Brief Review Notes on Neuroinflammation and Arthritis Crosstalk: Theoretical Developments
Received: 01-Feb-2023 / Manuscript No. ijrdpl-22-84601 / Editor assigned: 03-Feb-2023 / PreQC No. ijrdpl-22-84601 / Reviewed: 17-Feb-2023 / QC No. ijrdpl-22-84601 / Revised: 21-Feb-2023 / Manuscript No. ijrdpl-22-84601 / Accepted Date: 27-Feb-2023 / Published Date: 28-Feb-2023 QI No. / ijrdpl-22-84601
Abstract
The chronic inflammatory illness rheumatoid arthritis (RA) is characterised by erosive polyarthritis. RA is connected with neuropsychiatric comorbidities such as depression, anxiety, and an increased risk of developing neurodegenerative disorders later in life. Studies of the central nervous system (CNS) in preclinical models of rheumatoid arthritis (RA) have contributed to the comprehension of the close interplay between peripheral and central immune responses. This mini-review outlines the current understanding of CNS comorbidity in RA patients and the known cellular processes
driving this condition.
Keywords
Rheumatoid arthritis; CNS; Neurodegenerative disorders
Introduction
The blood-brain barrier has been thought to shield the central nervous system (CNS) from circulatory inflammatory signals for a long time (BBB). A multitude of neurological and psychiatric consequences associated with chronic inflammatory illnesses such as rheumatoid arthritis, however, demonstrate an intimate interaction between chronic peripheral inflammation and the CNS (RA). RA is a systemic autoimmune disease characterised by inflammation of the synovium and deformity of the joints and surrounding bones. The pathogenesis of rheumatoid arthritis is driven by a complicated interaction between T-cells, autoantibodies, and innate immune components such as myeloid cells and proinflammatory cytokines [1-3]. Patients with RA have a greater propensity to acquire mental comorbidities. The estimated prevalence of major depressive illness in RA patients is 16.8 percent, which is much higher than the overall population [4, 5]. In addition, RA patients have elevated levels of anxiety [6] and cognitive impairment [5] compared to healthy persons. In addition, about 40 percent of RA patients suffer from chronic pain, which is associated with melancholy and anxiety (9). Intriguingly, midlife RA was associated with a 2.5-fold higher risk of developing dementia after 21 years of follow-up. Epidemiological research on the relationship between RA and certain neurological disorders, such as Alzheimer's disease (AD) and Parkinson's disease (PD), have produced inconsistent findings (11–16). Nonetheless, RA therapies that block pathogenetic pro-inflammatory cytokines such as tumour necrosis factor (TNF) and interleukin-6 (IL-6) ameliorate symptoms such as sadness and anxiety. And have been associated with a decreased risk of future neurodegeneration in RA patients. While precise pathological mechanisms underlying CNS involvement in RA are currently under investigation, the majority of our current understanding of the propagation of peripheral inflammation into the CNS and subsequent impairment of neural function is derived from animal models of acute infection induced by administration of lipopolysaccharide (LPS) or polyinosinic-polycytidylic acid (Poly(I:C)). By the infiltration of bloodderived immune cells or the inflammatory stimulation of endothelial cells, peripheral inflammatory mediators may reach the CNS via the BBB or the choroid plexus in this situation. Additionally, astrocytes and CNS-associated myeloid cells acquire an inflammatory state, including parenchymal microglia, meningeal, perivascular, and choroid plexus macrophages. Inducing neuronal injury, decreased adult hippocampal neurogenesis, and altered neurotransmitter signalling , neuroinflammation may eventually be the cause of neuropsychiatric symptoms.
