Cytomegalovirus, Parvovirus B19 and Rubella Co-Infection among Pregnant Women Attending Antenatal Clinics in Mwanza City: The Need to be considered in Tanzanian Antenatal Care Package
Received: 28-Jan-2016 / Accepted Date: 07-Mar-2016 / Published Date: 14-Mar-2016 DOI: 10.4172/2161-1165.1000230
Abstract
Background: Viral infections are common in pregnancy and have been associated with poor pregnancy outcome. In many developing countries including Tanzania, the magnitude of these infections and their impact to pregnancy outcome is not clearly understood. The aim of this study was to determine the magnitude of these infections. The information from this study may influence policy makers to consider routine screening of these infections during antenatal visits.
Methods: A cross sectional hospital based study involving 214 pregnant women was conducted between December 2014 to and August 2015 in two antenatal clinics in Mwanza city. Rubella, cytomegalovirus and parvovirus B19 (B19) specific IgG and IgM antibodies were detected by using commercial indirect enzyme linked immunosorbent assay. Data were analyzed using STATA version 11.
Results: The median age of enrolled pregnant women was 21 (Interquartile range: 20-26) years. Previous co-infections of rubella, cytomegalovirus and B19 was detected in 78 (36.5%) of pregnant women tested. A total of 20 (9.4%) pregnant women had acute co-infection of rubella and parvovirus B19 while 1(0.5%) had acute co-infection of cytomegalovirus and parvovirus B19. The odds of having previous co-infection (IgG sero-positivity) increase significantly as the age increases (odd ratio: 1.056, 95% CI: 1.00-1.11, P=0.03). Moreover, as the gestation age increases the odds of having co-infection decreases significantly (odd ratio: 0.923, 95% CI: 0.88-0.96, P=0.001).
Conclusion: Considerable proportion of pregnant women in Mwanza is co-infected with rubella, Cytomegalovirus and parvovirus B19. We recommend routine screening for these infections during antenatal visits so as to reduce the possibility of congenital infection.
Keywords: Rubella; Cytomegalovirus; Parvovirus B19; Co-infection; Antenatal; Mwanza
164363List of abbreviations
CMV: Cytomegalovirus; ELISA: Enzyme Linked Immunosorbent Assay; IgG: Immunoglobulin gamma; IgM: Immunoglobulin mu; OR: Odd ratio
Introduction
Congenital intrauterine infections have been associated with poor pregnancy outcome ranging from spontaneous abortions, still births, congenital malformations, intrauterine growth restriction, fetal deaths, developmental delay and many other sequels that can be seen later in life [1]. Cytomegalovirus (CMV), rubella and parvovirus B19 (B19) infections are among the principal blood borne viral infections that are transmitted transplacentally [2]. Primary and secondary of these infections in pregnant women are often inconspicuous, but may result into serious fetal damage [3-5]. With exception of few countries like Nigeria, epidemiology of these infections in pregnancy is not well documented in Africa. More than 85% of adults are infected with CMV in developed countries, and the prevalence has been found to be higher among adults and pregnant women in countries with low socio economic status [6,7]. On the other side, natural immunity to rubella among pregnant women in Africa, has been found to range from 52.9 to as high as 97.9% indicating high transmission rates [8].The data regarding the magnitude of Parvovirus B19 in many developing countries are scarce but have been found to be higher worldwide with sero-conversion rates ranging from 3 to 34% during pregnancy [9-11].
Despite their importance, the magnitude of these infections and coinfections during pregnancy remain poorly understood in many developing countries including Tanzania. A single published report on rubella during pregnancy exists in Tanzania [12], with no single published report on B19 and CMV among pregnant women. Early detection and fetal monitoring of these infections during pregnancy might assist appropriate counseling on potential adverse pregnancy outcomes. The information obtained from this study may influence policy makers to include screening of these infections in the current antenatal package.
