Cartilage Palisade Grafting in Retrograde Canal Wall Down Mastoidectomy: A Review of 80 Cases
Received: 07-Mar-2017 / Accepted Date: 30-Mar-2017 / Published Date: 06-Apr-2017 DOI: 10.4172/2161-119X.1000302
Abstract
Objective: Although synthetic grafts have been extensively used for tympanoplasty in canal wall down mastoidectomy, a substantial proportion of the patients show graft extrusion. Conchal cartilage grafts can be effectively used for the above purpose for a better graft uptake and hearing gain. Here, anatomical and functional outcomes have been assessed in 80 patients undergoing retrograde canal wall mastoidectomy with cartilage tympanoplasty. Material and methods: This study was conducted in a tertiary care referral hospital during the period from July 2012 to June 2015. A total 80 patients of active squamous disease with conductive hearing had undergone canal wall down mastoidectomy. Pure tone audiogram and speech reception thresholds were carried out in preoperative and each postoperative visit i.e. at 3, 6, 12 months of surgery. ≥ 10 dB closure of air-bone (AB) gap and ≥ 10 dB improvement in speech reception threshold were considered significant. Results: Out of 80 patients, 58 (72.50%) were males and 22 (27.50%) were females and 68 (85.00%) were fresh cases and 12 (15.00%) were revision cases. Overall closure of the tympanic membrane was achieved in 76 (95.00%) cases. At the end of 12 months, mean air conduction threshold was 34.30 dB with 8.2 dB closures of AB gap was found in new cases and 35.08% of them had significant improvement in hearing. Again the mean air conduction thresholds for the revision cases was 40.8 dB with 6.9 dB closure of AB gaps noticed at the end of 12 months and 25% of the them had significant improvement in hearing (≥ 10 dB closure). Conclusion: Autologous conchal cartilage can be used for the tympanic membrane grafting in patients undergoing canal wall down mastoidectomy with minimal rejection rate. Although significant improvement in hearing was achieved in 33.80% cases, almost all had social serviceable hearing till the end of 12 months.
Keywords: Cartilage tympanoplasty; Canal wall down mastoidectomy
254937Introduction
Canal wall down mastoidectomy is a routinely surgical procedure performed in any otologic clinic for active squamosal chronic otitis media, aimed at safe and a dry mastoid cavity with improvement of the residual hearing. Although the initial two goals are achieved with little difficulty, improvement in hearing is a surgical challenge in patients undergoing canal wall down mastoidectomy. It is because, to maintain the original ossicular continuity is always difficult task, as the middle ear width is partially obliterated due to the removal of the posterior canal wall. Although it can be performed through outside in or inside out mastoidectomy procedure, later is more preferred in the present time due to the decreased postoperative morbidly. Since bone drilling is comparatively less in the inside out mastoidectomy, there produced a smaller cavity for leading to early epithelialization of the mastoid cavity decreasing the incidence of postoperative cavity problem. Again there is reduction in the middle ear air space resulting to detrimental in the acoustic transmission of the sound. Both autologous grafts (cartilage/bone) and synthetic grafts (titanium/hydroxyapatite) has been extensively used in the past in an effort to improve in hearing threshold in patients undergoing with canal wall down mastoidectomy. Although improvement in hearing is found to be satisfactory with synthetic ossicular grafts as demonstrated in many past literatures, a substantial proportion of the patients require revision surgery because of its displacement and extrusion [1,2]. Keeping in view the above facts, autologous cartilage grafts have been tried for ossiculoplasty [3] alternate to its synthetic counterparts for canal wall down mastoidectomy and is expected to have a good anatomical and functional outcome. In the present study, 80 patients of active squamosal chronic otitis media have undergone retrograde canal wall down mastoidectomy with classical type III cartilage palisade tympanoplasty. The anatomical and functional outcomes were assessed after 12 months of surgery.
