Central Primary Fibrosarcoma Maxilla - A Rare Presentation
Received: 27-Apr-2016 / Accepted Date: 30-May-2016 / Published Date: 06-Jun-2016 DOI: 10.4172/2161-119X.1000237
Keywords: Maxilla; Herringbone pattern; CT-scan (Computed Tomography-Scan); MRI (Magnetic resonance imaging); IHC (Immunohistochemistry)
251926Introduction
Fibrosarcoma (FS) is a malignant mesenchymal tumour with fibroblastic proliferation and variable amount of collagen production. In classical cases, herringbone architecture is seen [1]. FS essentially, is a diagnosis of exclusion, thus exact incidence rate cannot be assessed. It mostly accounts for 1-3% of adult sarcomas [1]. It is more frequently seen in soft tissue but primary intraosseous origin has been described in 5% of all cases [2,3]. It rarely affects head and neck region (10%). Mandible is the more common site of involvement in this region [4]. Maxilla is rarely involved and accounts for only 0 to 6.1% cases [5]. Involvement of maxillary antrum is rarely seen [3]. FS of jaw can be periosteal (peripheral) or endosteal (central) [4].
Secondary FS may arise in pre-existing fibrous dysplasia, paget’s disease, bone infarct, cyst andosteomyelitis or may present as malignant transformation of pre-existing giant cell tumors of bone or transformation of ameloblastic fibroma [6,7]. It has also been documented to be induced by prior history of irradiation [4].
Case Report
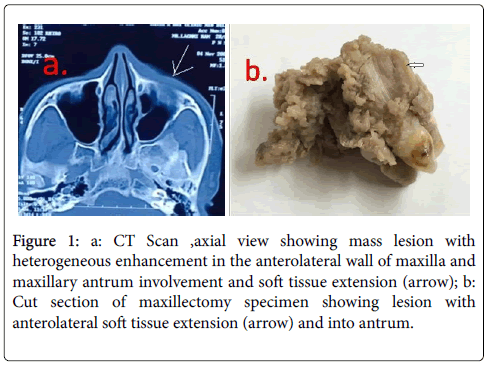
A 60 year old male patient presented with 10 months history of swelling and pain in left cheek region. On intraoral examination an ulceroproliferative growth was seen in the left premolar region with palatal and anterolateral extension as soft tissue swelling in the cheek. The premolar teeth were missing, which according to patient were extracted earlier as were loose. CT scan showed mass lesion in maxilla, with destruction of anterolateral wall and extension into anterior soft tissue as well as into the maxillary antrum (Figure 1a).
Figure 1: a: CT Scan ,axial view showing mass lesion with heterogeneous enhancement in the anterolateral wall of maxilla and maxillary antrum involvement and soft tissue extension (arrow); b: Cut section of maxillectomy specimen showing lesion with anterolateral soft tissue extension (arrow) and into antrum.
Incisional biopsy showed proliferation of spindle shaped cells arranged in proliferating bundles, fascicles and “herringbone pattern”, suggestive of Fibrosarcoma. Left partial maxillectomy was performed. Specimen of left partial maxillectomy measuring 10*4*2.5 cm was received. Grossly, an ulceroproliferative, firm, grey white growth measuring 5*3*3 cm on the alveolar ridge extending into maxillary antrum, eroding anterolateral and inferior wall of maxillawith absent overlying premolarteeth was noted. (Figure 1b) It was 4.5 cm away from posterior mucosal and 1. 8 cm from anterior mucosal margins.
