Research Article Open Access
Closure of the Cystic Duct: Comparison to Harmonic Scalpel Versus Clip Application in Single Incision Laparoscopic Cholecystectomy
Huseyin Yilmaz*, Husnu Alptekin, Ilhan Ece, Akin Calisir and Mustafa Sahin
Department of General Surgery, Medical Faculty of Selcuk University, Konya, Turkey
- *Corresponding Author:
- Huseyin Yilmaz
Selcuk Universitesi A. Keykubat Kampusu
Selcuklu Tip Fakultesi Genel Cerrahi Klinigi 42075 Konya, Turkey
Tel: +903322415000
Fax: +903322412184
E-mail: hyilmazmd@hotmail.com
Received date: November 18, 2013; Accepted date: December 30, 2013; Published date: January 08, 2014
Citation: Yilmaz H, Alptekin H, Ece I, Calisir A, Sahin M (2014) Closure of the Cystic Duct: Comparison to Harmonic Scalpel Versus Clip Application in Single Incision Laparoscopic Cholecystectomy. J Gastroint Dig Syst 4:165. doi:10.4172/2161-069X.1000165
Copyright: © 2014 Yilmaz H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Backround: Single incision laparoscopic cholecystectomy [SILC] is usually performed using titanium clips [TC] for occlusion of the cystic duct and cystic artery. The use of Harmonic scalpel [HS] in SILC to be applied has been reported. In this study we aimed to compare effect of HS and TC application for closure of the cystic duct and artery in patients undergoing SILC.
Methods: Totally 70 patients were operated using SILC technique from May 2011 to Jan 2012. 37 patients underwent single incision laparoscopic cholecystectomy with titanium clips [TC-SILC] and 33 patients underwent single incision laparoscopic cholecystectomy with hormonic scalpel [HS-SILC]. In the TC-SILC group, closure of the cystic duct and artery was achieved by applying simple TC. In the HS-SILC group, HS was used for the closure and division of both cystic duct and artery. Demographics, diagnosis, operative data, complications and length of hospital stay were compared between the two groups.
Results: Patients demographics were not different between the groups. Conversion to open surgery or need of additional port was not necessary in any patient. The operative data were similar in both groups. Superficial wound infection was seen in one patient in TC group which was trated by oral antibiotics. During the follow-up period, one port-site hernia was detected in a patient who underwent TC-SILC.
Conclusions: The HS seems to be a feasible, effective and a safe technique for performing SILC on selected patients. However, complications of TC was thought to be rare in experienced hands, and the cost of HS should be also considered prior to adopting the technique.
Keywords
Laparoscopy; Single incision; Cystic duct ligation
Introduction
Today laparoscopic cholecystectomy [LC] is accepted as the ‘’gold standard’’ surgical treatment of gallbladder benign diseases due to its optimal postoperative results and enhanced quality of the life [1,2]. Single-incision laparoscopic operations have recently emerged as used in minimal invasive alternative to conventional laparoscopy. HS is used to the single incision laparoscopic cholecystectomy [SILC] for laparoscopic removal of the gallbladder safely, short surgical time and a shorter length of hospital stay [3].
The standard LC is usually performed using monopolar electrosurgical hook for dissection and clips for ligation of the cystic duct and cystic artery. Standard closure of cystic duct during LC by titanium surgical clips [TC] is the most frequently used technique to achieve both cystic duct and artery closure [4,5]. In LC, alternative techniques for duct ligation have included linear stapler, endoloops, knot and HS [3,6]. Recently SILC is usually performed using titanium clips [TC-SILC] for occlusion of the cystic duct and cystic artery.
