Calvarial Deformities in Children: A Radiological Gamut, Studied at a Tertiary Hospital
Received: 15-Nov-2017 / Accepted Date: 14-Dec-2017 / Published Date: 26-Dec-2017 DOI: 10.4172/2161-1165.1000335
Abstract
Aims and Objectives: To present the application of a protocol of low dose optimized for multidetector TC of 64 slice developed in our institution and directed to the study of the cranial deformity in the pediatric population.
• Compare the radiation doses obtained with this protocol with the standard reference levels recommended by ICRP (International council for Radiation Protection).
• To evaluate the diagnostic quality of the images obtained with this protocol.
Materials and Methods: We present this prospective study conducted in our institution between August 2015 and September 2017. A total of 87 studies were conducted in 81 patients (61 boys and 20 girls) with an age range of between 4 days and 6.5 years (median of 7 months). A single study was performed in 76 patients, two studies in 4 patients and three studies in 1 patient.
All studies were carried out with a 64 slice MDCT (Multidetector CT) scanner with bone reconstruction (Philips Brilliance USA), equipped with an automatic dose modulation system on the Z axis (AutomA) and subsequent images in MIP (maximum intensity projection), MPR (Multiplanar Reconstruction) and 3D mode.
Results: Of the total of 87 studies, 69 were initial CT for diagnosis, while 18 were follow-up studies. Of these 18 controls, 12 patients had one or more previous CT studies performed with our standard protocol. The studies were required, in descending order, by neurosurgeons, pediatricians and rehabilitators.
The most frequent reason for the request was the study of cranial deformities, especially to differentiate between significant postural plagiocephaly and craniosynostosis; less frequently, they were requested for postsurgical control or for the evolutionary follow-up of fractures.
Conclusion: This low dose protocol optimized for TCMD-64 and aimed at the study of cranial lesions, obtains images with good diagnostic quality using very low radiation doses. It may even obviate the need for simple radiography in clinically selected patients.
Keywords: Pediatric; Imaging; Reconstruction; Calvarium; Deformity
Introduction
According to the ALARA principle (As Low As Reasonably Achievable (as low as reasonably possible), it is necessary to develop low dose protocols for Computed Tomography (CT), especially if they are directed to the study of the pediatric population, given the greater sensitivity of this to ionizing radiation.
The most common clinical manifestation in such calvarial deformities is the cranial deformity, of variable degree, according to which sutures are altered. Sometimes it is accompanied by facial deformities. The skull stops growing in the synostosed area and compensatory grows more in the areas where the sutures are not yet ossified, in order to accommodate the growth of the underlying brain.
Anatomy and embryology
• The normal infant skull is oval and wider later.
• The cranial bones of the newborn are separated from each other by means of sutures and fontanelles composed of fibrocartilaginous tissue, which allow the expansion of the cranial vault and the progressive increase of the brain mass.
Greater sutures: Metopic, Sagittal, Lambdoid and Coronal.
Fontanelles: They are the space created between the confluence of more than one suture. They differ: two odd and half (anterior and posterior) and two lateral and even (mastoid and sphenoid) with the passage of time, when brain growth decreases, the sutures and fontanelles close. Usually the metopic suture closes between 9 months and 2 years, the coronal, sagittal and lambdoid sutures close at 40 years.
We present this paper highlighting the application of a protocol of low dose optimized for multidetector CT scanner developed in our institution and directed to the study of the cranial deformity in the pediatric population.
Materials and Methods
We present this prospective study conducted in our institution between August 2015 and September 2017. After obtaining clearance by the ethical committee attached to the Sardar Patel Medical College, Bikaner, Rajasthan, India.
Inclusion criteria
• Children with deformity or other cranial lesions to whom a CT scan was requested as a diagnostic imaging test or for evolutionary control.
• Children undergoing skull surgery who were asked for a postsurgical CT scan.
• Children with cranial fractures that present risk of transformation in evolutionary fractures to which a follow-up CT was requested.
A total of 87 studies were conducted in 81 patients (61 boys and 20 girls) with an age range of between 4 days and 6.5 years (median of 7 months). A single study was performed in 76 patients, two studies in 4 patients and three studies in 1 patient.
All studies were carried out with a 64 slice MDCT(multidetector CT) scanner with bone reconstruction (Philips Brilliance USA), equipped with an automatic dose modulation system on the Z axis (AutomA) and subsequent images in MIP (maximum intensity projection),MPR (multiplanar reconstruction) and 3D mode.
The low dose protocol used included, among others, the following parameters: voltage: 80 kVp; current intensity: between 50-150; noise index: 23.22 [1]. After the acquisition of a lateral topogram, an ocular bismuth protector was placed and a single helical acquisition without intravenous contrast was obtained.
In order to carry out the studies, the image quality criteria for encephalocerebellar CT in pediatrics recommended in the ICRP guidelines 2004 [2] were followed. These define, on the one hand, criteria of visualization (organs and structures that should be included in the volume of the study) and, on the other, criteria of critical reproduction (anatomical details that must be clearly defined). We have added a third criterion of critical reproduction of the three-dimensional (3D) reconstruction of the skull. According to these criteria, the diagnostic quality of the images was evaluated using a 3-point graduated scale:
• Good for diagnosis.
• Enough for the diagnosis.
• Insufficient for diagnosis.
All studies were reviewed and processed by two pediatric radiologists at a workstation (General Electric Advantage Workstation Volume Share 2 version 4.4 software).