Method and Material
A cross sectional hospital based study was carried out between December 2014 and August 2015 involving pregnant women from Makongoro and Karume antenatal clinics representing urban and rural areas respectively as defined by Mwanza city council. After obtaining written informed consent from participants, 4-5 ml of blood were collected using plain vacutainer tubes (Becton, Dickinson and Company, Nairobi, Kenya) and transported to the Bugando multipurpose laboratory whereby sera were separated and stored in cryovials at -40°C freezer until processing. Standardized data collection tool was used to obtain socio-demographic information. Data collected included; age, gestation age, parity, residence, education level and socio-economic status. Women with no formal education and primary education attendees were considered having low education level while those attained secondary and tertiary education were considered having higher education level. Good social economic status was defined as being educated with sustainable income or having any income generating activities [13].
Laboratory procedures
Quantitative and qualitative detection of specific rubella, CMV and B19 IgM and IgG antibodies were done by using commercial indirect enzyme-linked immunosorbent assay (ELISA) (Pishtaz Teb Diagnostics kits, Iran). Consequential steps carried out according to protocols of Pishtaz Teb Corporations (https://www.pishtazteb.com) using ChemWell® 2910-Awareness Technology Inc. USA. These IgG and IgM assays have been found to have sensitivity and specificity of >95% [14-17]. Before performing the test the method was calibrated by using the provided standards and controls to obtain a standard curve.
Data management and analysis
Data were entered using Microsoft Office Excel 2007 and analyzed using the STATA version 11 (College Station, Texas, USA). Categorical variables were summarized as proportions while continuous variables were summarized as median with interquartile range. Univariate logistic regression analysis was done to investigate association of coinfections with gestational age and age of participants. Odds ratio (OR) and 95% confidence interval [95% CI] were noted and a p value of < 0.05 was considered significant.
Ethical clearance
The protocol for conducting the study was approved by the Joint Catholic University of Health and Allied Sciences/Bugando Medical Centre (CUHAS/BMC) research ethics and review committee (CREC). Permission was sought from hospital/clinic administration and written informed consent was obtained from each participant prior enrolment to the study.
Results
The median age of enrolled pregnant women was 21(IQR: 20-26) years while median gestation age was 14 (IQR: 10.5-18) weeks. As defined by the city council; majority of participants 146 (68.2%) were from urban areas. A total of 172 (80.37%) had low education level while 126 (58.9%) had good socioeconomic status. Of 214 women, 101 (47.2%), 87 (40.7%) and 26 (12.2%) were in first, second and third trimester respectively.
The overall prevalence of previous co-infection was 36.5%, while none of the 78 pregnant women with co-infection had acute infections of all three viruses (Table 1). However, 20 (9.4%) had acute infection of both rubella and parvovirus B19, while 1 (0.5%) was acutely coinfected with CMV and B19 having and had natural immunity to rubella (Table 1).
| Virus | IgG | IgM |
|---|---|---|
| Individual infections | ||
| CMV | 167(78.04%) | 1(0.5%) |
| B19 | 118 (55.1%) | 76 (35.5%) |
| Rubella | 188 (87.9%) | 48 (22.4) |
| Co-infections | ||
| CMV +B19 | 87(40.6%) | 1(0.5%) |
| CMV+ Rubella | 146 (68.2%) | 0 |
| Rubella +B19 | 105 (49.06%) | 20 (9.3%) |
| CMV+Rubella+B19 | 78 (36.5%) | 0 |
Table 1: Proportions of pregnant women co-infected with CMV, Rubella and B19 viruses in Mwanza.
Infections with gestational age; for CMV as gestation increases the IgG seropositivity was found to decrease significantly while no statistical difference was seen between parvovirus B 19 and rubella IgG seropositivity and gestation age Table 2. Regarding IgM seropositivity, for rubella seropositivity was significantly higher in first trimester than in second and third trimester (31.7% vs. 14.9% vs. 11.5%, P<0.002) Table 2.
| Trimester | CMV | Rubella | B19 | Co-infection |
|---|---|---|---|---|
| IgG | ||||
| 1st (101) | 91(90.1%) | 87% (86.1%) | 57(56.4%) | 43(42.6%) |
| 2nd (87) | 67(77%) | 80(91.9%) | 52(59.8%) | 35(40.2%) |
| 3rd (26) | 9(34.6%) | 21(80.7%) | 9(34.6%) | 0(0%) |
| P value | <0.014 | >0.05 | <0.07 | |
| IgM | ||||
| 1st (101) | 0(0.0%) | 39(38.6%) | 32(31.68%) | - |
| 2nd (87) | 1(0.15%) | 27(31.03%) | 13(14.9%) | - |
| 3rd (26) | 0(0.00%) | 10(38.5%) | 3(11.5%) | - |
| P value | >0.05 | <0.02 | ||
Table 2: Gestation age and CMV, rubella and B19 infections.