Material and Methods
This study was conducted in a tertiary care referral hospital during the period from July 2012 to June 2015. A total 80 patients of active squamous chronic otitis media with conductive hearing loss were included in the study. HRCT of temporal bone was routinely performed for each of the patient preoperatively and patients having intact stepes suprastructure irrespective of the status of malleus and incus were included in the study. Pure tone audiogram (PTA) and speech reception threshold (SRT) was advised for each patient in preoperative and in each postoperative follow-up visit. All the patients underwent retrograde canal wall down mastoidectomy with classical type III tympanoplasty by putting a strip of full thickness conchal cartilage over the stepes head.
Operative Procedure
All canal wall down mastoidectomies were performed by a single surgeon, exclusively by post auricular approach under general anesthesia. Circumferential canal skin was elevated which was pedicled anteriorly at 3 to 6 ‘o’ clock position. Canaloplasty was performed with a large diamond burr followed by atticotomy where the outer attic wall was removed to expose the cholesteatoma sac. Further removal of posterior bony canal wall was done according to the extension of the cholesteatoma sac. Ossicular continuity was assessed, malleus and incus were removed. Complete clearance of the disease was ensured after lowering the facial ridge to the level of lateral semicircular canal and to the floor of the middle ear cavity. Special surgical procedures like facial nerve decompression was performed wherever required.
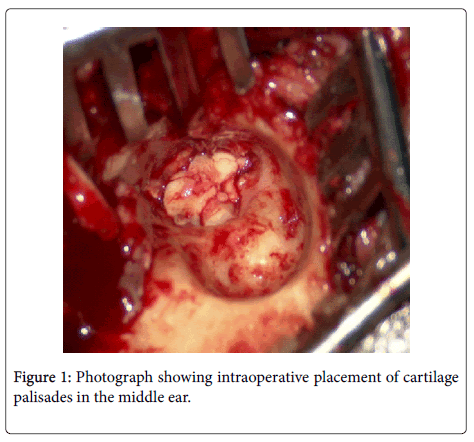
Wide meatoplasty was performed after removing a large piece of conchal cartilage which was cut in to 3 full thickness pieces, 2 semi lunar shaped and one small rectangular shaped to negotiate the shape of the middle ear cavity. First semilunar cartilage piece was placed posteriorly over covering the stepes head (type III tympanoplasty) and second was placed anteriorly by forwarding towards the eustachian tube area and the small rectangular piece was placed in between them as shown in Figure 1.
The cartilage assembly was supported laterally by temporalis fascia further secured laterally by gelfoams. Skin incision was closed in double layer and mastoid dressing was placed. Patents were discharged after 48 h of the operation after changing the mastoid dressing and were advised to visit the otology clinic after one week for removal of postaural stitch and mastoid pack. Subsequent visits were allowed at the end of 3 months, 6 months and 12 months and at each follow-up visit, otomicroscopic cleaning of the mastoid cavity and assessment of the hearing were carried out. Average air and bone conduction thresholds were calculated at the mean of 0.5, 1, 2 and 4 kHz frequencies. More than 10 dB closure of air-bone (AB) gap and 10 dB improvement in speech reception threshold were considered significant. Preoperative and postoperative data obtained were analyzed and compared by student’s t-test.
Results
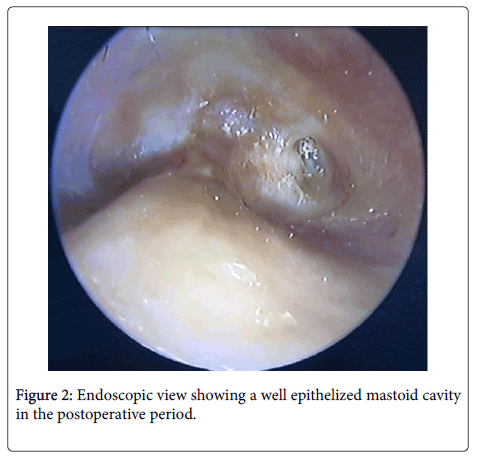
Out of 80 patients, 58 (72.50%) were males and 22 (27.50%) were females and 68 (85%) were new cases to the otology clinic and 12 (15%) cases had previous history of surgery. The mean of duration of the disease was12 months (8-19 months) for new cases and 10 months (range 6-13 months) for the revision cases (Table 1). Cholesteatoma was found in all primary cases and of the revision cases, majority 8 (66.66%) were presented with meatal stenosis and 4 (33.34%) of patients had high facial ridge. All the patients except the revision cases have undergone retrograde canal wall down mastoid exploration through postural approach. Classical type III cartilage tympanoplasty was performed in 71 cases (62 from new and 9 from revision). In 5 cases (4 from the new cases and 1 from the revision cases), tympanoplasty could not have done because of extensive granulation tissue in the middle ear. In 4 patients (2 from new group and 2 from revision group) stepes suprastructure was found to be missing and were posted for total ossicular replacement prosthesis. No major intraoperative and postoperative complications detected in the surgical study. In 5 (6.25%) patients (2 from new cases and 3 from revision cases) there was erosion of tegmen tympani leading to exposure of dura without any intraoperative or postoperative complication. Of the 80 ears undergoing type III cartilage tympanoplasty, anatomical closure of the tympanic membrane was achieved in 95.00% of the cases (Figure 2).