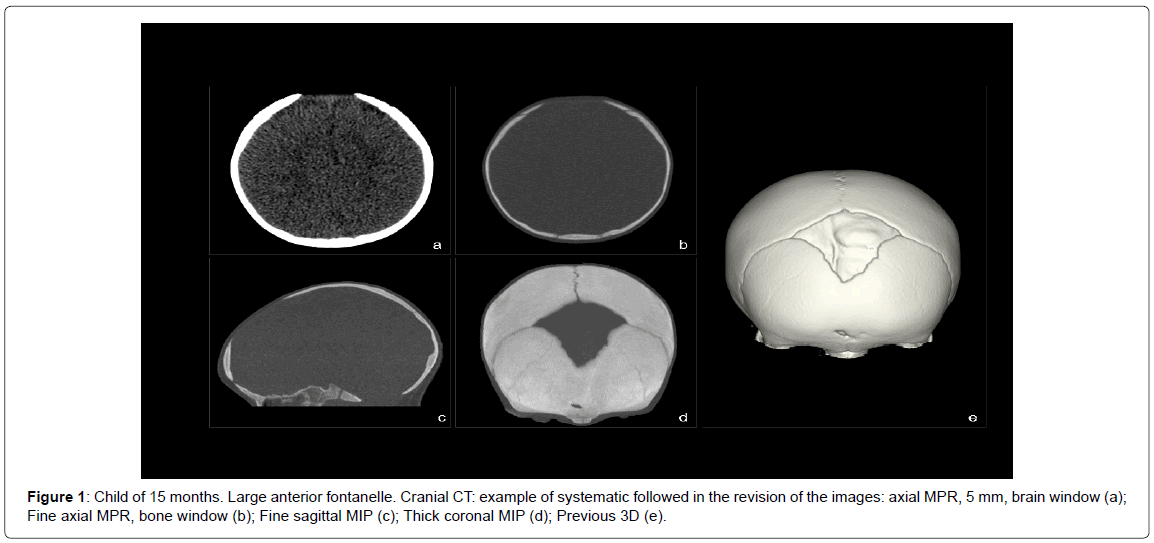
The systematics followed in the review of the studies consisted in Figure 1:
• Evaluation of the intracranial structures by reconstructed images with a soft tissue algorithm, 5 mm thick, in the brain window and, at least, in the axial plane.
Evaluation of skull bones and sutures by:
• Images reconstructed with bone algorithm, 1 to 2 mm thick, in bone window and, at least, in the axial plane.
• Images reconstructed with bone algorithm and in maximum intensity projection mode (MIP for its acronym in English), with fine thickness (2 to 3 mm) and thickness (5 to 50 mm).
• Three-dimensional volumetric reconstruction (3D) obtained from images with soft tissue algorithm.
As dose indicators we have used:
• CT Dose Index (CTDI vol): provided by the TC’s own console.
• Product Dose Length (DLP): provided by the TC’s own console.
• Effective dose (E): product of DLP by a conversion factor (k) dependent on body region and age (<1 year, k=0.011, 1-5 years, k=0.0067, 5-10 years, k=0.004 and>10 years, k=0.0032) [3].
For the statistical analysis of the data, the patients were divided into 3 groups, according to the age range defined by the conversion factor used in the calculation of E (<1 year, 1-5 years and 5-10 years).
Quantitative variables are presented with mean and standard deviation, and qualitative variables with frequencies and percentages.
Normality in the continuous variables (CTDIvol, DLP and E) was evaluated with the Kolmogorov-Smirnov test. For the comparison of means between the different age groups, the Kruskall-Wallis H test was used. All analyzes were performed with SPSS 15.0 for Windows (SPSS Inc., Chicago, IL). P<0.05 was considered statistically significant.
Result and Discussion
Of the total of 87 studies, 69 were initial CT for diagnosis, while 18 were follow-up studies. Of these 18 controls, 12 patients had one or more previous CT studies performed with our standard protocol [4].
The studies were required, in descending order, by neurosurgeons, pediatricians and rehabilitators.
The most frequent reason for the request was the study of cranial deformities, especially to differentiate between significant postural plagiocephaly and craniosynostosis; less frequently, they were requested for postsurgical control or for the evolutionary follow-up of fractures with the risk of becoming increasing fractures and craniosynostosis or other cranial defects that did not require surgical correction.
All the studies were well tolerated, without complications in any patient.
The image quality was considered good for the diagnosis in a concordant manner in 85 of the 87 studies (98%). Only two studies were considered inadequate for the diagnosis and it was necessary to repeat them. This was due to patient movements during the acquisition and not to technical deficiencies of the protocol.
The findings in the initial diagnostic studies included:
• Craniosynostosis (9 cases, 13%):
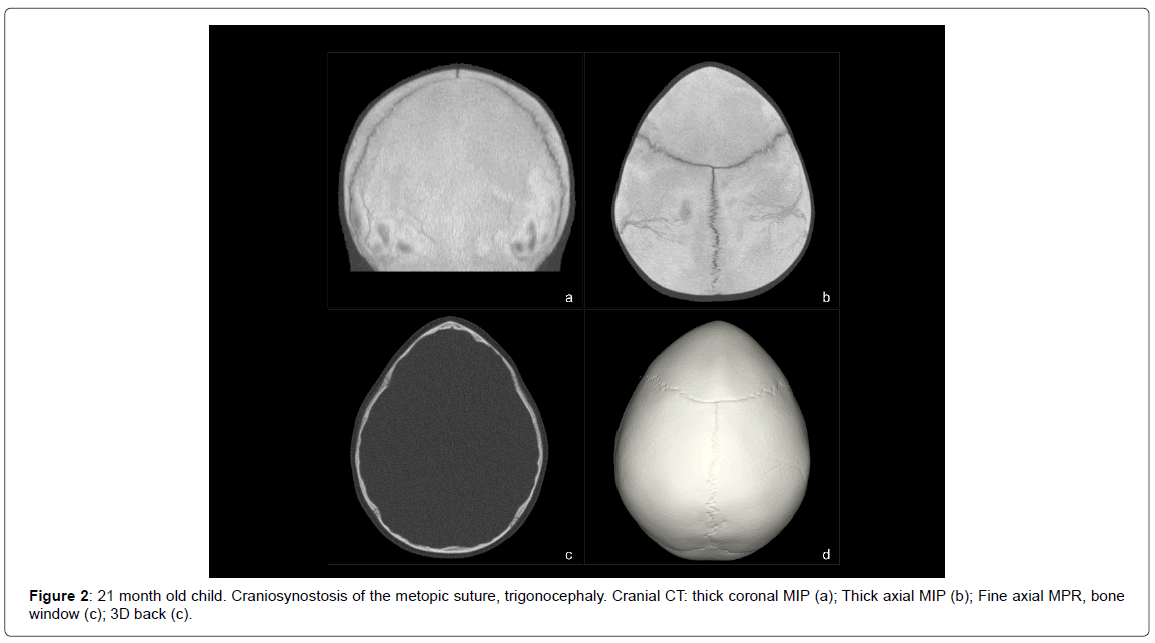
- Synostosis of the metopic suture (3 cases) (Figure 2).