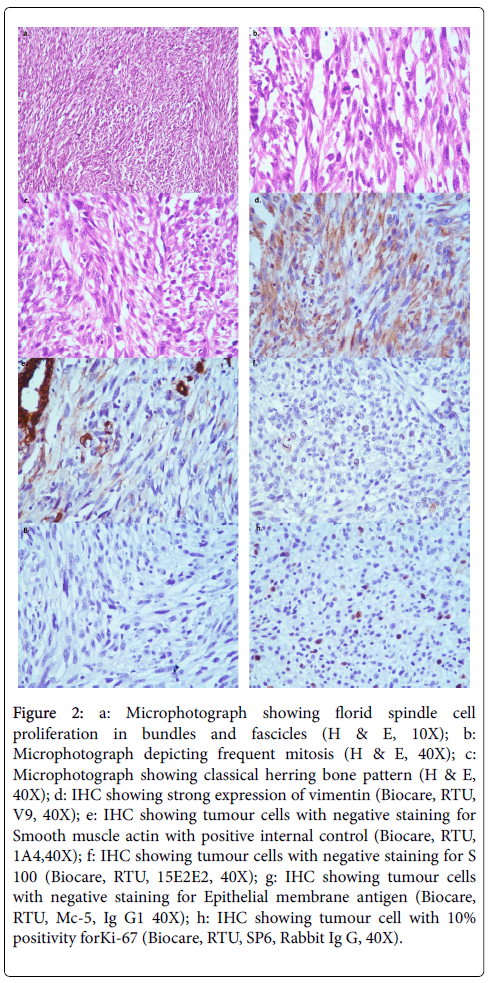
Multiple sections of tumour were taken and stained with Hematoxylin and Eosin (H&E). Sections showed spindle cells arranged in proliferating bundles, fascicles and “herringbone pattern”. Tumour cells showed elongated nuclei, coarse chromatin and tapering eosinophilic cytoplasm. Tiny focal loose myxoid areas were also seen. Tumour showed rich vascularity, focal necrosis, moderate degree of pleomorphism and 1-2 mitosis per high power field. Immunohistochemical stains stained were performed. Tumor cells showed positive staining for vimentin ((Biocare, RTU, V9) and ki-67 (Biocare, RTU, Mc-5, Ig G1) proliferation index was estimated at 10%.
The tumor cells were negative for S-100 (Biocare, RTU, 15E2E2), smooth muscle actin (SMA) (Biocare, RTU, 1A4) and Epithelial Membrane Antigen (EMA) (Biocare, RTU, Mc-5, Ig G1), HMB45 (Dako, RTU, HMB45, Ig G1D3), CD34 (Biocare, RTU, QBEnd/10), CD99 (Biocare, RTU, HO36-1. 1, IgG1)and Pan CK (Dako, RTU, AE1/3). Thus a final diagnosis of FS of maxilla (intermediate grade) was given Figure 2.
Figure 2: a: Microphotograph showing florid spindle cell proliferation in bundles and fascicles (H & E, 10X); b: Microphotograph depicting frequent mitosis (H & E, 40X); c: Microphotograph showing classical herring bone pattern (H & E, 40X); d: IHC showing strong expression of vimentin (Biocare, RTU, V9, 40X); e: IHC showing tumour cells with negative staining for Smooth muscle actin with positive internal control (Biocare, RTU, 1A4,40X); f: IHC showing tumour cells with negative staining for S 100 (Biocare, RTU, 15E2E2, 40X); g: IHC showing tumour cells with negative staining for Epithelial membrane antigen (Biocare, RTU, Mc-5, Ig G1 40X); h: IHC showing tumour cell with 10% positivity forKi-67 (Biocare, RTU, SP6, Rabbit Ig G, 40X).
Discussion
FS is malignant fibroblastic tumour, which rarely affects maxilla. It is more often seen to involve mandible than maxilla. Only in 0-6.1% cases, it involves maxilla [5]. It is more common in 5-6th decade, with equal sex predilection. However, an occasional case has been reported in pediatric age group too [6]. Patients are mostly asymptomatic. In 30% cases only, it may be symptomatic [2]. Patients mostly present with complain of swelling in jaw with or without pain. Other complaints are loosening of teeth, trismus, fracture and paresthesia [3,5,6].
Radiologically, it presents as osteolytic lesion with ill-defined margins, lacking any internal structures [8]. Thus in absence of any characteristic feature, it is difficult to distinguish it from other central malignant osteolytic lesion including carcinoma and myeloma, when no enlargement of jaw is noted. In some cases it may present as cystic lesion or with well circumscribed margins as documented by a few authors and then the differential of infected dental cyst and central desmoplastic fibroma arise. Ameloblastic fibrosarcoma, Ewing’s sarcoma, and radiolucent osteosarcoma can also show similar features [6,9,10]. On Computerized Tomography Scan (CT) it may present as destructive bony lesion, commonly associated with extra osseous soft tissue mass, as seen in this case [11]. Magnetic Resonant Imaging (MRI) shows low to intermediate signal intensity with inhomogeneous enhancement on both T1- and T2-weighted images with an inhomogeneous pattern of contrast enhancement [11].
