Dementia Part One: A Physical Treatment of Individuals with Dementia
Received: 10-Nov-2018 / Accepted Date: 20-Nov-2018 / Published Date: 30-Nov-2018
Abstract
A very difficult item because physical treatment for elderly is still a “lesser” form of physical therapy and a treatment for elderly with dementia is almost “not done”. But out investigation all over the world, it is clear, that movement and especially aerobe exercises have a better effect on slowing down this disease than other approaches including medical treatment. This part about dementia will discussed these investigations and their conclusion and the translation to the practice. And the first problem is very fast present, because most investigation is only done with mobile individuals with dementia and not with individuals that are not so mobile anymore. That means: “That the greatest problem isn’t properly investigated and that makes things complicated”. People with dementia have a restriction in the capacity, what their brain can copy with. Is that problem “Movement”, than are there an lot of possibilities, but exercising/ training ask for an activity close to the border of the possibilities and that can be difficult by this group. The fear for failing is very strong and has a great negative effect, where this people are very sensitive for and can make exercising almost impossible. Another problem is environment, the care givers/family but also other professionals. They often react from their own perspective and search for an solution, that make it work for themselves easier but the independency of the individual with dementia will often fast decrease. The environment can also be an inhibition for movement and that we see often in residences/nursing home and even in their own home, that the possibilities are not optimal to move independent with their own speed. In this part the emphasis lies on what we know about the sciences and how to translate this for the individual with dementia to hold his own possibilities. Further one we start with an assessment, to get an picture, where the difficulties lies and that is often still possible at the beginning of the disease. When the disease is progressing this will far more difficult but with the knowledge of the start, we have a cardinal point. To have a “railway guide” in developmental of this degenerative disease we start with the introduction of the “Rakt-scheme” to focus on the main problems of the people with dementia in the diver’s moments of this disease.
Keywords: Dementia; Physical therapy; Environment influences; Rakt-scheme
Introduction
This disease is most inhuman disease that exists. There are a lot of disabilities but losing you human- ship is the most devastating disease. You lose as an older person not only your body but also your mind. You are not able to communicate and recognized the people you love the most and with you have done everything in your live. And the family has the same experience, losing an important person without the possibility to be there and give support that this person experienced. There is now a movement in progress that try to help this people suffering from this disease and their love-ones, but long it was a problem for this group and the assistance was minimal.
Growing old, is still this day an starting with saying goodbye to all good things of live and the culture that belong with this attitude is still present.
There are all kinds of action to change that, but there is still a great gap between the care for individuals with dementia and older people that are present in the streets and shops. This disease isn’t curable and it will not be curable for a long period, but there are signs that the disease can be slowing down by medicine but especially by movement. And human movement is the working area where physical therapist is trained for. But it was a long time not well understands that therapy must have a certain level, will it be effective. That part is by the science discovered centuries ago but the physical therapy by people with dementia was still moving on a too low base, strange! Strange? Yes, because in the education of the physical therapist, it was clear what has to be done and how, to get progression of the body through movement. Till today often the exercises are so low of intensity that it is no exercise that will have result. And that means that therapist is not preparing to train but makes movements with this group of individuals and don’t believe that this can have results.
That concept
Training must have results - means that it is your job to get on the border and on the right level.
Is this fear for or is it an culture, that old and certainly individuals with dementia must not be trained on an right level or is the interest in this people too little to do what is necessary?
Rakt-Scheme
This Rakt-scheme is developed in the middle of the year 90 of the last century and it was mending to be a scheme to train people with dementia with their movement problems in the difference stages of the diseases and is practiced in Nursing Home in the Netherlands. This scheme is no rigid system but is changing and that changing occur the last 10 years rapidly because the borders of intensity of movement where changing by science. That means that the possibilities to move with all kinds of new things were increasing. But regrettably, a lot of that apparatus where difficult to obtain for nursing home citizens because there was no money for.