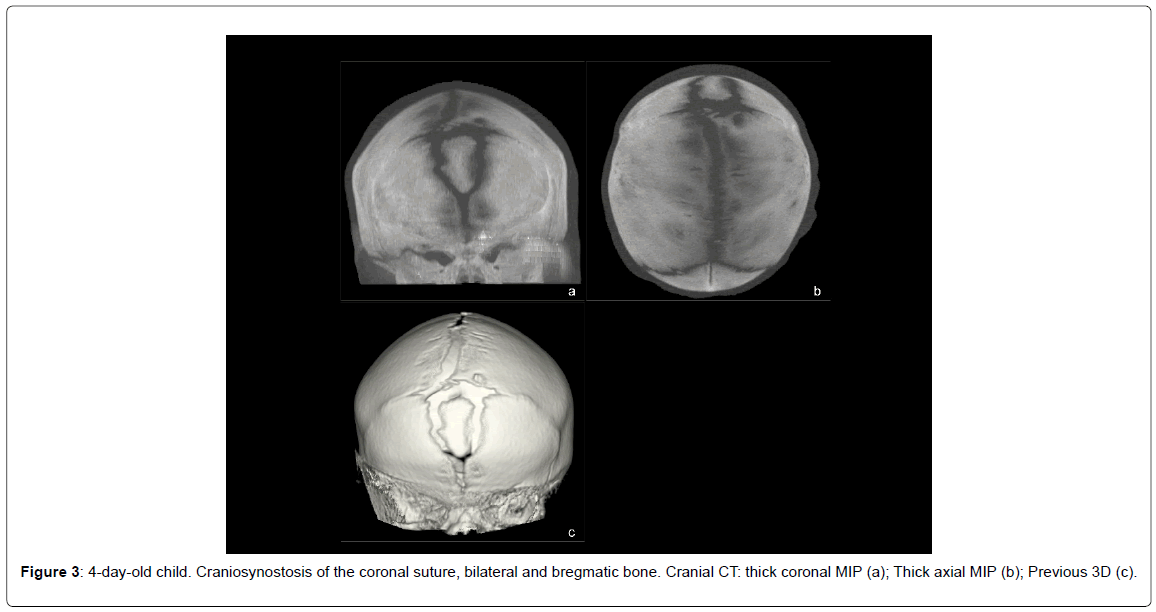
- Bilateral synostosis of the coronal suture (1 case) (Figure 3).
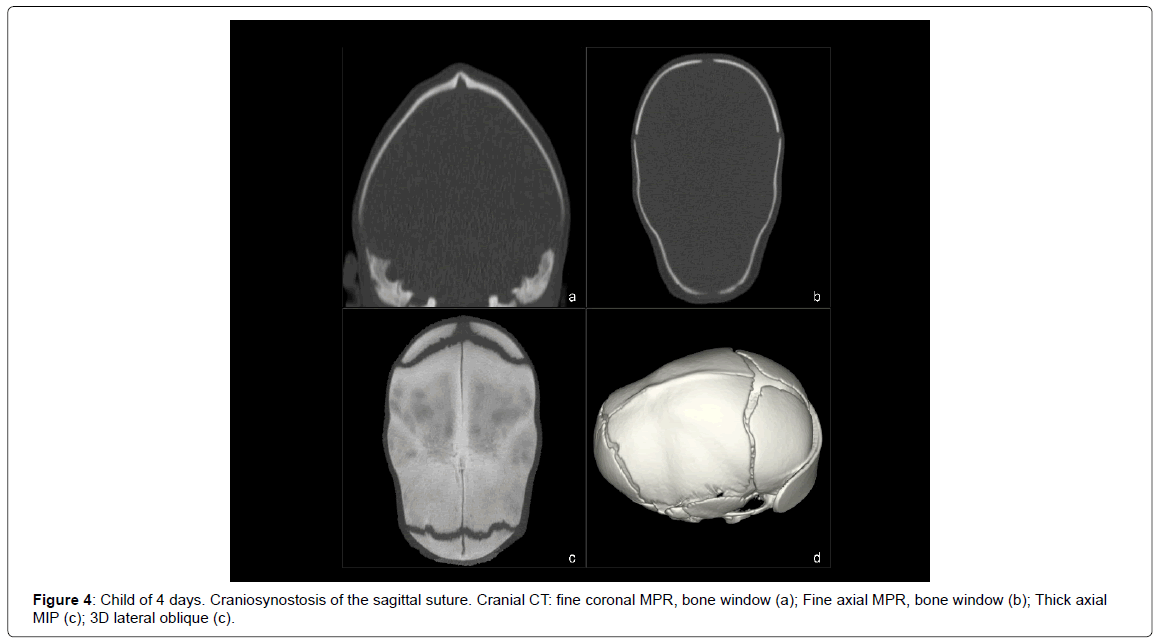
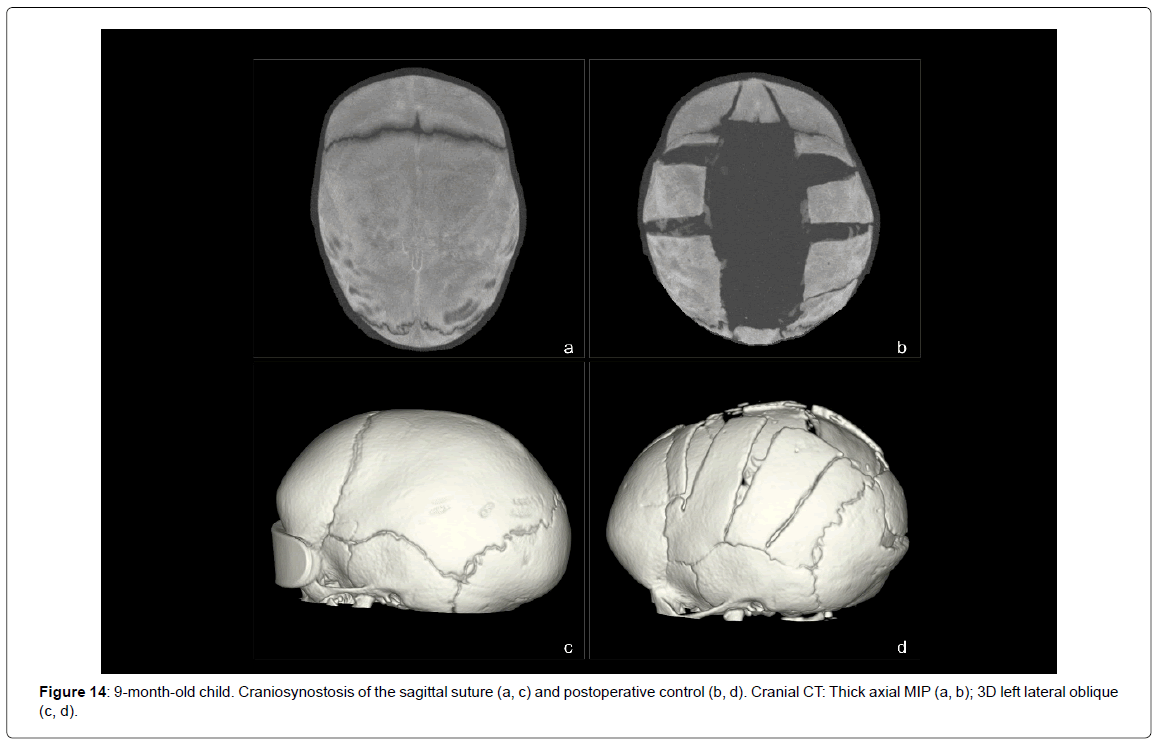
- Synostosis of the sagittal suture (4 cases) (Figure 4).