Several studies have described the use of ultrasound dissection technology in LC where ultrasonic devices have been used in dissection of the gallbladder [7,8]. The ultrasonically activated scalpel [HS, Harmonic Scalpel-Ethicon Endo Surgery INC] was introduced into clinical use more than two decades ago. Its technology relies on the application of ultrasound within the harmonic frequency range to tissues and allows two effects: ultrasonic coagulation and cutting [9]. Large series studies have demonstrated the effectiveness and safety of the use of the HS for dissection of the gallbladder [10,11], some researchers have found that the titanium clip to be more effective for closure of cystic duct and artery [12]. The HS is also an effective device for closure of biliary ducts and vessels whose diameter is <4 mm to 5 mm [as certified by the FDA in 2006]. In recent years, variable energy sources have been tried in SILC for closure of the cystic duct. The use of HS scalpel in SILC [HS-SILC] for laparoscopic removal of the gallbladder was reported by Geidie [3]. It was the only published report about usage of HS in SILC. Moreover, comparative studies are needed.
The aim of this retrospective study is to compare the HS and the standard TC, with respect to efficacy and safety for a correct and complete closure and division of the cystic duct and artery in SILC.
Methods
We began performing HS-SILC in our department in May 2011. Up to Jan 2012, 33 patients underwent HS-SILC and 37 patients underwent TC-SILC. After institutional review board approval [no: 2012/19], follow-up data was obtained from hospital charts and office records. The data included operative time [defined as the time from after placement of the port or trocars to removal of the gallbladder out of the abdomen], gender, age, body mass index [BMI], ASA [American Society of Anesthesiologists score] classification, comorbidities, length of hospital stay [defined as the time from the post anesthesia care unit until discharge from the hospital], operative complications and short-term outcomes. Patients were reexamined at 2 and 4 weeks postoperatively. Postoperative evaluation was conducted by a surgeon who was not aware of the study groups. The patients were contacted by telephone in January 2012 for recorded to short-term outcomes. Postoperative data of patients with missing notes or telephone contact could not be documented, therefore excluded from the study.
Surgical Technique
Patients selected for the SILC approach had uncomplicated symptomatic gallstone disease, verified by ultrasonography. Antibiotic prophylaxis was administered preoperatively with 1gr cefazolin sodium.
Exclusion criterias for the SILC approach were patients with common bile duct stones, acute cholecystitis, previous upper abdominal operation, suspicion of gallbladder malignancy based on ultrasonography, subsequent computed tomography [CT] findings, pregnant patients and morbid obesity [body mass index over 40 kg/ m2]. Patients with abnormal serum bilirubin, alkaline phosphatase and gamma glutamyl transferase levels were also excluded. All SILC were performed by the same team with experience of about 150 SILC the same approach and techniques were adopted to all procedures.
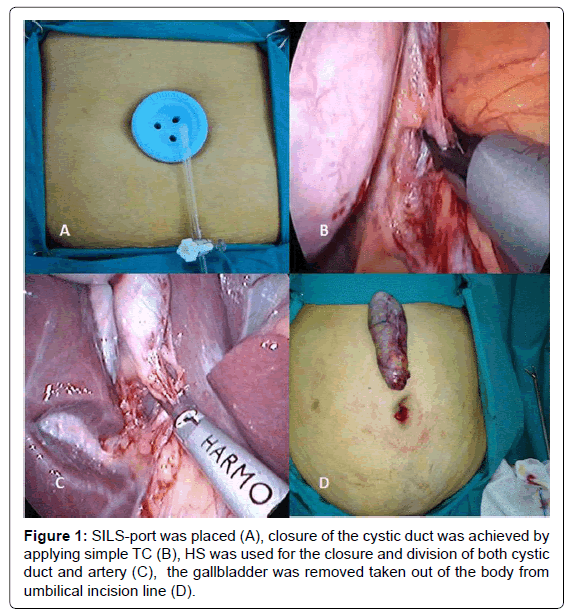
Operative procedures were performed under general anesthesia and the patients were positioned in the supine position with 30-degree head up and right side up. The surgeon stood between the patient’s legs. Camera assistant stood to the patient’s left. The same access technique was used in all patients. Skin and subcutaneous tissues were passed with a 20 mm transverse incision in a standard manner in all cases. The abdomen was entered with a transverse fascia incision. Port manufactured for single-incision laparoscopic surgery [SILS port Covidien©. USA.] was placed (Figure 1A). Intraabdominal pressure was elevated to 12 mmHg with insuflation. The abdomen was entered via the specific ports with 2 (5 mm) and 1 (12 mm) trocar. 5 mm, 30° laparoscope was used. Gallbladder was suspended using a grasper. Dissection of the gallbladder was initiated at the triangle of Calot with the identification and skeletonization of both the cystic duct and artery. Relation between the main bile duct and cystic duct was displayed.