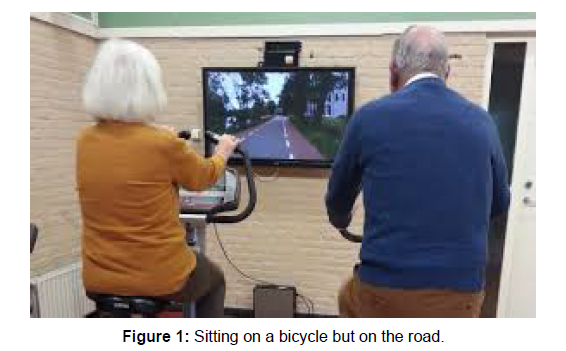
An example, bicycle is very good aerobe [1-3] exercise that can help to train the cardio vascular system but only sitting on a bicycle is boring but when there is a screen on which she travels through their own village, is much more nicer and stimulated. Another aspect is that people must be become tired. Older people have heart the whole live that older people must not anymore work so hard because that isn’t good.
We know now that the opposite is true, not moving will change the body rapidly and weaken it. Knowing, that exercise is very important but how can I get someone with the “wrong” exercise attitude so far that he go sitting on an bicycle and make an lot of kilometres with resistance that he is at the end tired and had need of an good rest period. And will he come back the next time and can I as therapist, change the situation in his house or on the ward that he will do more there also. And be honest what will the other members of the family say with this approach, when he tell that he must drive on an bicycle all away through “Amsterdam” !! Through the connection with the bicycle they are capable to ride through the city and can have a goal where they are want to go. That means so many kilometres and in a certain time! And Amsterdam has a lot of bridges! (Figure 1) But is this enough to hold the body in shape and also the mind?
The investigations of the scientist all over the world are still searching but there is now more clarity what the intensity must be. Erickson [4] has investigated this by older people without dementia and he makes MRI –pictures of the brain and especially from the hippocampus. A system that is important for our short/work memory. He makes these pictures after 6 months and after a year.
He divided the participants in two groups:
A. Group one has one per week walking exercise starting with 5 minutes, but increasing to 40 minutes. The heart rate was week one 50-60% of the heart bates maximum and after a week 7 was this 60-75% and that means that the intensity was increased not only by the time but also in speed.
B. Group two did in this time stretch- and resistance exercises that also was increase in heaviness. This exercise where done in a sitting position and with apparatus.
The blue line is the chance that occur in the size of the hippocampus at 6 months and after one year for group one! The red line is the chance that occur in the size of the hippocampus at 6 months and after one year for group two (Figure 2). The conclusion was that aerobe walking exercise with increasing intensity has changes the size of the hippocampus about 2% and that means that here is evident that walking with increasing intensity has a positive effect on the size of the hippocampus and therefore it is an approach that break the regular loss of the hippocampus.
Group 2, who did exercise to get more strength and stretch exercise let see that at 6 months and after an year the loss of the hippocampus was the same as normal. 1-2% size loss of hippocampus per year is the comment loss that occurs by all older people, but walking with an intensity level can change this loss and the first year even change that loss in a growth.
The loss of the hippocampus in group one will occur, but start with a greater hippocampus and maybe the loss is slower. From this investigation (among others) is one of the important effects from exercises that this has an effect on the brain and that there is a rule to get this done! This therapy is possible in the first stage of the disease when individuals are capable to walking with so much speed but not by the group that is living in a nursing home or at home or that level. The disease has been worse and these possibilities are not anymore present, but the rule stays. One of the main problems that individual with dementia experience is the loss of the balance and then it is dangerous to walk without an aid and walking outside is difficult and dangerous according a lot of people and often is the family the first one. This group of people will be treated by physical therapist to get the level as high as possible and that ask for a good assessment. An assessment that search why the balance is lesser and where there are possibilities to get this on a higher level. Here we have the first problem in our society, because often there is no assessment and is the first action that this individual will be given a rollator frame and maybe their home is changed with more aids, a stair elevator and removal of all carpets.
Will this Change the Possibilities Regarding the Balance?
There are strong indications that walking with support as a rollator frame [5] will lead to a decrease of balance capacity. An investigation, that in this field has investigated what happen when individual with dementia in Nursing homes get to walk with an rollator frame instead of another aid or no aid as walking with support of furniture of from the railing. Before the rollator frame was used this people were capable to do the one leg standing test [6] with the eyes open for more than 15-30 sec. on both legs. After 3 months this test was repeated and the capacity to stand on one leg was dramatic decreased and a very rear item was that the movement to stand on one leg was changed and that this people were afraid to go with the hip/trunk sideways over the foot to lift the other leg. We have rehearsed this investigation, because we want to know what the reason was that so many individuals make not the proper sideways movement and therefore were not capable to lift the other leg and cannot do the one leg standing test.
- Is this because the body perception is changes and is that by individuals with dementia faster than with older without dementia.