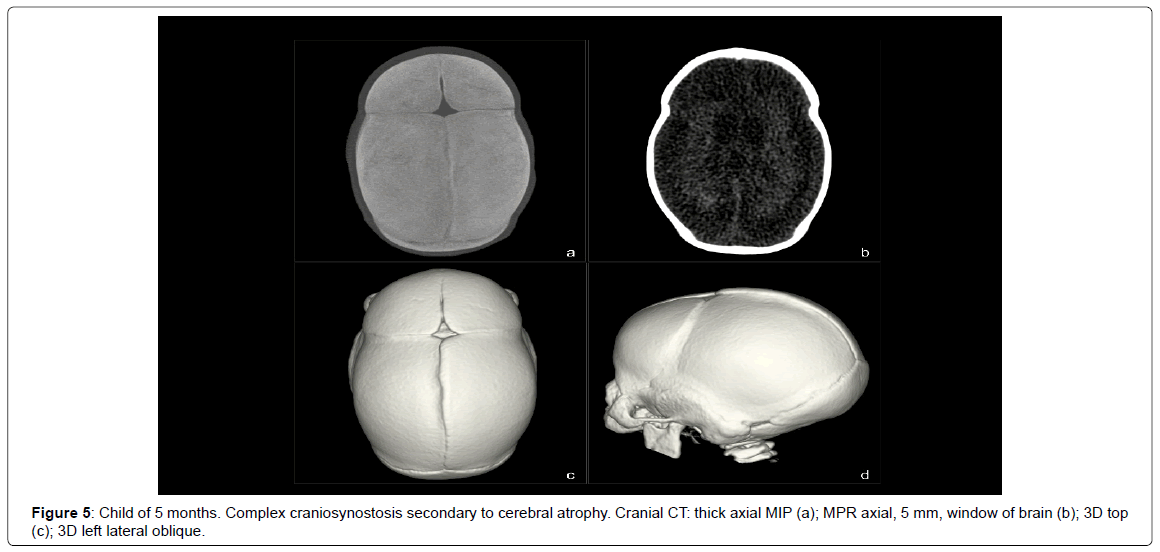
- Complex craniosynostosis secondary to cerebral atrophy (1 case) (Figure 5).
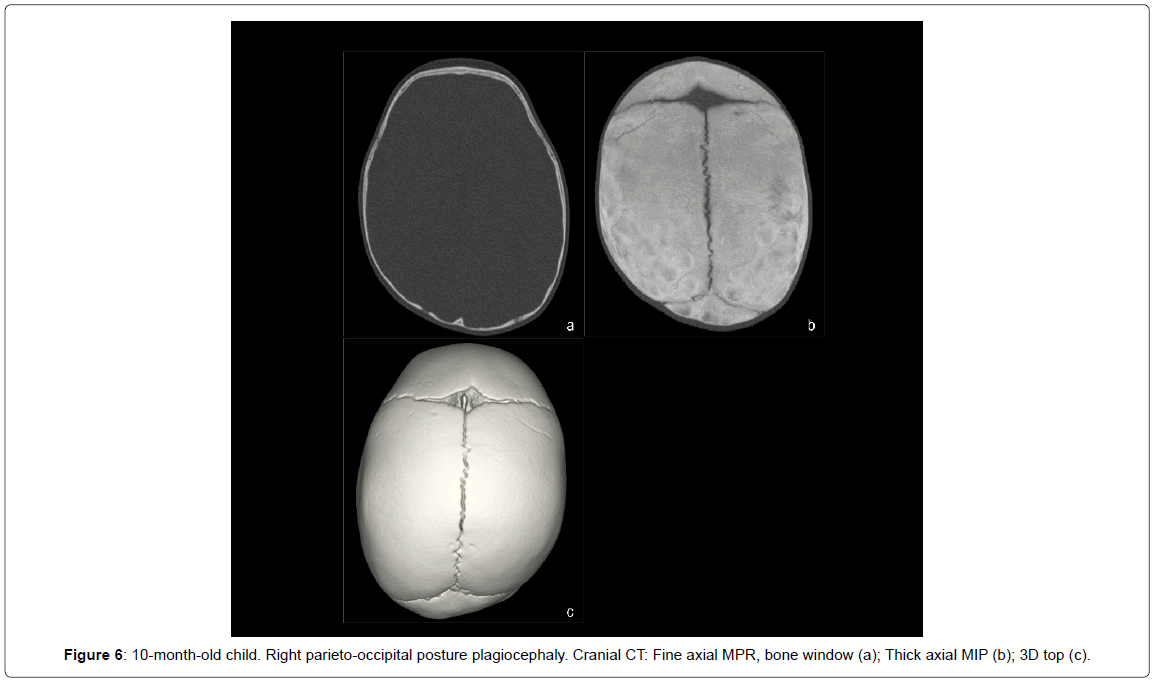
• Postural plagiocephaly (38 cases, 55.1%) (Figure 6).