Problem statement
Osteoarthritis (OA) is a degenerative disease of the joints that affects cartilage and surrounding tissues. Typically, the condition proceeds slowly, but it may ultimately lead to joint failure, degeneration, discomfort, and even paralysis [1]. It is distinguished by the localised region of articular cartilage loss in synovial joints and its associated symptoms, which include osteophyte development, subchondral bone alterations, and synovitis [2]. The risk of knee and hip illnesses is elevated, followed by broad lower limb, hand OA, and knee and hip disorders [3]. Pain, stiffness, joint deformity, and cracking are the most prominent symptoms [4]. OA affects women more than males, and its prevalence rises with age [5]. Consequently, it is regarded as the most prevalent chronic joint condition [6]. OA is also the major cause of disability, and its prevalence is rising [4]. Joint degeneration occurs in the majority of instances; however, the risk of OA rises with age, joint loading, joint deformities, and crashes. In addition, the condition is associated with bone marrow edema, synovitis, and joint effusion. Consequently, OA, as a prevalent complicated illness, represents a significant public health burden. Studies indicate that exercise treatment may successfully alleviate pain in people with osteoarthritis (OA) of the hip or knee, but the expense is significant. Generally, nonsurgical treatment is the best option, with a focus on lifestyle modifications, weight reduction, and exercise, supplemented with pharmacological therapy (12). In addition, conservative OA-specific treatment may lower the risk of surgery and improve pain and function in individuals with hip or knee OA. In addition to surgery, standard therapies for severe OA include pain-relieving nonsteroidal anti-inflammatory medications, anaesthetic and non-anaesthetic (limp) analgesics, and physiotherapy. Viscoelastic injections of hypertonic acid (HA) are often utilised for the local therapy of osteoarthritis (OA) .The possible inflammatory effect of OA results in the loss of chondrocytes, hence lowering the cartilage layer in the joint. Compounds with anti-inflammatory characteristics are possible OA treatments. Several studies have shown that etoxib has a positive impact on OA inflammation and a low frequency of adverse effects. Collagen hydrolysate is a possible treatment for osteoarthritis and osteoporosis . However, these medications can only relieve moderate OA and have little impact on conditions needing surgery that are more severe. Therefore, it is of utmost significance to determine ways to alleviate the clinical symptoms of severe OA patients using non-surgical means. Multiple disorders, including rheumatoid arthritis (RA), inflammatory bowel disease (IBD), and colorectal cancer (CRC), are caused by dysregulation of the hypoxia and inflammation pathways. Recent scientific study has thus focused on seeking to comprehend how these pathways are controlled, interact, and react to illness.
Review Analysis
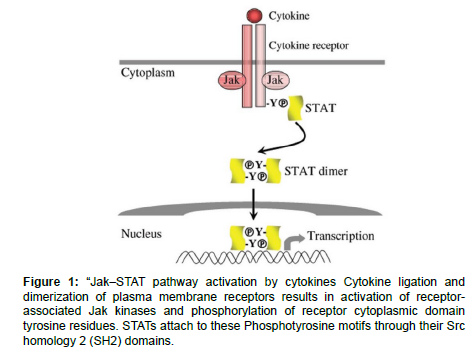
Cytokines are released proteins that facilitate communication between cells. Cytokines accomplish their biological roles by binding with high affinity and specificity to cell-surface receptors, therefore initiating signal transduction cascades that control cellular activation, proliferation, differentiation, and survival. Gene activation or repression is mediated through the Janus kinase (Jak)–signal transducer and activator of transcription (STAT) signalling pathway in the majority, if not all, cytokines. The Jak–STAT pathway was discovered as a result of research into methods of gene regulation by interferons (IFNs). Numerous IFN-inducible genes exhibited fast and independent transcriptional activation, showing that IFNs triggered transcription by altering the activity of existing proteins and transcription factors. The Jak–STAT signalling pathway has since been identified by tests conducted in several labs. Protein tyrosine kinases known as Jaks are pre-associated with the membrane-proximal domains (box 1 and box 2) of cytokine receptors. Only four mammalian Jaks seem to exist: Jak1, Jak2, Jak3, and Tyk2. At the carboxy terminus of each protein is a catalytically active kinase domain and a regulatory pseudo kinase domain. The region responsible for Jaks receptor binding is situated at the amino terminus. The binding of cytokine ligands leads in the dimerization of receptor subunits, which increases the local concentration of Jaks and brings these kinases close together. In