Colosalpingeal Fistula: Rare Complication of Sigmoid Diverticulitis
Received: 02-Oct-2017 / Accepted Date: 17-Oct-2017 / Published Date: 23-Oct-2017 DOI: 10.4172/2167-7964.1000277
Introduction
Colonic diverticulosis is a common entity and sigmoid colon is the most commonly affected colonic segment [1]. Patients are usually asymptomatic but frequently super added complication of diverticulitis [1] make the presence of this condition clinically overt. Currently Computed Tomography (CT) plays a major role in detection of diverticulitis and its associated complications [2]. In the background of diverticulitis various fistulous communications of sigmoid colon with adjacent organs have been described, colovesical fistula being the most common [3]. Fistulous communication between colon and fallopian tube (colosalpingeal fistula) develop when either of them have diseased wall which can be secondary to pelvic tubal infections or pelvic malignancies, however few cases have been reported in background of diverticulitis. We present a rare case of colosalpingeal fistula complicating sigmoid diverticulitis which was detected and followed up on Computed Tomography (CT).
Case
A 45 year old post-menopausal woman presented with non-colicky persistent left lower abdominal and pelvic pain for two weeks without any associated bowel complaint or dysuria. There was scanty serous vaginal discharge few days after onset of pain. There was no significant past history. On clinical examination patient was afebrile with stable vitals. Mild tenderness was noted in the left lower abdomen. Pelvic examination revealed mild left adnexal tenderness. Lab parameters showed mild leucocytosis (12000/mm3) and elevated C-reactive protein. CT examination was advised keeping in mind the possibility of inflammatory bowel or adnexal pathology.
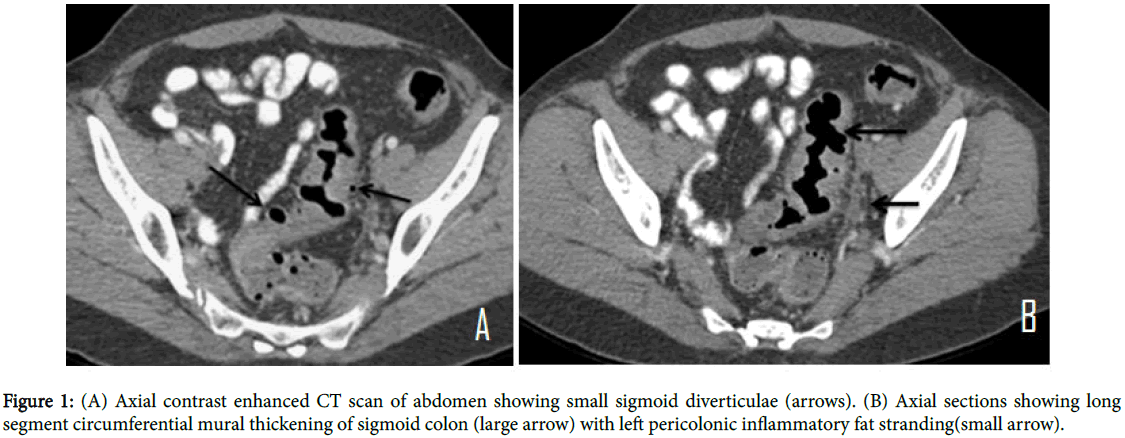
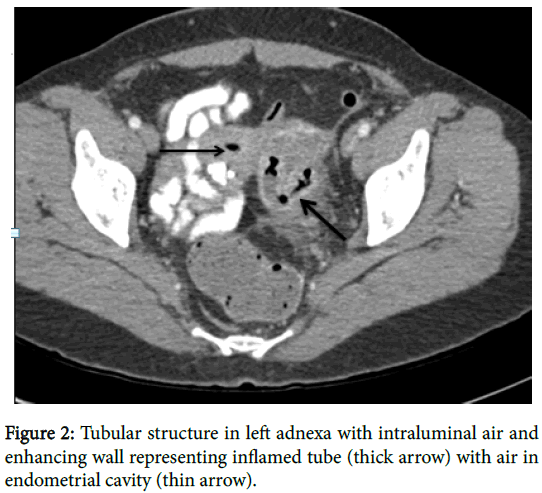
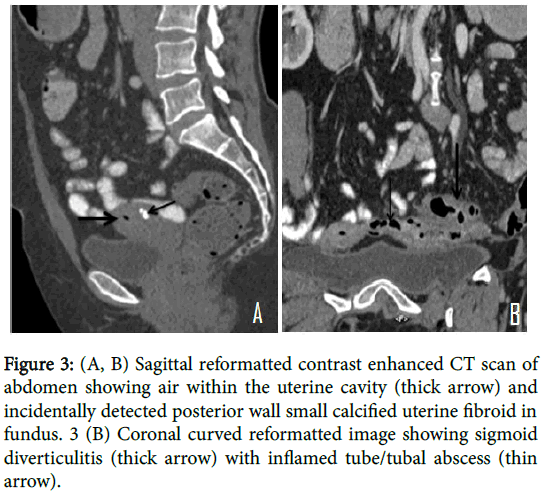
CT revealed multiple small diverticulae with symmetrical circumferential mural thickening of the long segment (7-8 mm in thickness) of sigmoid colon and pericolonic fat stranding. In addition, a linear air filled tubular structure with enhancing walls was noted adjacent to thickened sigmoid colon extending to the left uterine cornu likely representing inflamed tube/tubal abscess with air foci within the uterine endometrial cavity. Findings were suggestive of colosalpingeal fistula. Patient was managed conservatively with antibiotics. Follow up CT done after 4 weeks of antibiotic therapy showed reduction of inflammatory changes in the sigmoid colon and in left adnexa. Sigmoidoscopy done after follow up CT reveal sigmoid diverticuli with inflammatory changes but no definitive fistulous opening (Figures 1-3).