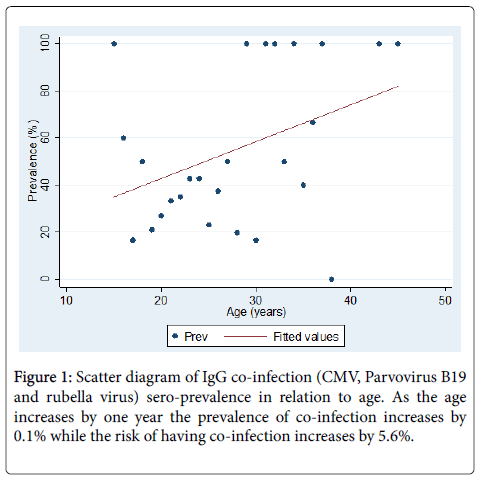
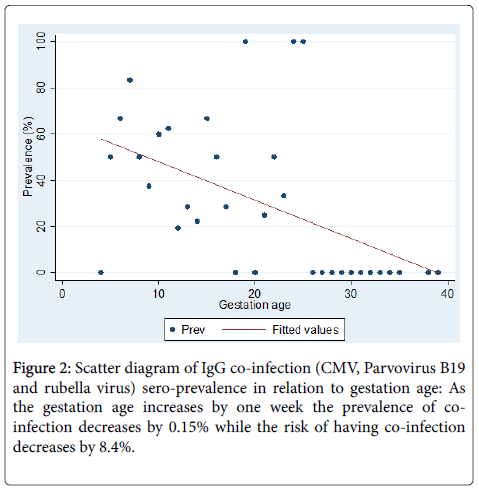
As the age increases the risk of co-infections significantly increases (OR: 1.056, 95%CI: 1.00 -1.11, P=0.03) (Figure 1). Moreover, as the gestational age increases the risk of getting co-infection decreases (OR: 0.923, 95% CI: 0.88 -0.96, P=0.001) (Figure 2).
Discussion
To the best of our knowledge this is the first report in Tanzania indicating the magnitude of viral co-infection with potential for congenital infection among pregnant women. The most important finding is the high proportion of past co-infections indicated by detection of IgG specific antibodies to all three viruses. This observation is supported by previous studies which showed high proportion of individual infection [8,12,18-21]. High level of natural immunity to these viruses indicates high transmission rates in this population necessitating the need for screen during antenatal visits.
The study found high proportions of acute co-infections of rubella and B19 indicating the potential risk of maternal to fetus transmission which might be associated with significant poor fetal outcome. The high prevalence of co-infections of rubella and parvovirus is supported by previous studies which also showed high proportions of acute infections of these viruses in developing countries [11,22,23].
In contrast to previous study in Africa prevalence of acute CMV infection was very low in the current study [21]. However, there is a need to investigate this further to explore the significance of multiple viral infections and severity of congenital anomalies. This also suggests endemicity in this area as evidenced by rubella IgG sero-prevalence observed by Mwambe et al. [12]. High prevalence rates are alarming considering the possible consequences.
Effect of seasonality and geographical distribution might also account for high reported proportions. This study was conducted during rainy season alternating with dry season which has been shown to influence viral transmission [24,25]. Further studies to investigate seasonal variations are highly recommended in this area.
As the age increases the prevalence of co-infection and individual infection also increases. Due to the fact that these infections are common during childhood; exposure during this time may explain such high proportions of natural immunity as previously described [8,26].
In contrast to individual infections [12,27,28], it was observed that as gestation age increases the risk of being co-infected decreases significantly. These results might have been influenced by CMV IgG sero-positivity because when individual infections were analyzed it is the only one which was found to be significantly associated with gestation age. This observation could not be explained or supported by previous studies. Therefore, further studies to investigate these aspects are highly recommended.