- Or is it the muscle power, so fast decreased that there not enough power to hold the pelvis stable.
- Or maybe it is a combination of these two elements.
We created a situation in which the individual was complete secure, but we ask them to stand near the chair with a distance that wasn’t enough to lift the other leg on the right way (Figure 3). They were permitted to get their hand on the support of the chair, but the investigator laid his finger under hand to stimulate that they will support only little on it. All individuals with perception-loss stand with the pelvis against the back support of the chair and where therefore not capable to lift the other leg without making a trunk movement upper trunk sideways (Duchene). We did the same test also by all individuals that walk with a rollator frame, with or without dementia and walk and support on this frame for more than 3 months. And the first attempts were exactly the same, she also stand too close to the back support of the chair and make therefore a trunk movement with upper trunk. That movement is done by individuals that have pain on their hip and a Duchene- movement lower the pressure on that joint.
But there was a difference between the two groups. The group rollator frame walkers with and without dementia. The group with dementia stay with their movement and couldn’t make any change on their one. With assistance, they dare to try with more distance to the chair and someone succeed.
In the group without dementia almost everyone did change with assistance the position of the distance to the back support and make a one leg standing with a lower trunk sideways. Only the individuals that have insufficient muscle power in the abductors were not capable to do this that was all individuals after hip surgery.
We test than the power of the abductors of all people and there was a decrease in muscle power but not enough that this was the reason that one leg standing wasn’t possible.
Conclusion of this investigation was:
- Walking with a rollator frame changes the perception [7] of the body, especially the sideways movement of the hip over the foot, the distance that is necessary, to move the other leg to the front. The support on the rollator frame makes it not necessary to makes this movement because the hand is controlling this movement and in the lower trunk and hip is no movement sideways necessary. The perception from the individuals with dementia is obvious also changed but there is no recollection how it shout be and that means that it is very difficult to get that back – Within 3 months supporting on an rollator frame !!
- The muscle power of the individuals with and without dementia seems to be faster decreasing through the walking with support on the rollator frame. Obviously the support on the rollator frame gives another diagonal system and asks almost nothing from the homolateral structure (see articles about diagonals [8t/m15]0. And muscle that performs badly or less, that has also an influence on the perception through the muscle spindle. But also will the muscle lose power, first more fast muscle fibres will decrease and replaced for slow muscle of fat. That will have an effect on the perception and the power [8].
Therefore we search in the literature, what is known about perception and dementia. Little is investigated in this area, very little and there is no guideline about this subject. Muscle strengthening is an item that in all exercise programs is mentioned, when the balance is decreasing and that strengthening must be task specific with load. But, realized that the effect on the cognitive aspect of this disease through strengthening exercise is according Erickson and manty others isn’t present. It has only an effect on balance!
Rakt-Scheme Phase 4
The greatest amount of investigation is the group that in the Raktscheme are in phase 4. This is people that are capable to walk with or without an aid/rollator frame and are often still at home. The greatest problems occur on ADL area. Walking outdoor is still possible, only when there are much open planes, distraction, difficulties on the pad or an combination of all this things, it is become difficult and will the speed slowing down. ADL according Dr. A.v.d. Plaats [9] ask so much of our brain, that is this is a high cortical /subcortical action that will be loss very soon in the process of dementia [1].
Orientation, especially outside and on places that are not familiar is very difficult, but also familiar surroundings can disappear very suddenly. Beautiful performed in the film “Still Alice” [10] and investigated by Prof. O’Keefe and Prof. Moser [11]. They prove in 2014 (Nobel Price) that the “G.P.S. “can suddenly stop and that the individual isn’t capable to know where he is, but also not capable to find a solution. Often we see the first problems with walking outdoor and doing double task and that makes walking in a strange and difficult environment very difficult and ask very much from this individuals.