• Dolichocephaly not associated with craniosynostosis (1 case, 1.45%).
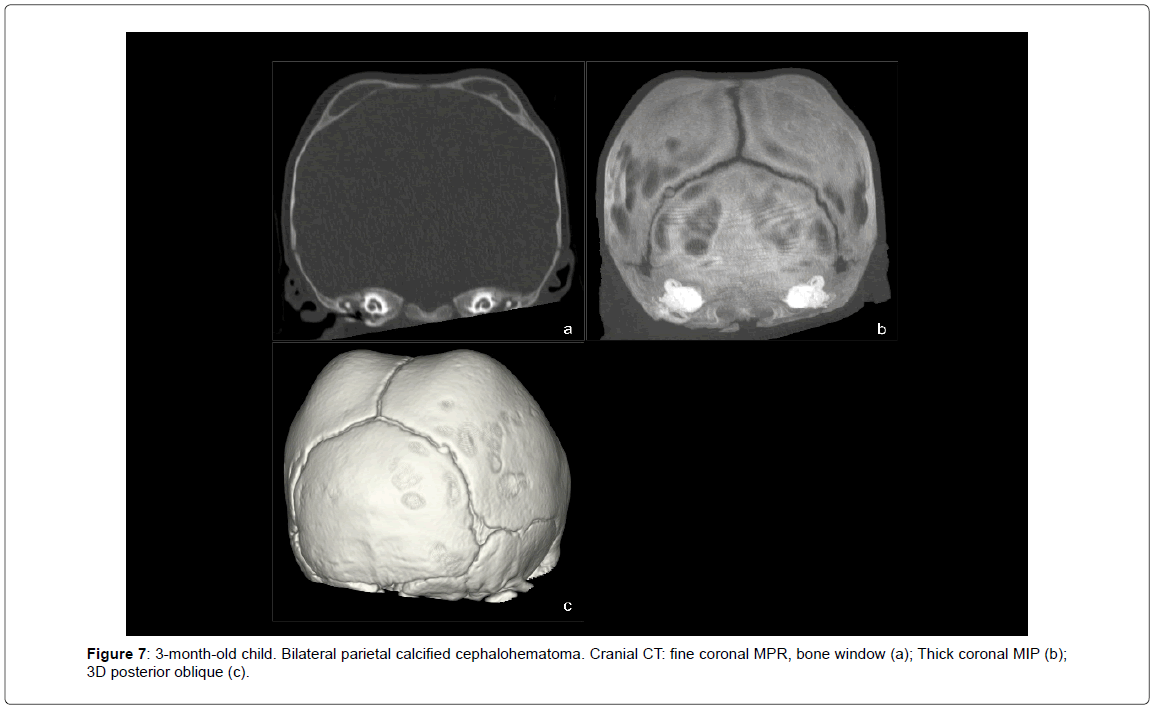
• Céphalohematoma (4 cases, 5.8%) (Figure 7).
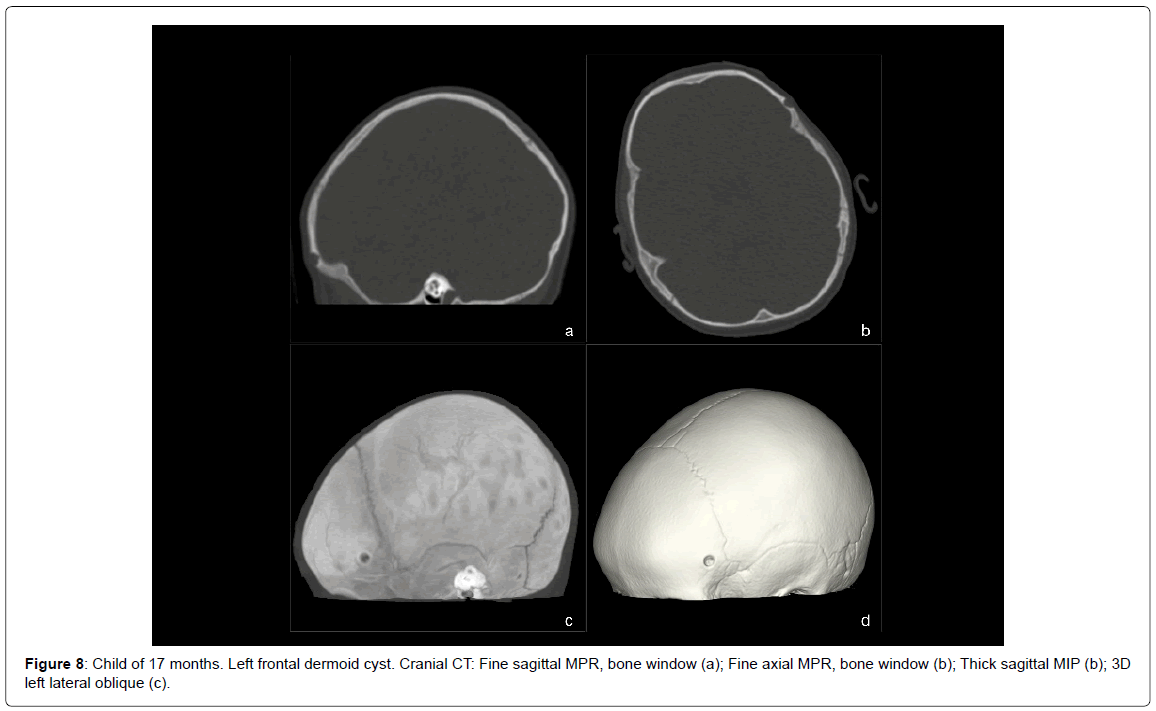
• Dermoid cysts (1 case, 1.45%) (Figure 8).