Limitation
The study was cross-sectional so participants were not followed especially for those found IgM positive to determine the outcome of the pregnancy. In addition ultrasound to detect fetal abnormalities was not performed. Failure to do PCR and avidity test to confirm the acute infection is another limitation of the study.
Conclusion
Significant proportion of pregnant women in Mwanza is infected with at least one virus and more than one third of these women have markers for previous co-infections of rubella, CMV and B19.
This calls for urgent need to screen these women during antenatal visits for proper counseling and advice on the potential of the outcomes that can be caused by these viruses during pregnancy.
Moreover, immunization of susceptible pregnant women to rubella virus infection after delivery will have more impact of controlling congenital rubella syndrome (CRS) in subsequent pregnancies. A follow up study to establish the outcome of pregnancy for IgM seropositive women is highly recommended.
Declaration
Authors declare to have no competing interest
Acknowledgement
The authors would like to acknowledge the technical support provided by Mr. Mkama, Mr. Vitus Silago, Ms. Carol, Mr. Benard Okamo, Ms. Maria Mwacha and Mrs. Damson. We thank all staff at KAMANGA Medics, Makongoro and Karume antenatal clinics. This study was supported by research grant from CUHAS to MMM.
References
- Wong A, Tan KH, Tee CS, Yeo GS (2000) Seroprevalence of cytomegalovirus, toxoplasma and parvovirus in pregnancy. Singapore Med J 41: 151-155.
- Odland JØ, Sergejeva IV, Ivaneev MD, Jensen IP, Stray-Pedersen B (2001) Seropositivity of cytomegalovirus, parvovirus and rubella in pregnant women and recurrent aborters in Leningrad County, Russia. ActaObstetGynecolScand 80: 1025-1029.
- Organization WH (2000) WHO position paper on rubella vaccines. Weekly epidemiological record 75: 161-172.
- Albanna EAE, El-latif RSA, Sharaf HA, Gohar MK, Ibrahim BM (2013) Diagnosis of congenital cytomegalovirus infection in high risk neonates. Mediterranean journal of hematology and infectious diseases 5: e2013049.
- Gratacós E, Torres PJ, Vidal J, AntolÃn E, Costa J, et al. (1995) The incidence of human parvovirus B19 infection during pregnancy and its impact on perinatal outcome. J Infect Dis 171: 1360-1363.
- Staras SA, Dollard SC, Radford KW, Flanders WD, Pass RF, et al. (2006) Seroprevalence of cytomegalovirus infection in the United States, 1988-1994. Clin Infect Dis 43: 1143-1151.
- Mustakangas P, Sarna S, Ammälä P, Muttilainen M, Koskela P, et al. (2000) Human cytomegalovirus seroprevalence in three socioeconomically different urban areas during the first trimester: a population-based cohort study. Int J Epidemiol 29: 587-591.
- Mirambo MM, Majigo M, Aboud S, Groß U, Mshana SE (2015) Serological makers of rubella infection in Africa in the pre vaccination era: a systematic review. BMC Res Notes 8: 716.
- Giorgio E, De Oronzo MA, Iozza I, Di Natale A, Cianci S, et al. (2010) Parvovirus B19 during pregnancy: a review. J Prenat Med 4: 63-66.
- Schoub B, Blackburn N, Johnson S, McAnerney J (1993) Primary and secondary infection with human parvovirus B19 in pregnant women in South Africa. South African medical journal 83: 505-506.
- Emiasegen SE, Nimzing L, Adoga MP, Ohagenyi AY, Lekan R (2011) Parvovirus B19 antibodies and correlates of infection in pregnant women attending an antenatal clinic in central Nigeria. MemInstOswaldo Cruz 106: 227-231.
- Mwambe B, Mirambo MM, Mshana SE, Massinde AN, Kidenya BR, et al. (2014) Sero-positivity rate of rubella and associated factors among pregnant women attending antenatal care in Mwanza, Tanzania. BMC Pregnancy Childbirth 14: 95.