| Patient characteristics | New cases n=68 (85%) | Revision cases n=12 (15%) |
|---|---|---|
| Mean age | 29 years | 33 years |
| Male | 54 (79.41%) | 4 (33.33%) |
| Female | 14 (20.85%) | 8 (66.66%) |
| Mean duration of disease | 12 months | 10 months |
| range | 8-19 months | 6-13 months |
| Anatomical closure of TM | 83.34% | 97.00% |
| Preoperative air conduction threshold | 42.50 dB | 47.70 dB |
| Postoperative air conduction threshold | ||
| 3 months | 32.40 dB | 39.90 dB |
| 6 months | 33.80 dB | 40.2 dB |
| 12 months | 34.30 dB | 40.80 dB |
| Postoperative AB closure | ||
| 3 months | 10.10 dB | 7.80 dB |
| 6 months | 8.7 dB | 7.80 dB |
| 12 months | 8.20 dB | 6.90 dB |
| Speech Reception threshold(SRT) | ||
| Preoperative SRT | 41.4 dB | 46.6 dB |
| Postoperative SRT | 39.6 dB | 44.9 dB |
Table 1: Description of patients data in the in the perioperative period.
4 patients (2 from the new patient group and one 2 from the revision group) presented with displacement of a cartilage strip detected at the end of 12 months and patients were managed with cartilage tympanoplasty under local anesthesia after 12 months. There was no recurrence of disease till 12 months of follow-up, although 3 (2 from primary and 1 from revision) patients had persistent ear discharge because of meatal stenosis as a result of perichondritis in the immediate postoperative period. The mean period of healing the mastoid cavity including the new and the revision cases was 70 days. Mean preoperative air conduction thresholds were 42.50 dB and 47.70 dB for new cases and revision cases respectively with average 0.5, 1, 2 and 4 kHz frequencies. At the end of 3 months, the mean air conduction threshold of the new patients was 32.40 dB with 10.10 dB closure of the AB gap and for the revision cases it was 39.90 dB with 7.50 dB closure of AB gap. Similarly, at the end of 6 months and 12 months, the mean air conduction thresholds of new cases were 33.80 dB and 34.30 dB with 8.7 dB and 8.2 dB closure of AB gaps respectively. At the end of 6 months and 12 months, the mean air conduction thresholds of revision cases were 40.2 dB and 40.8 dB with 7.50 dB and 6.90 dB closure of AB gaps respectively. At the end of 3 months, 48% of the new patients and 39% of revision patients had significant improvement in hearing (≥ 10 dB AB closure). Similarly at the end of 6 months, 38 % of patients of new cases and 32% of revision cases presented with significant hearing improvement in hearing. Again at the end of 12 months, 35.08% of cases of new patients and 25% of revision patients had shown significant improvement in hearing. Mean preoperative speech reception threshold of the new and revision patients were 41.4 dB and 46.6 dB respectively and the respective postoperative scores were 39.6 dB and 44.9 dB respectively for the revision cases.