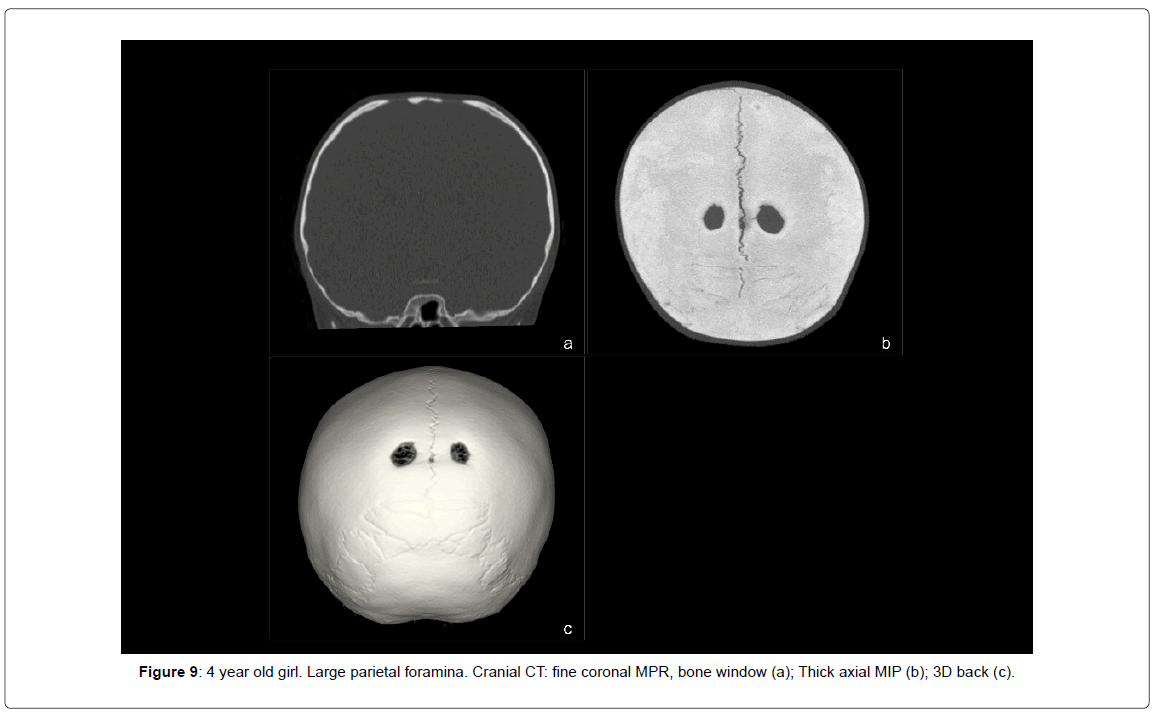
• Large parietal foramina (1 case, 1.45%) (Figure 9).
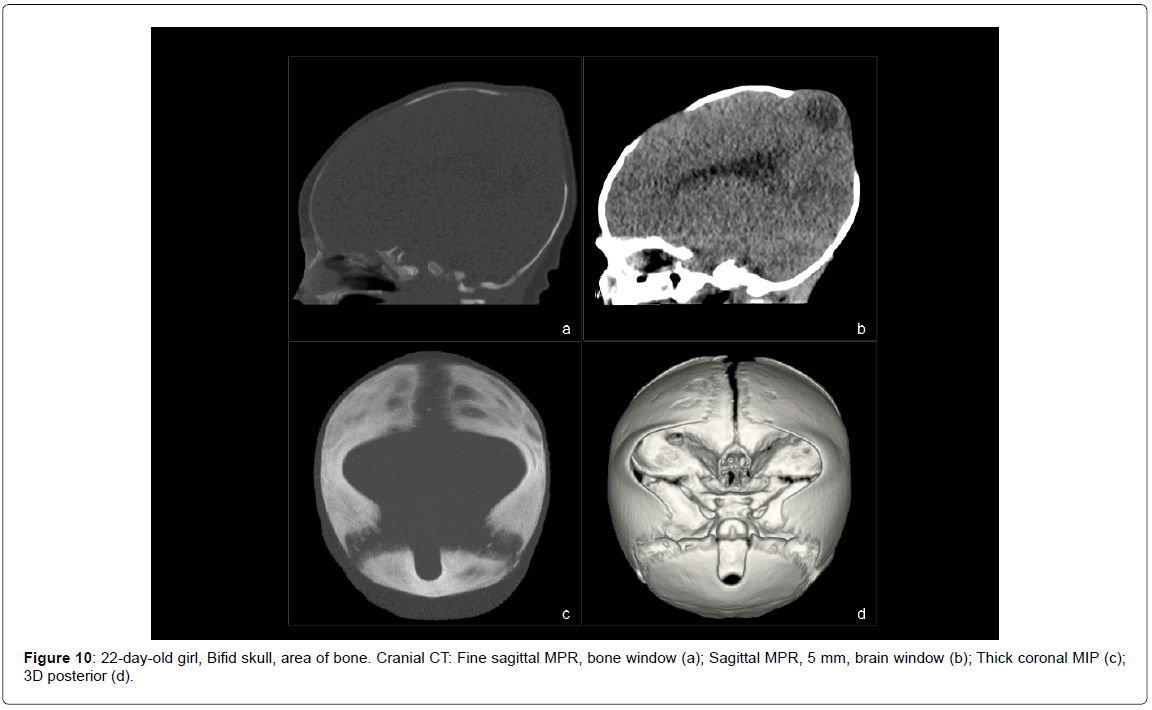
• Bifid skull (1 case, 1.45%) (Figure 10).