response to tyrosine phosphorylation, the Jaks become activated and launch the signal transduction cascade by phosphorylating tyrosine motifs found in receptor cytoplasmic domains and receptor-associated proteins. Phosphotyrosine-containing motifs in the cytoplasmic domains of receptors serve as docking sites for several signalling proteins, such as STATs (Figure 1). Receptor-associated proteins that are activated by Jaks include kinases that activate signalling pathways that are parallel to but separate from the Jak–STAT pathway. However, it is believed that Jaks is at the apex of the signalling cascade and are essential for all cytokine signal transduction through type I and type II cytokine receptors. In certain instances, Jak expression is essential for the proper expression of receptors on the cell surface, and therefore Jaks may play both a structural and catalytic function in signal transduction. A few minutes after receptor ligation, transcriptional responses may be identified. Utilizing a restricted number of proteins: protein or protein: DNA interactions between the extracellular ligand and gene promoters enable the selectivity of signal transduction. Jak, Janus kinase; STAT, signal transducer and activator of transcription.” Multiple cytokines, including IL-6, IL-10, and IFN-/, may activate STAT3 because of its pleiotropy. Because STAT3 is critical for the early development of mouse embryos, conditional gene targeting has been used to determine the biological role of STAT3 in many organs and cell types. In bone marrow progenitor cells, STAT3 controls granulopoiesis adversely. During haematopoiesis, deletion of STAT3 leads to anomalies in myeloid cells, overactivation of innate immune responses, and pathophysiology resembling inflammatory bowel disease. STAT3 is essential for IL-6-mediated inhibition of apoptosis in T cells and promotes proliferation through this mechanism. By upregulating the expression of IL-2R , a component of the high-affinity IL-2 receptor, STAT3 is also essential for effective IL-2-induced T cell proliferative responses. In contrast to its pro-immune action in T cells, deletion of STAT3 in myeloid cells leads to hyperactivation of macrophages, significant increases in inflammatory cytokine production, and inflammatory bowel disease, demonstrating the immunosuppressive and anti-inflammatory function of STAT3 in the myeloid lineage. The hyperactive phenotype of these animals implies that the in vivo activity of STAT3 in macrophages and neutrophils is to mediate the anti-inflammatory effects of IL-10, since the response to IL-10 was entirely abrogated in STAT3-deficient macrophages and neutrophils. Chronic enterocolitis in myeloid cell-specific STAT3- null rats may occur from the overproduction of IL-12 caused by Tolllike receptor 4 (TLR4) signalling, indicating a function for STAT3 in coordinating innate and adaptive immunity. In addition, a recent study demonstrates that STAT3 signalling in antigen-presenting cells is necessary for the generation of antigen-specific T cell anergy and, therefore, immunological tolerance , shedding cuulighter on the immune regulatory role of STAT3. In addition to immune system cells, the STAT3 gene has been conditionally silenced in keratinocytes, epithelial cells, endothelial cells, mammary gland cells, and motor neurons. Deletering STAT3 from keratinocytes demonstrates that STAT3 is important for skin remodelling and wound healing. STAT3 is essential for the death of epithelial cells necessary for proper mammary gland involution, in contrast to its anti-apoptotic activity in T cells and likely fibroblasts. Consequently, depending on the cell type and circumstance, STAT3 may either promote apoptosis or survival. The observation that the injection of a constitutively active version of STAT3 is sufficient for cellular transformation supports a causal role for STAT3 in oncogenesis. This discovery, in conjunction with the fact that constitutive activation of STAT3 has been observed in human cancer cells, highlights the significance of STAT3 in cancer. Collectively, the actions of STAT3 are complicated since, depending on cell type and activation level, STAT3 may have conflicting effects on distinct cells.
Figure 1: “Jak–STAT pathway activation by cytokines Cytokine ligation and dimerization of plasma membrane receptors results in activation of receptorassociated Jak kinases and phosphorylation of receptor cytoplasmic domain tyrosine residues. STATs attach to these Phosphotyrosine motifs through their Src homology 2 (SH2) domains.