Discussion
Providing a dry mastoid cavity and improvement in the preexisting hearing are the two important goals aimed at canal wall down mastoidectomy. Although tympanic membrane grafting is an important determinant for a well epithelized mastoid cavity in the postoperative period, yet it has always been given the least importance particularly in canal wall mastoidectomy. Assuming eustachian tube dysfunction could be the important factor for pathogenesis of primary cholesteatoma, full thickness cartilage palisade could be a better option for tympanic membrane grafting, as later prevents recurrent retraction of the tympanic membrane and hence the disease recurrence. Again due to the concavity of the conchal cartilage, it can readily fit to the middle ear cavity to provide a good cartilage assembly and expected to improve both the anatomical and functional outcome of the ossiculoplasty.
In the present study, 80 cases of active squamosal chronic otitis media have undergone canal wall down mastoidectomy with classical type III tympanoplasty using full thickness conchal cartilage palisades and have shown excellent anatomical results, i.e., 76 (95.00%) patients had complete closure of the tympanic membrane. 2 patient from the fresh group and 2 patients from the revision group had residual perforation at the end of 12 months (P=0.06). These anatomic results probably resulted from the fact that the cartilage grafts are being nourished by diffusion and imbibition and can be viable in relatively avascular environment resulting in excellent incorporation into the remaining tympanic membrane [4].
Considering the hearing outcome at the first follow-up period i.e. at the end of 3 months, it has been noted that 48% of new cases and 39% of revision cases had significant improvement in hearing (≥ 10 dB AB closure) and the difference was found significant (p=0.00). Again the improvement in hearing (mean AB closure) is slightly decreased in the subsequent follow-ups for both new and the revision patients (p=0.797), observed at the end of 12 months. In the present study all the patients had improvement in hearing at the third follow-up and 35.08% of the fresh patients and 25% of the revision patients had significant improvement in hearing (p=0.006). Although better hearing outcomes have been documented in type III tympanoplasty using synthetic ossicular grafts as demonstrated in various past literatures, a substantial proportion of the patients require revision surgery because of displacement and extrusion of graft in the postoperative period [5-7]. There are very few studies conducted in the past showing cartilage being exclusively used for ossiculoplasty and tympanic membrane grafting (classical type III tympanoplasty) in canal wall down mastoidectomy [8] although it has been widely used for type I cartilage tympanoplasty for the reconstruction of a large central perforation and for the repair of attic defect in limited attic disease [9-12]. A similar study conducted by Quaranta et al. [13] taking patients undergoing cartilage tympanoplasty in intact canal wall mastoidectomy has demonstrated 100% anatomical closure of tympanic membrane without any extrusion of cartilage graft in the postoperative period. As described by Sendra J et.al.in a parallel study taking patients, those have undergone cartilage tympanoplasty in intact canal wall mastoidectomy have noted <30 dB closure of AB gap in 92.2% of the cases with 9.72 dB mean improvement of hearing [14]. Unlike the improvement in hearing threshold, there was no significant difference in the SRT between two groups (p=0.296) as described by Bernal- Sprekelsen et al. [6]. It has been noted that autologous cartilage tympanoplasty in retrograde canal wall down mastoidectomy is a safe and effective procedure with encouraging postoperative results. Presence of stepes suprastructure is an important determinant for hearing outcome as it is evident in the current study and which has been supported different authors [15-17]. Conchal cartilage can be abundantly obtained in canal wall down mastoidectomy without much difficulty and can be used in the same operative sitting. Unlike synthetic grafts, cartilage grafting does not fix to promontory or facial nerve, would have been associated with worsening of hearing [18]. Almost all of the patients had a dry mastoid cavity at the end of three months and that could be due successful graft uptake by cartilage palisade. In our experience the cartilage tympanoplasty is little lengthy in comparison to the conventional myringostapedopexy because it needs nearly 15 min extra time to shape and positioning of the conchal cartilage and can be considered a better option for patients, refusing for regular follow-up in a developing country like India.
Conclusion
Autologous conchal cartilage can be used for the tympanic membrane grafting in patients undergoing canal wall down mastoidectomy with minimal rejection rate. Cartilage being inexpensive and abundantly available from the same surgical site can be safely placed in the middle ear in the same sitting to have a satisfactory outcome. Although significant improvement in hearing was achieved in 33.80% cases, almost all had social serviceable hearing till the end of 12 months.