- Taylor S, Yu D (2009) The importance of socio-economic status in determining educational achievement in South Africa. Unpublished working paper (Economics) Stellenbosch: Stellenbosch University.
- Souza VAUFd, Sumita LM, Otsubo MES, Takei K, Pannuti CS (1995) Enzyme linked immunosorbent assay for rubella antibodies: a simple method of antigen production. A preliminary report. Revista do Instituto de Medicina Tropical de São Paulo 37: 357-359
- Field PR, Ho DW, Cunningham AL (1988) Evaluation of rubella immune status by three commercial enzyme-linked immunosorbent assays. J ClinMicrobiol 26: 990-994.
- Chernesky M, Wyman L, Mahony J, Castriciano S, Unger J, et al. (1984) Clinical evaluation of the sensitivity and specificity of a commercially available enzyme immunoassay for detection of rubella virus-specific immunoglobulin M. Journal of clinical microbiology 20: 400-404.
- Schwarz TF, Jäger G, Gilch S (1997) Comparison of seven commercial tests for the detection of parvovirus B19-specific IgM. ZentralblBakteriol 285: 525-530.
- Rodier M, Berthonneau J, Bourgoin A, Giraudeau G, Agius G, et al. (1995) Seroprevalences of Toxoplasma, malaria, rubella, cytomegalovirus, HIV and treponemal infections among pregnant women in Cotonou, Republic of Benin. Actatropica 59: 271-277.
- Maksheed M, Pacsa AS, Essa SS, Ahmed MA, Monem RA, et al. (1999) The prevalence of antibody to human parvovirus B19 in pregnant women in Kuwait. Acta Trop 73: 225-229.
- Akinbami AA, Rabiu KA, Adewunmi AA, Wright KO, Dosunmu AO, et al. (2011) Seroprevalence of cytomegalovirus antibodies amongst normal pregnant women in Nigeria. Int J Womens Health 3: 423-428.
- Hamdan HZ, Abdelbagi IE, Nasser NM, Adam I (2011) Seroprevalence of cytomegalovirus and rubella among pregnant women in western Sudan. Virol J 8: 217.
- Grace P (2009) Serologic survey of specific rubella virus IgM in the sera of pregnant women in Makurdi, Benue State, Nigeria. African journal of reproductive health 13: 69-73.
- Keikha F, Miri-Moghaddam E, Sharifi-Mood B (2006) Prevalence of parvovirus B19 infection in successful and unsuccessful pregnancy in Zahedan, southeast of Iran. J Med Sci 6: 495-497.
- Harger JH, Adler SP, Koch WC, Harger GF (1998) Prospective evaluation of 618 pregnant women exposed to parvovirus B19: risks and symptoms. ObstetGynecol 91: 413-420.
- Hobman T, Chantler J. Rubella virus, 5th ed. Fields virology, Lippincott/The Williams & Wilkins Co, Philadelphia, PA; (2007).
- Junaid SA, Akpan KJ, Olabode AO (2011) Sero-survey of rubella IgM antibodies among children in Jos, Nigeria. Virol J 8: 244.
- Yeroh M, Aminu M, Musa B (2014) Seroprevalence of Cytomegalovirus Infection amongst Pregnant Women in Kaduna State, Nigeria. African Journal of Clinical and Experimental Microbiology 16: 37-44.
- Abiodun I, Opaleye OO, Ojurongbe O, Fagbami AH (2013) Seroprevalence of parvovirus B19 IgG and IgM antibodies among pregnant women in Oyo State, Nigeria. J Infect DevCtries 7: 946-950.
Citation: Mirambo MM, Chibwe E, Mushi MF, Majigo M, Mshana SE (2016) Cytomegalovirus, Parvovirus B19 and Rubella Co-infection among Pregnant Women Attending Antenatal Clinics in Mwanza City: The Need to be considered in Tanzanian Antenatal Care Package. Epidemiology (Sunnyvale) 6:230. DOI: 10.4172/2161-1165.1000230
Copyright: © 2016 Mirambo MM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 12703
- [From(publication date): 4-2016 - Aug 30, 2025]
- Breakdown by view type
- HTML page views: 11692
- PDF downloads: 1011