In the Group TC, dissection of Calot’s triangle was performed with an atraumatic dissecting forceps. Closure of the cystic duct and artery was achieved by applying simple TC via 12 mm trocar (Figure 1B). Artery and cystic duct were divided with endoscopic scissors. Mobilization of the gallbladder from the liver bed started posterior to the Calot’s triangle and was seperated from the liver via hook cautery. Gallbladder was removed through umblical incision and endobag was not used in any patient.
In the Group HS, the HS was used for the closure and division of both cystic duct and artery. Closure and division of the cystic duct proceeded as follows: [i] the instrument was set at the power level 2 which translated into less cutting and more coagulation, [ii] the cystic duct was faced between the jaws at a safe distance from the common bile duct to avoid damage to this structure, and the jaws were then closed (Figure 1C), [iii] the instrument was activated until the gallbladder was detached from the cystic duct. Finally, the gallbladder was removed from liver bed using HS and taken out of the body via the umbilical incision (Figure 1D).
A laparoscopic exploration was then performed to ensure that there were no intraoperative complications, such as organ injuries, bleeding or biliary leakege. After removing the ports and releasing the residual carbon dioxide, the fascial defect was closed with No.1 loop prolene. Skin was sutured in an intradermic fashion using vicryl.
Statistical Analysis
Demographic data and perioperative data were compared using Student’s t test for continuous variables and Fisher’s exact test for categorical variables. The level of significance was set at 0.05.
Results
A total of 70 patients were operated using with SILC technique from May 2011 to Jan 2012. Three patients undergoing HS-SILC and 2 patients undergoing TC-SILS were excluded because of missing data in files. The mean follow-up period for the 65 responding patients was 5.2 months, ranging from 1 month to 8 months. Their demographic data was shown in Table 1. Patient’s demographics were not different between groups.
| TC Group (37 patients) | HS Group (33 patients) | P-value | |
|---|---|---|---|
| Age Range Mean ±SD Sex Female Male BMI(kg/m2) Mean ±SD Associated co-morbidities Hipertension Diabetes Mellitus BrochialAstma |
|
28,32 ± 2,14 |
not significant not significant not significant not significant |
TC, used to titanium clip for SILC group; HS, used to harmonic scalpel for SILC group; SD,
Table 1: Demographic characteristic of the patients.
Open surgery or need for an additional port was not necessary in any patient. The operative data were similar in both groups (Table 2). Superficial wound infection we seen in one patient in group TC which was treated by oral antibiotics. During the follow-up period, one port-site hernia was detected in a patient who underwent TCSILC.
| TC Group (37 patients) | HS Group (33 patients) | P-value | |
|---|---|---|---|
| Operative time(min) Range Mean ±SD Postop complication Port-site infection Port-site Herni Length of hospital stay (LHS) |
20-37 27,37 ± 5,11 1 1 1,64 ± 1,08 |
12-36 24,13 ± 6,51 - - 1,40 ± 1,24 |
not significant not significant |
TC, used to titanium clip for SILC group; HS, used to harmonic scalpel for SILC group; SD, standard deviation.
Table 2: The incidence of operative time, postoperative complication and length of hospital stay in both groups.
Discussion
Single-incision laparoscopic cholecystectomy was first described in 1997 via two incisions placed in the periumbilical region [13]. Although the technique has many names since its first description, SILC is the most widely accepted terminology. The most important advantage of SILC is that it can be completely performed using conventional laparoscopic instruments [14]. El-Geidie’s [3] report is the first in the literature that showed no bile leaks from the cystic duct stump in his 67 patients in whom the closure and division of the cystic duct was achieved using only the HS in SILC.