References
- Pringle MB, Sunkaraneni VS, Tann N (2014) Is cartilage interposition required for ossiculoplasty with titanium prostheses? Otol Neurotol 35: 482-488.
- Yung M, Smith P (2010) Titanium versus nontitanium ossicular prostheses-a randomized controlled study of the mediumterm outcome. Otol Neurotol 31: 752–758
- Yung M (2008) Cartilage tympanoplasty: Literature review. J Laryngol Otol 122: 663-672.
- Schuknecht HF, Shi SR (1985) Surgical pathology of middle ear implants. Laryngoscope 95: 249-258.
- Gerber MJ, Mason JC, Lambert PR (2000) Hearing results after primary cartilage tympanoplasty. Laryngoscope 110: 1994-1999.
- Bernal-Sprekelsen M, Romaguera Lliso MD, Sanz Gonzalo JJ (2003) Cartilage palisades in type III tympanoplasty: Anatomic and functional long-term results. Otol Neurotol 24: 38-42.
- Rondini-Gilli E, Grayeli AB, Borges Crosara PF, El Garem H, Mosnier I, et al. (2003) Ossiculoplasty with total hydroxylapatite prostheses anatomical and functional outcomes.Otol Neurotol 24: 543-547.
- Kalcioglu MT, Tan M, Croo A (2013) Comparison between cartilage and fascia grafts in type 1 tympanoplasty. B-ENT 9: 235-239.
- Vashishth A, Mathur NN, Choudhary SR, Bhardwaj A (2014) Clinical advantages of cartilage palisades over temporalis fascia in type I tympanoplasty. Auris Nasus Larynx 41: 422-427.
- Güneri EA, Ikiz AO, Erdag TK, Sütay S (2009) Cartilage tympanoplasty: Indications, techniques and results. J Otolaryngol Head Neck Surg 38: 362-368.
- Ozbek C, Ciftçi O, Tuna EE, Yazkan O, Ozdem C (2008) A comparison of cartilage palisades and fascia in type 1 tympanoplasty in children: Anatomic and functional results. Otol Neurotol 29: 679-683.
- Wielgosz R, Mroczkowski E (2006) Assessment of the hearing results in tympanoplasties with the use of palisade-technique. Otolaryngol Pol 60: 901-905.
- Quaranta N, Fernandez-Vega Feijoo S, Piazza F, Zini C (2001) Closed tympanoplasty in cholesteatoma surgery: Long-term (10 years) hearing results using cartilage ossiculoplasty. Eur Arch Otorhinolaryngol 258: 20–24.
- Sendra J, Rosell A, Navas C, Denia AJ, Denia A (2001) Long-term functional results in ossicular reconstruction with cartilage. Acta Otorrinolaringol Esp 52: 103-109.
- Mishiro Y, Sakagami M, Adachi O, Kakutani C (2009) Prognostic factors for short-term outcomes after ossiculoplasty using multivariate analysis with logistic regression. Arch Otolaryngol Head Neck Surg 135: 738–741.
- Mills RP (1993) The influence of pathological and technical variables on hearing results in ossiculoplasty. Clin Otolaryngol Allied Sci 18: 202-205.
- Wilson KF, London NR, Shelton C (2013) Tympanoplasty with intact canal wall mastoidectomy for cholesteatoma: Long-term hearing outcomes. Laryngoscope 123: 3168-3171.
- Farrior JB, Nichols SW (1996) Long-term results using ossicular grafts. Am J Otol 17: 386-392.
Citation: Pradhan P, Lal P (2017) Cartilage Palisade Grafting in Retrograde Canal Wall Down Mastoidectomy: A Review of 80 Cases. Otolaryngol (Sunnyvale) 7:302. DOI: 10.4172/2161-119X.1000302
Copyright: © 2017 Pradhan P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distributionand reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3717
- [From(publication date): 0-2017 - Jul 06, 2025]
- Breakdown by view type
- HTML page views: 2858
- PDF downloads: 859