodenum and in the area of gastroenteroanastomosis could not be visualized with conventional endoscopy. Several diagnosis and treatment techniques are available for such cases, namely, the use of pediatric colonoscope with retrograde insertion through jejunojejunoanastomosis [7,10], Tc-99m labeled erythrocyte scintigraphy [10-12], angiography [6,10] percutaneous or laparoscopical gastrostomy followed by endoscope or bronchoscope introduction into the stomach [1,7,10,11] and single or double balloon enteroscopy [1,6,11].
The two latter techniques are especially noteworthy. Being low invasive and of high diagnosis and treatment value, enteroscopy is quite reasonable in cases when conventional upper endoscopy fails to verify the source of bleeding [6,11]. However, this technique requires the use of expensive equipment and should be conducted by the team of experienced endoscopist and bariatric surgeon. Moreover, its use is limited in cases of profuse bleeding accompanied by unstable hemodynamics. Many authors consider gastrostomy either through laparoscopic or open surgical access followed by gastroduodenoscopy of the intestinal loop to be a reasonable modality in such cohort of patients [1,2,10,11,13].
Conclusion
In those patients who underwent RYGB with suspected gasrointestional bleeding the management approach should be determined first of all depending on the extent of hemodynamic disorder caused by blood loss. Upper endoscopy seems to be quite reasonable at the early stages of diagnosis in patients with signs of gastrointestinal bleedings. When the symptoms of blood loss are rapidly aggravated and upper endoscopy fails to reveal the source of bleeding, urgent laparoscopic or open gastrostomy followed by transgastric endoscopic examination is indicated. Patients who are difficult to diagnose, without the signs of persisting or intensive bleeding and with stable hemodynamics should be transferred to hospitals specializing and experienced in bariatric surgery, having adequate equipment and trained personnel to perform advanced endoscopic manipulations. Enteroscopy carried out by an experienced endoscopist enables to verify the source of bleeding in the remnant stomach and biliopancreatic limb, to control bleeding and avoid highly invasive surgical interventions.
References
- Rabl C, Peeva S, Prado K (2011) Early and late abdominal bleeding after Roux-en-Y gastric bypass: Sources and tailored therapeutic strategies. Obes Surg 21: 413-420.
- Dick A, Byrne TK, Baker M (2010) Gastrointestinal bleeding after gastric bypass surgery: Nuisance or catastrophe? Surg Obes Relat Dis 6: 643-647.
- Nguyen NT, Longoria M, Chalifou S (2004) Gastrointestinal hemorrhage after laparoscopic gastric bypass. Obes Surg 14: 1308-1312.
- Subhani M (2012) Endoscopic evaluation of symptomatic patients following bariatric surgery: A literature review. Diagn Ther Endosc 2012: 1-8.
- Acquafresca PA, Palermo M, Rogula T (2015) Early surgical complications after gastric by-pass: A literature review. Arq Bras Cir Dig 28: 74-80.
- Sharma A (2015) A case report on complicated bleeding in a patient post Roux-en-Y gastric bypass. Gen Med (Los Angel) 3: 3.
- Heneghan HM, Meron-Eldar S, Yenumula P (2012) Incidence and management of bleeding complications after gastric bypass surgery in the morbidly obese. Surg Obes Relat Dis 8: 729-735.
- Kumar N, Thompson CC (2013) Endoscopic management of complications after gastrointestinal weight loss surgery. Clin Gastroenterol Hepatol 11: 343-353.
- Siddique SS, Feuerstein JD (2014) Gastrointestinal complications of Roux-en-Y gastric bypass surgery. OA Minimally Invasive Surg 2: 1.
- Zerey M, Sigmon LB, Kuwada TS (2008) Bleeding duodenal ulcer after Roux-en-Y gastric bypass surgery. JAOA 108: 25-27.
- Kitamura RK (2015) The management of GI bleeding after gastric bypass surgery. Int J Surg Res Pract 2: 2.
- Mehran A, Szomstein S, Zundel N, Rosenthal R (2003) Management of acute bleeding after laparoscopic Roux-en-Y gastric bypass. Obes Surg 13: 842-847.
- Braley SC, Nguyen NT, Wolfe BM (2002) Late gastrointestinal hemorrhage after gastric bypass. Obes Surg 12: 404-407.
Citation: Solovyeva MO, Velikorechin AS, Dvoryankin DV, Machs VM (2017) Bleeding after Gastric Bypass Surgery: The Possibility of using of Postoperative Balloon Enteroscopy . J Gastrointest Dig Syst 7: 545. DOI: 10.4172/2161-069X.1000545
Copyright: © 2017 Solovyeva MO, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7612
- [From(publication date): 0-2017 - Dec 13, 2025]
- Breakdown by view type
- HTML page views: 6713
- PDF downloads: 899