Closure of cystic duct during laparoscopic cholecystectomy using TC is the most frequently used technique [4,5]. Wise et al. [15] demonstrated that simple titanium clips applied to the cystic duct could not be displaced by a pressure of 300 mmHg. Unfortunately, the literature provides various examples of cystic-duct leakage, due to inadequate closure of the duct, due to mismatch of the clip arms, necrosis of the duct at the site of clipping, or slippage of the clips off the end of the duct and migration into the biliary tract [16-19]. In recent years, some energy sources have been tried for the closure of the cystic duct. The use of ultrasonically activated shears for both dissection and closure-division of the cystic duct and artery was reported [3,5,10,12,20]. Westervalt [12] reported no bile leaks from the cysticduct stump in his 100 patients in whom the closure and division of the cystic duct was achieved solely by the harmonic shears. Kavlakoglu et al. [21] was performed a study to compare the cystic duct bursting pressure of TC, HS, and plasmakinetic sealer. They have identified the bursting pressure [343 mmHg] in the HS group higher than the TC group [326 mmHg].
The use of HS was accepted as a reasonable alternative for closure of cystic ducts <6 mm in diameter [22,23]. Studies have shown that the HS is an effective and safe tool for the closure of both the cystic duct and artery in patients who undergo laparoscopic cholecystectomy [22,24].
Although average operative time does not show a statistically significant difference between the group the TC and group HS, it seems to be relatively shorter operation time HS group. The HS replaces four instruments [scissors, clip applier, dissector, and hook cautery]. This is because of the use of the HS as the sole instrument, which prevents the extraction and insertion of different instruments and subsequent waste of time. Thus, the risk of organ injuries may decrease and the ergonomics of laparoscopic surgery may be enhanced by allowing the surgeon to concentrate on the operating field and not to be distracted with the continuous changing of instruments [25,26]. In addition, HS hardly produces any smoke [21]. Thus, the visibility of the operative field is preserved during the whole procedure and no time is spent on clearing the vision.
Limitation of our study is that it has not compared the cost. On the other hand HS are quite expensive when compared with the price of titanium clip, an average of 10 times. There is the added disadvantage of lost efficiency caused by other instrument change such as dissectors and scissors. It should be noted that reusable clip application are now available. Clearly HS is very expensive. For this reason, we do not need a price comparison.
In conclusion, the HS seems to be a feasible, effective and safe technique for performing SILC on selected patients, and divided to groups randomly.
References
- Keus F, Broeders IA, van Laarhoven CJ (2006) Gallstone disease: Surgical aspects of symptomatic cholecystolithiasis and acute cholecystitis. Best Pract Res Clin Gastroenterol 20: 1031-1051.
- Mufti TS, Ahmad S, Naveed D, Akbar M, Zafar A (2007) Laparoscopic cholecystectomy: an early experience at Ayub Teaching Hospital Abbottabad. J Ayub Med Coll Abbottabad 19: 42-44.
- El-Geidie AA (2012) Single-incision laparoscopic cholecystectomy (SILC) using harmonic scalpel. J Surg Res 176: 50-54.
- Rohatgi A, Widdison AL (2006) An audit of cystic duct closure in laparoscopic cholecystectomies. Surg Endosc 20: 875-877.
- Yano H, Okada K, Kinuta M, Nakano Y, Tono T, et al. (2003) Efficacy of absorbable clips compared with metal clips for cystic duct ligation in laparoscopic cholecystectomy. Surg Today 33: 18-23.
- Nathanson LK, Easter DW, Cuschieri A (1991) Ligation of the structures of the cystic pedicle during laparoscopic cholecystectomy. Am J Surg 161: 350-354.
- Tsimoyiannis EC, Jabarin M, Glantzounis G, Lekkas ET, Siakas P, et al. (1998) Laparoscopic cholecystectomy using ultrasonically activated coagulating shears. Surg Laparosc Endosc 8: 421-424.