An test with an group of dementia individual in the States in the last century show that walking in an forest was for this group easier than walking in an grassland. The condition of the “floor” wasn’t identical but the trees gave a better “border” system and make it easy for the individual with dementia to feel secure and the possibility to touch a tree stimulated that security [12,13]. In spring time this group will want to walk outdoor, but when the entrée of the house or institution is far open than often this people hesitate to go further because the control of the border is gone. We see this also on the ward, walking through the corridor isn’t an great problem, often they walk in the middle of the corridor but when the corridor end and the comes an greater room, this people stops and search for an support before the go further and then often along the furniture. All kinds of signs such as high cognitive functions are decreasing as memory, attention, praxia, gnosis [14] and speech tec. All this problems are signs, that the brain has problems to hold his level. Because of the uncertainty, people were afraid and depressed, but the capacity that they have to cope with this situation is also decreasing and there we see a change in behaviour but also in tone of the body. This change in behaviour vary from agitation till apathy, but the reaction on an situation is always in our eyes extreme and from an therapeutic view we see that often the tone of the muscle increased and sometimes is that tone so high that walking and moving isn’t possible anymore.
Walking inside with no aid can change outside in an attitude in which he is so rigid that he cannot walk further or he squeeze in the arm of his assistance and want to go back inside. That are signs that the system has an too heavy burden to carry and that is called capacity. This is for all aspect true, therefore also for the possibility to move and to exercise. But to exercises on the right level par example balance, there must be a change, because otherwise this stimulus has no value. That’s complete correct, but by people with dementia, we must create the circumstances and the sphere so positive as possible and that means often an individual exercise in which the individual with dementia feels that he “wins” from the much younger therapist. This aspect is very important and is often not there in a group session. Often the laughing [15] is present but in a group the weakest member determined the level of exercises. Group therapy is very good movement moment but no exercise.
Therapeutic
The individuals with this phase of dementia will live often still at home and will be able to walk in home on the one, but there are some problems with the body and that is almost always balance. Balance improvement is possible by exercising balance and task specific resistance treatment from the important muscle pattern that is needed to get in balance and be able to restore balance. But a good assessment is very important because we must know;
- What is the perception of the whole body and from the legs and feet especially [16]?
- What is the power of the muscle pattern and are they complete.
- Are there signs that the alignment makes it difficult to move in the right way. Think of lumbar stenosis²ᶣ that will change the lumbar spine from extension to flexion and will force the individual in an attitude in which he will bend more in the hips and lower trunk. Or is there illness that changes the nerves on another way – diabetes or restrictions in the joints can also give a problem by a good balance reaction.
Perception
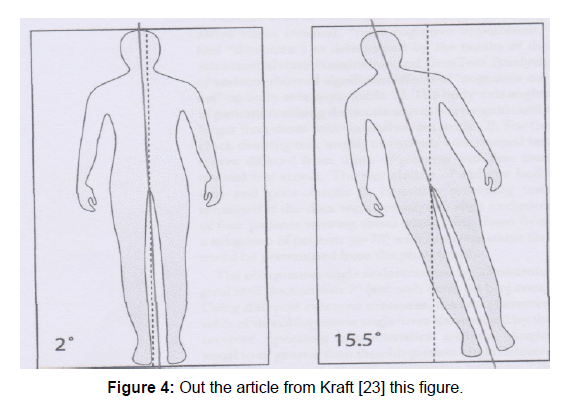
There is growing evidence that dementia will changes the perception of the whole body. In 2009 Kraft [17] and others published an article: “Lying obliquely “– a clinical sign of cognitive impairment. This oblique lying was typical for people with cognitive impairment and after reading this article all the individuals (35 persons) we have testing on this sign. Nobody of that group lay in the mid of the bench. Other individuals with a lot of problems but no cognitive one, were still lie in the mid of the bench.
From the individual in the phase 4 (Rakt-scheme) group only 2 were capable after the investigators have addressed them that they are lying oblique and not in the middle to correct that only when:
1. The bench stood with one side to the wall.
2. The may use the eyes to correct there attitude.
Out the article from Kraft [17] these in Figure 4. And that gives a picture of the great different of the oblique lying. Starting by 2° as normal was the different degrees by cognitive impairment by someone fast 15- 16°. But what has this for implications for the balance in standing position?
Figure 4: Out the article from Kraft [23] this figure.
There are no investigations that has investigated or that degree of oblique lying also occur in sitting and standing position. What we well know is that people that change the body position [18]. When they had back pain over an longer period (more than 3 months). Than this attitude is getting “normal” and only by seeing in the mirror, this individuals witness that they walks with more flexion in his hip and trunk as they suspected. We know that the individual with an stroke (pusher syndrome) also feel that he stand in an erect position, but the reality shows that they push to the affected side with the not-affected side too far out the midline and in severe cases they will fall to the affected side.