Figure 3: (A, B) Sagittal reformatted contrast enhanced CT scan of abdomen showing air within the uterine cavity (thick arrow) and incidentally detected posterior wall small calcified uterine fibroid in fundus. 3 (B) Coronal curved reformatted image showing sigmoid diverticulitis (thick arrow) with inflamed tube/tubal abscess (thin arrow).
Discussion
Colonic diverticular disease is a common disorder affecting the elderly [2]. Though any colonic segment may be involved, sigmoid colon is the most commonly affected segment [1]. Small calibre with multiple colonic haustrations in sigmoid colon leads to frequently increased intracolonic segmental pressure [4] and herniation of mucosal layer through the colonic muscle layer forming small air filled outpouchings.
Diverticulitis develops when stagnation [2] occurs due to occlusion of diverticular neck by hard stool or food particles leading to increased pressure within the sac and vascular compromise which favours bacterial invasion leading to mucosal ulceration and microperforations. Various imaging modalities [5] have been used for the detection of diverticulosis and its complications however CT is the preferred modality [1] due to its ability to detect complications of diverticulitis and assess response after treatment. CT [2] can show the extent and multifocality of disease. Complications like perforation, pericolonic abscess, intestinal obstruction, fistulisation and pylephlebitis can be accurately diagnosed.
Sigmoid diverticulitis complicated by fistulisation is seen in 20% patients [6] undergoing surgery for the disease, colovesical fistula being the most common [3]. Fistulisation with pelvic genital organs in female patients has been described, the commonest being colovaginal fistula [3] while with fallopian tube (colosalpingeal fistula) is the least common [6]. Other pathological conditions reported to be associated with salpingoenteric fistula are - tubercular or pyogenic salpingitis, as obstetric complication during caesarean or forceps delivery and due to intrauterine contraceptive device perforation [6]. Pelvic bowel or ovarian malignancies can secondarily invade fallopian tube [7] or it can be seen as a complication of Crohn’s disease [7]. Due to close proximity of the fallopian tube and sigmoid colon communication can develop when either of them have diseased wall.