The histopathological examination plays a very crucial role in identifying this tumour. Although, FS is essentially a diagnosis of exclusion but presence of certain definitive morphological features comprising of spindle shaped cells arranged in interlacing bundles, fascicles and “herringbone pattern” with variable amount of collagen deposition are helpful in reaching the diagnosis. Characteristically cells are spindle with elongated oval to round hyperchromatic nuclei, varying in size. Myxomatous, pseudomyxomatous and cartilaginous areas may also be noted [1-4].
Other malignant tumors which can be considered in its differential are spindle cell carcinoma, monomorphic synovial sarcoma, malignant fibrous histiocytoma, malignant nerve sheath tumors, leiomyosarcoma, and malignantamelanotic melanoma. Malignant peripheral nerve sheath tumour commonly shows spindle cells with serpentine nuclei with high mitotic rate and definitive S-100 positivity [12]. Monomorphic synovial sarcoma is a very close differential diagnosis and especially when it presents with sarcomatous spindle cell component, with co-expression of vimentin, CK and CD 99, absence of which rules its diagnosis [13]. Leiomyosarcoma comprises of fascicles of spindle-shaped cells with blunt ended vesicular nuclei, which are strongly positive for vimentin and smooth muscle actin [14]. Amelanotic melanomas can pose a problem but IHC helps in presence of HMB45, S100 [15]. Spindle cell carcinoma is usually biphasic and shows a strong positivity for EMA and Pancytokeratin [16]. Ameloblastic FS is also biphasic, showing presence odentogenic epithelial elements in some focus atleast. On Immunohistochemistry (IHC), strong vimentin positivity and negative S-100, SMA, desmin, EMA, CD99, CD34, CK, HMB45 help in ruling out other differential diagnosis and reach a conclusive diagnosis [12-16].
Tumour can be graded on the basis of their histological appearances by Broders’ method. Grade I (well differentiated) comprises of tumour cells with uniform nuclear appearance with appreciable amount of collagenous intracellular substance. Giant cell and mitotic figures are absent. Grade II (intermediate) comprises of tumour with increased cellularity and decreased amount of intracellular collagenous substance. Tumour cells have closely packed, uniform nuclei. Classical herring bone pattern is prominent with occasional mitotic figures. Grade III (high) comprises of anaplastic tumour cells with increased giant cells and mitotic figures. Our cases falls into intermediate grade with prominent herring bone pattern and uniform closely packed tumour nuclei [1,2]. Depending on the number of mitotic figures, tumor differentiation, and the presence of tumornecrosis, French Fédération Nationale des Centres de Lutte Contre le Cancer (FNCLCC) grading system is currently, the most widely accepted and according to this it was scored as grade 2 [1].
Management and follow up
Unlike soft tissue FS, osseous FS of bone has a poorer prognosis with 5year survival rate of only 4.231.7% [17]. A Primary vs. secondary site of origin and histological grading, play an important role in the prognosis of FS. Secondary FS usually have an aggressive course [3,8,18]. A difference in clinical course between FS of jaw and its long bone counterpart has been reported by many authors. A favourable prognosis of FS of jaw has been observed during the 5-20 year follow up observation period as compared with long bone fibrosarcoma [17]. FS of oral cavity also have lower rate of metastasis as compared to long bones [4]. The local recurrence has been reported has been reported as 50-60% and metastases in 20-25%, irrespective of the tumour grade. FS of long bones have 5 year survival rate of 4.3% to 31.7% whereas, in case of oral cavity it is 60% for soft tissue and 27% for medullary origin. Degree of differentiation has inverse relation with survival rate, higher grade of differentiation being associated with worse survival [4].
Preferred treatment modality is surgical resection with wide margin. In the FS that is not possible to excise completely, either due to their location or extreme size, postoperative radiotherapy of 60007, 000 cGy and postoperative adjunctive chemotherapy is suggested, to treat potential subclinical or microscopic metastasis especially in grade III FS [17]. However the role of adjuvant radiotherapy and/ or chemotherapy in the treatment is not very clear [4]. This case underwent surgical resection. His recovery was uneventful but subsequently presented with recurrence after 8 months and was referred for further treatment and subsequently lost for follow up.