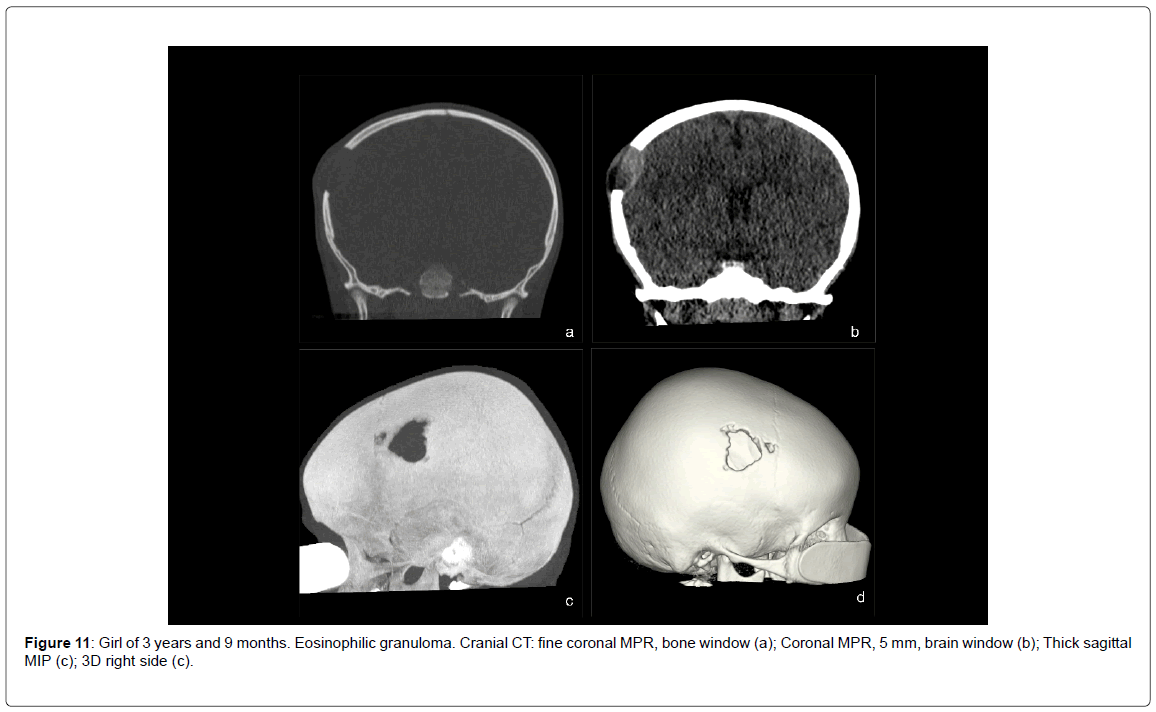
• Eosinophilic granuloma (1 case, 1.45%) (Figure 11).
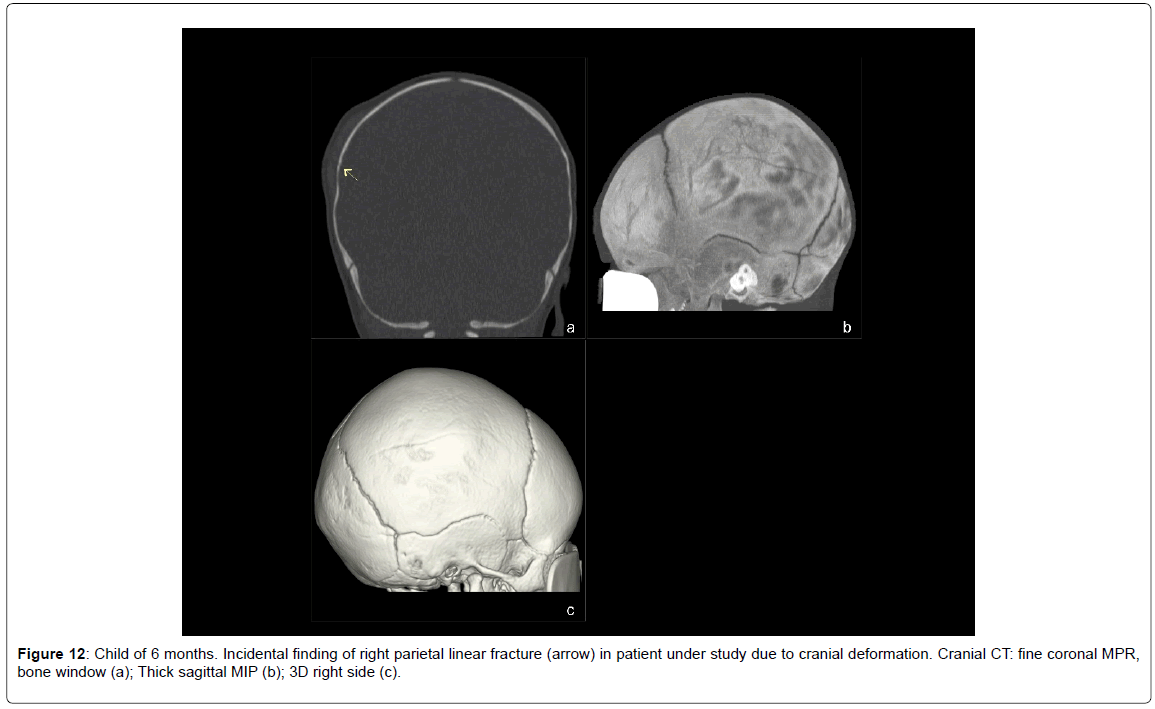
• Incidental finding of a linear fracture (1 case, 1.45%) (Figure 12).
• Normal studies (12 cases, 17.4%).
Of patients with craniosynostosis, 3 are syndromic patients: 1 with Crouzon syndrome, 1 with Muenke syndrome and 1 with an as yet unidentified syndrome pending genetic study. The patient with dolichocephaly not associated with craniosynostosis is also syndromic, with a syndrome associated with 5q14-q15 deletion.