Reprogramming of cytokine signalling
Not only may the amount of signal transduction be favourably or negatively controlled, but the character of cytokine responses can also be changed or reprogrammed, according to an emerging idea in Jak–STAT signalling. Consequently, the precise cellular response to a cytokine is dictated by the existence of a specific stimulus and the milieu to which the cells are exposed. The reprogramming of IL-10 signalling by IFN- and IFN- is one such example. In myeloid cells, IL-10 is a poor activator of STAT1 and does not generally stimulate STAT1 target genes, but IFN- does. Pre-exposure to type I IFNs reprograms STAT activation by IL-10 in such a way that STAT1 is preferentially activated by IL-10 in these cells, leading in the stimulation of a set of STAT1- dependent genes and an increase in inflammatory activity. IFN- is also capable of switching the ratio of IL-10 STAT activation from STAT3 to STAT1, accompanied by downregulation of STAT3-dependent gene expression and partial attenuation of IL-10 anti-inflammatory action. The reprogramming of IL-10 signalling by IFN- and IFN- may involve different processes. It seems that IFNs function as a switch that quickly controls STAT activation by IL-10 and modifies macrophage responses to IL10. Dynamic regulation of the activation of different STATs by the same cytokine provides a mechanism for cells to integrate and balance signals delivered by opposing cytokines, and extends our understanding of cross regulation by opposing cytokines to include reprogramming of signalling and modification of function. In, positive and negative regulation pathways of IFN signalling are shown schematically.
Endogenous inhibitors of MMPs
There are several endogenous MMP inhibitors, which limit activity and prevent excessive proteolysis (Table 1). The tissue inhibitors of metalloproteinase (TIMPs) are the most selective of these inhibitors for the MMPs. The TIMPs are a family of secreted proteins that may bind all MMPs in a 1:1 stoichiometry with different affinities; TIMP- 1 binds to MMP-9 with great affinity, whilst TIMP-2 inhibits MMP- 2 more effectively. The N- and C-terminal domains of TIMPs (21 to 29 kDa) are composed of 125 and 65 amino acids, respectively, and each contains three conserved bisulfide linkages. The N-terminal domain is capable of blocking MMPs and folds as a distinct unit. 2- macroglobulin is the primary inhibitor of MMPs in tissue fluids. The restricted proteolysis of a bait area of the plasma protein by an MMP generates a conformational shift in the macroglobulin, which then envelops the enzyme. It is a generic proteinase inhibitor, but it can only bind to active MMPs, which are subsequently removed irreversibly by endocytosis after connecting to a scavenger receptor. The C-terminal component of the procollagen C-terminal proteinase enhancer protein (PCPE) is another protein with MMP-inhibiting characteristics, but less effective than the TIMPs. The non-collagenous NC1 region of type IV collagen contains structural similarities with TIMPs and has been shown to inhibit MMP. Tissue factor pathway inhibitor-2, a serine protease inhibitor, and endostatin, a collagen XVIII-derived proteolytic fragment, may inhibit the activation of MMP-2, MMP-9, and MMP-13, as well as the catalytic activity of MMP-2 and MT1- MMP. Thrombospodin-1 (TSP-1) is an extracellular glycoprotein of 450 kDa that inhibits the activation of proMMP-2 and -9. Similar to 2-macroglobulin, it is believed that Thrombospondin-2 (TSP-2) binds MMP-2 and MMP-9 and facilitates low density lipoprotein receptorrelated protein (LRP)-mediated endocytosis and clearance. Reversioninducing cysteine-rich protein with Kazal motifs (RECK) protein is a glycoprotein with a molecular weight of 110 kDa that is widely expressed in normal tissues and is the only known membrane-bound MMP inhibitor. Finally, it has been shown that fatty acids decrease gelatinase activity but no other MMPs. The activity was dependent on the length of the carbon chain and the presence of unsaturation, and inhibition included binding to the fibronectin type II module. Other outstanding reviews examine endogenous MMP inhibitors in further depth.