Conclusion
FS is a malignant tumour of fibroblastic origin, which rarely affect maxillofacial region. Histopathological examination plays an important role. However in absence of classical herring bone pattern, differentiating it from other spindle cell lesions becomes a diagnostic dilemma. In such cases IHC plays a very important role by ruling out other differentials and planning the appropriate treatment.
References
- Fisher C, Van Den Berg E, Molenaar WM (2002) World Health Organization classification of tumours. Pathology and genetics of tumours of soft tissue and bone. Lyon, France: IARC Press.
- Huvos AG, Higinbotham NL (1975) Primary fibrosarcoma of bone. A clinicopathologic study of 130 patients. Cancer 35: 837-847.
- Mansouri H, Rzin M, Marjani M, SifatH, Hadadi K, et al. (2006) Fibrosarcoma of maxillary sinus. Indian Journal of Otolaryngology and head and neck surgery 58:104-105.
- Angiero F, Rizzuti T, Crippa R, Stefani M (2007) Fibrosarcoma of the jaws: Two cases of primary tumors with intraosseous growth. Anticancer Res 27: 2573-2581.
- Khanna S, Singh NN, Singh A, Purwar A (2014) Fibrosarcoma of maxilla with extension into maxillary sinus: A rare case report. Oral MaxillofacPatho J 5: 462-465.
- Swain N, Kumar SV, Dhariwal R, Routray S (2013) Primary fibrosarcoma of maxilla in an 8yearold child: A rare entity. J Oral MaxillofacPathol 17: 478.
- Reichart PA, Zobl H (1978) Transformation of ameloblastic fibroma to fibrosarcoma. Int J Oral Surg 7: 503-507.
- Rajendran A, Sivapathasundharam B (2012) Shafer's Textbook of Oral Pathology (7thedn) Elsevier.
- White SC, Pharoah MJ (2000) Oral Radiology: Principles and Interpretation (4thedn) St Louis, MO: Mosby.
- Khalili M, Shakib PA (2013) Ameloblasticfibrosarcoma of the upper jaw: Report of a rare case with long-term follow-up. Dent Res J (Isfahan) 10: 112-115.
- Razek AA (2011) Imaging appearance of bone tumors of the maxillofacial region. World J Radiol 3: 125-134.
- Das SR, Dash S, Pradhan B, Sahu MC, Padhy RN (2015) Malignant peripheral nerve sheath tumour of nose and paranasal sinuses with orbital extension Journal of Taibah University Medical Sciences 10: 238-242.
- Khalili M, Eshghyar N, Ensani F, Shakib PA (2012) Synovial sarcoma of the mandible. Journal of Research in Medical Sciences? The Official Journal of Isfahan University of Medical Sciences 17: 1082-1085.
- Chew YK, Noorizan Y, Khir A, Brito MS (2009) Leiomyosarcoma of the maxillary sinus. Med J Malaysia 64: 174-175.
- Saghravanian N, Pazouki M, Zamanzadeh M (2014) Oral amelanotic melanoma of the maxilla. J Dent (Tehran) 11: 721-725.
- Rath R, Das BK, Das SN, Baisakh MJ (2014) Spindle cell carcinoma of maxilla: Histomorphological and immunohistochemical analysis of a case Oral Maxillofac Pathol18: 256–261.
- Marx RE, Stern D (2002) Oral and maxillofacial pathology: A rationale for treatment. Hanover Park, IL: Quintessence Publishing.
- Slootweg PJ, Müller H (1984) Fibrosarcoma of the jaws. A study of 7 cases. J MaxillofacSurg 12: 157-162.
Citation: Sood N, Sehrawat N (2016) Central Primary Fibrosarcoma Maxilla - A Rare Presentation. Otolaryngol (Sunnyvale) 6:237. DOI: 10.4172/2161-119X.1000237
Copyright: © 2016 Sood N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 11321
- [From(publication date): 6-2016 - Jul 10, 2025]
- Breakdown by view type
- HTML page views: 10370
- PDF downloads: 951