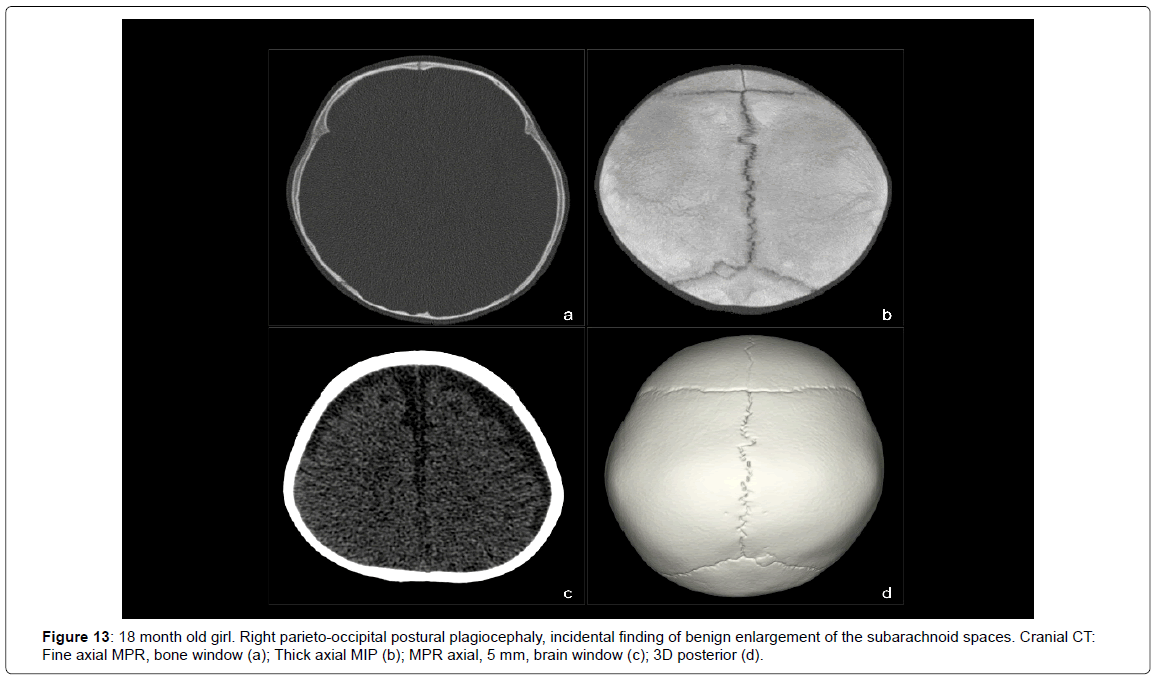
This low dose protocol is aimed at the study of the skull and does not allow an accurate evaluation of the intracranial structures. Even so, it was possible to incidentally detect some gross anomalies, such as a benign enlargement of the subarachnoid spaces (Figure 13), a severe brain atrophy in a patient with secondary global craniosynostosis and even an area of encephalomalacia in a patient with bifid skull.
Among the control examinations, 1 was for follow-up of craniosynostosis, 3 for fractures with the risk of developing into evolutive fractures, 1 for a large anterior fontanelle and 13 for postoperative control: surgically corrected craniosynostoses (11 studies) (Figure 14) and granuloma excision eosinophils (1 study) or dermoid cysts (1 study).
The average values obtained according to age groups were:
• For children
• For children between 1-5 years: CTDIvol, 2.15 mGy; DLP, 39.07 mGy/cm; E, 0.26 mSv.
• While the minimum dose values:
• For children
• For children between 1-5 years old: CTDIvol, 1.68 mGy; DLP, 29.11 mGy/cm; E, 0.20 mSv.
• On the other hand, the reference dose values for encephalocerebral CT studies in the pediatric population recommended in the European guidelines for MDCT 2004 are [5]:
• For children
• For children between 4 and 6 years old: CTDIvol, 47 mGy; DLP, 374 mGy/cm; E, 1.8 mSv.
This translates into an average dose reduction of up to 16 times and a maximum of up to 30 times compared to the levels recommended in the ICRP guidelines for the
As for the calculation of the additional risk of cancer, the estimated values are below the two decimal places, very close to 0.
Conclusion
This low dose protocol optimized for 64 slice CT scanner and aimed at the study of cranial lesions, obtains images with good diagnostic quality using very low radiation doses. It may even obviate the need for simple radiography in clinically selected patients.
This protocol can be adapted to other MDCT equipment, both from the same brand with different number of detectors as from other manufacturers. In the first case, selecting the same Noise Index for an acquisition width of 1.25 mm for equipment from other manufacturers, by adapting the noise index to its specific parameters of automatic exposure control, In both cases keeping the rest of the technical parameters.
The application of new advances such as adaptive collimation, iterative reconstructions, axial volumetric acquisition of data, the possibility of using smaller kilovolts, better beam filters and software improvements will allow even greater dose savings 7.
Acknowledgements
NIL.
Financial Support
NIL.
Source of Funding
NIL.
References
- Vazquez JL, Pombar MA, Pumar JM, del Campo VM (2013) Optimised low-dose multidetector CT protocol for children with cranial deformity. Eur Radiol 23: 2279-2287.
- Valentin J (2007) Managing Patient Dose in Multi-Detector Computed Tomography (MDCT). Chapter and Appendix A. Ann IRCP 37: 59-79.
- Hanley M, Koonce JD, Bradshaw ML (2009) www.X-rayRisk.com: an online calculator for cancer risk. J Am Coll Radiol 6: 475-476.
- Alessio AM, Phillips GS (2010) A pediatric CT dose and risk estimator. Pediatr Radiol 40: 1816-1821.
Citation: Razak MK, Gupta S, Meena GL (2017) Calvarial Deformities in Children: A Radiological Gamut, Studied at a Tertiary Hospital. Epidemiol 8: 335. DOI: 10.4172/2161-1165.1000335
Copyright: ©2017 Razak MK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6445
- [From(publication date): 0-2018 - Dec 11, 2025]
- Breakdown by view type
- HTML page views: 5504
- PDF downloads: 941