| Inhibitor | Method of inhibition | Targets | |
|---|---|---|---|
| TIMP-1 | Catalytic activity | Most MMPs, ADAM-10, ADAMTS-4 | |
| TIMP-2 | Catalytic activity | Most MMPs, ADAMTS-4 | |
| TIMP-3 | Catalytic activity | Most MMPs, ADAM-10, -12, -17, ADAMTS-4, -5 | |
| TIMP-4 | Catalytic activity | Most MMPs | |
| α2-macroglobulin | Catalytic activity, clearance | Most proteases | |
| C-terminal of PCPE | Catalytic activity | ||
| Tissue factor pathway inhibitor-2 | Catalytic activity, activation | Serine proteases, other MMPs | |
| NC1 domain of type IV collagen | Catalytic activity | ||
| Endostatin | Catalytic activity, activation | MT1-MMP | |
| TSP-1 | Inhibition of activation | ||
| TSP-2 | Facilitates clearance | ||
| RECK proteins | Catalytic activity | MT1-MMP |
Table 1: Endogenous inhibitors of MMP-9.
Conclusion
The activation of Jak–STAT signalling requires no production of new molecules and involves just two sets of proteins, Jaks and STATs. Ligation of the cytokine receptor at the cell surface induces transcriptional responses in the nucleus. Despite its apparent simplicity, such a route is modulated by various elements at different levels of signal transduction. Several cellular mechanisms, including positive regulation, negative regulation, and reprogramming of STAT activity, coordinate the final consequence of cytokine stimulation. Using mouse genetics, the physiological roles of STATs have been deciphered. The role of STATs in the pathophysiology of rheumatic illness is an emerging topic of study, as detailed elsewhere. Understanding the pathogenic functions of STATs will undoubtedly aid in the creation of innovative treatment techniques. For instance, the carcinogenic characteristic of STAT3 might be a potential target for innovative cancer therapies. At the same time, enhancing STAT3's anti-inflammatory effect in myeloid cells might be advantageous for the treatment of inflammatory illnesses. Due to the pleiotropic nature of STAT1, it is unknown whether the enhanced expression of STAT1 during synovitis in rheumatoid arthritis is harmful or protective. Indeed, in one animal model of rheumatoid arthritis, STAT1 is protective. Consequently, STATs may have varying impacts on the aetiology of arthritis, depending on cell type and perhaps disease stage.
References
- Shin SY, Katz P, Wallhagen M, Julian L (2012) Cognitive impairment in persons with rheumatoid arthritis. Arthritis care & research 64:1144-1150.
- Vergne Salle P, Pouplin S, Trouvin AP, Bera‐Louville A, Soubrier M, et al. (2020) The burden of pain in rheumatoid arthritis: Impact of disease activity and psychological factors. European Journal of Pain 24:1979-1989.
- Covaci A, Tutudaki M, Tsatsakis AM, Schepens P (2002) Hair analysis: another approach for the assessment of human exposure to selected persistent organochlorine pollutants. Chemosphere 46: 413–418.
- Coxall M (2014) Ethical Eating: A Complete Guide to Sustainable Food Kindle Edition. Cornelio Books.
- Dennis LK, Lynch CF, Sandler DP, Alavanja MC (2010) Pesticide use and cutaneous melanoma in pesticide applicators in the agricultural heath study. Environ Health Perspect 118: 812– 817.
- Beard JD, Umbach DM, Hoppin JA (2014) Pesticide exposure and depressionamong male private pesticide applicators in the agricultural health study. EHP 122: 984–991.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Shivashankar (2023) Brief Review Notes on Neuroinflammation andArthritis Crosstalk: Theoretical Developments. Int J Res Dev Pharm L Sci, 9: 148.
Copyright: © 2023 Shivashankar. This is an open-access article distributed underthe terms of the Creative Commons Attribution License, which permits unrestricteduse, distribution, and reproduction in any medium, provided the original author andsource are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 1786
- [From(publication date): 0-2023 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 1405
- PDF downloads: 381