Colosalpingeal fistula can be clinically suspected when there are associated genito-urinary symptoms like vaginal discharge, in a known case of sigmoid diverticulitis. Various imaging modalities can help in the diagnosis as in previous reported cases in which the fistula was demonstrated either on hysetrosalpingography [7] or on barium enema [6] and radiological findings was confirmed surgically. Few cases have been reported primarily on CT [8,9] where authors described a case of left parauterine tubo-ovarian abscess containing air associated with sigmoid diverticulitis with operative findings confirming a colosalpingeal fistula. In our case CT demonstrated the inflamed left fallopian tube containing air which was seen extending from the thickened sigmoid colon up to the uterine cornu with air in the uterine cavity. Though definitive confirmation is always surgical imaging modalities specially computed tomography play an important role in diagnosis and follow up of patients which respond to conservative management.
Initially most patients are managed conservatively with liquid diet and antibiotics with requirement of surgical drainage of clinically significant pelvic abscess in a few [9] patients. However, in cases where conservative management fails with persistence of symptoms treatment is primarily surgical, aiming at removal of the diseased colon by colonic resection and for fistula either hysterectomy in postmenopausal women or unilateral salpingo-opherectomy in premenopausal women [10]. In cases of diverticulitis which respond to medical management and patient is asymptomatic for fistula as in our case, close follow can be done as spontaneous fistula closure had been reported earlier [10].
Conclusion
Sigmoid diverticulitis and associated complications is not an uncommon entity and radiologist should be aware of the fact that in patients with sigmoid diverticulitis, the presence of an adnexal inflammatory air containing lesion with air in the uterine cavity on CT should suggest the presence of colosalpingeal fistula, early diagnosis of which is essential for appropriate management. Genitourinary complaints in clinical background of sigmoid diverticulits further points towards this rarer entity. This case further strengthens the importance of CT scanning in these patients to reach upon the correct diagnosis.
References
- Tonelli F, Di Carlo V, Liscia G, Serventi A (2009) Diverticular disease of the colon: diagnosis and treatment. Ann Ital Chir 80: 3-8.
- Werner A, Diehl SJ, Farag-Soliman W, Duber C (2003) Multi-slice spiral CT in routine diagnosis of suspected acute left-sided colonic diverticulitis: a prospective study of 120 patients. Eur Radiol 13: 2596-2603.
- Tappenden J, Shrestha BM (2008) Colonic diverticular disease: current perspectives. J Nepal Med Assoc 46: 206-213.
- Painter NS (1975) Pressures in the colon related to diverticular disease. Proc R Soc Med 63: 144-155
- DeStigter KK, Keating DP (2009) Imaging update: acute colonic diverticulitis. Clin Colon Rectal 22: 147-155.
- Williams SM, Nolan DJ (1999) Colosalpingeal fistula: A rare complication of colonic diverticular disease. Eur Radiol 1432-1433
- Ogbeide OU, Ukadike IA, Ehigiamusoe FO, Okonofua FE (2010) Acquired salpingo-enteric fistula-a case report. Afr J Reprod Health 14: 139.
- Tonolini M, Bianco R (2012) Tubo-ovarian abscess complicating sigmoid colon diverticulitis. Euro Rad.
- Pannghaal VS, Chernvak V, Patkas M, Rozenblit AM (2009) CT features of adnexal involvement in patients with diverticulitis. Am J Roentgenol 192: 963-966.
- Hai JM, Sherick DG (1996) Salpingocolonic fistula secondary to diverticulitis. Am Surg 12: 984-986.
Citation: Kumar S, Sharma R, Madhusudhan KS, Valakkada J, Nandi B, et al. (2017) Colosalpingeal Fistula: Rare Complication of Sigmoid Diverticulitis. OMICS J Radiol 6: 277. DOI: 10.4172/2167-7964.1000277
Copyright: © 2017 Kumar S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 7216
- [From(publication date): 0-2017 - Nov 10, 2025]
- Breakdown by view type
- HTML page views: 6161
- PDF downloads: 1055