- Hüscher CG, Lirici MM, Di Paola M, Crafa F, Napolitano C, et al. (2003) Laparoscopic cholecystectomy by ultrasonic dissection without cystic duct and artery ligature. Surg Endosc 17: 442-451.
- Gossot D, Buess G, Cuschieri A, Leporte E, Lirici M, et al. (1999) Ultrasonic dissection for endoscopic surgery. The E.A.E.S. Technology Group. Surg Endosc 13: 412-417.
- Amaral JF (1995) Laparoscopic cholecystectomy in 200 consecutive patients using an ultrasonically activated scalpel. Surg Laparosc Endosc 5: 255-262.
- Wetter LA, Payne JH, Kirshenbaum G, Podoll EF, Bachinsky T, et al. (1992) The ultrasonic dissector facilitates laparoscopic cholecystectomy. Arch Surg 127: 1195-1198.
- Westervelt J (2004) Clipless cholecystectomy: broadening the role of the harmonic scalpel. JSLS 8: 283-285.
- Navarra G, Pozza E, Occhionorelli S, Carcoforo P, Donini I (1997) One-wound laparoscopic cholecystectomy. Br J Surg 84: 695.
- Oruc MT, Ugurlu MU, Boyacioglu Z (2012) Transumbilical multiple-port laparoscopic cholecystectomy using standard laparoscopic instruments. Minim Invasive Ther Allied Technol 21: 423-428.
- Wise Unger S, Glick GL, Landeros M (1996) Cystic duct leak after laparoscopic cholecystectomy. A multi-institutional study. Surg Endosc 10: 1189-1193.
- Hanazaki K, Igarashi J, Sodeyama H, Matsuda Y (1999) Bile leakage resulting from clip displacement of the cystic duct stump: a potential pitfall of laparoscopic cholecystectomy. Surg Endosc 13: 168-171.
- Nelson MT, Nakashima M, Mulvihill SJ (1992) How secure are laparoscopically placed clips? An in vitro and in vivo study. Arch Surg 127: 718-720.
- McMahon AJ, Fullarton G, Baxter JN, O'Dwyer PJ (1995) Bile duct injury and bile leakage in laparoscopic cholecystectomy. Br J Surg 82: 307-313.
- Labuski MR, Wise SW (1999) Recurrent abdominal abscess secondary to a dropped laparoscopic clip: CT imaging. Abdom Imaging 24: 191-192.
- Janssen IM, Swank DJ, Boonstra O, Knipscheer BC, Klinkenbijl JH, et al. (2003) Randomized clinical trial of ultrasonic versus electrocautery dissection of the gallbladder in laparoscopic cholecystectomy. Br J Surg 90: 799-803.
- Kavlakoglu B, Pekcici R, Oral S (2011) Clipless cholecystectomy: which sealer should be used? World J Surg 35: 817-823.
- Bessa SS, Al-Fayoumi TA, Katri KM, Awad AT (2008) Clipless laparoscopic cholecystectomy by ultrasonic dissection. J Laparoendosc Adv Surg Tech A 18: 593-598.
- Vu T, Aguilo R, Marshall NC (2008) Clipless technique of laparoscopic cholecystectomy using the harmonic scalpel. Ann R Coll Surg Engl 90: 612.
- Tebala GD (2006) Three-port laparoscopic cholecystectomy by harmonic dissection without cystic duct and artery clipping. Am J Surg 191: 718-720.
- Hüscher CG, Lirici MM, Anastasi A, Sansonetti A, Amini M (1999) Laparoscopic cholecystectomy by harmonic dissection. Surg Endosc 13: 1256-1257.
- Hüscher CG, Lirici MM, Di Paola M, Crafa F, Napolitano C, et al. (2003) Laparoscopic cholecystectomy by ultrasonic dissection without cystic duct and artery ligature. Surg Endosc 17: 442-451.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15704
- [From(publication date):
February-2014 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 11002
- PDF downloads : 4702