Further one there are also signs that the body perception can change by altering of your attitude but by individuals with dementia this changes can also be done through the damaged brain? Balance requires good information about the weight-bearing through the feet. Too much to the back must give immediately a muscular reaction even before the brain can think that someone is falling. That means that the everyone must be able to feel the movement under his feet.
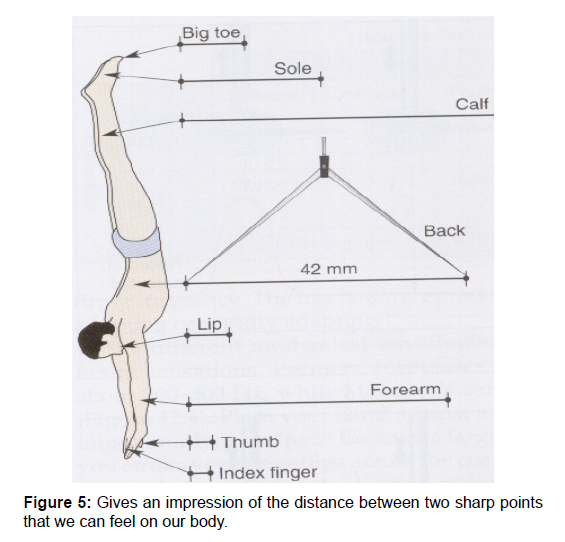
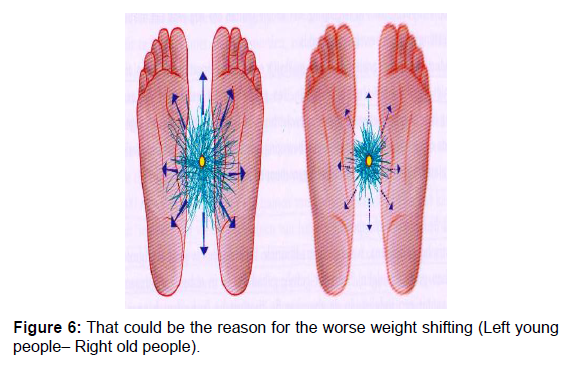
Discrimination sense
In this phase of dementia is testing often possible, therefore it is very important because when this is disturbed that will have consequences for the possibilities to change the balance and walking capacities and not right feeling of movement under the feet will also give an sign that the capacity of the brain is lesser than we taught [19]. The best performance we achieve with the thumb, index finger and the lips and the worse performance with our back. Under the feet this distance is about 35 mm and we have this tested by the phase 4 group and older without dementia (Figures 5 and 6). By both groups there is a decrease of two point discrimination sense and especially the heel are by older people less sensible that the other area of the foot sole. But the individuals with dementia were not so good, comparing with the other group. And that can have many consequences! When the distance is greater that the foot is wide, than will this mean that movement under the foot in medial and especially lateral direction isn’t feel anymore. The next test is testing the gnostic sense and now was the group with dementia far more badly than the older of the same age. This difference was very great and has very much surprise us.
Gnostic sense
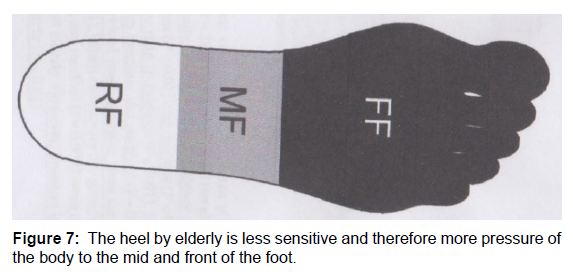
Testing with a tuning fork with a low frequency 64 or 125 hertz [14]. The first testing performance was very difficult because the individuals with dementia were not capable to give a difference when we apply the tuning fork against the bone parts of the foot, ankle or knee. The other group (elderly without dementia) were capable to feel the difference and it was obvious that the tuning fork was felt the better in the malleolus and lesser in the bone of the heel. The hallux was often felt well by this group. We try it with hot and cold and in between and again the differences were for individual with dementia very difficult and only true cold and true hot was recognised and then there was also the good reaction. In between was it difficult. But there was another strange thing, often there was no reaction in the face by the individuals with dementia when the fork was on hallux, heel and was the first reaction when the fork was placed against the malleolus. This reaction was often: Removing the towel before their eyes and search for reason what there was happening.
It seems that the foot was not “felt” through the fork, because no or very little reaction occur when we touch bone part of the foot sole, heel or hallux joint and the first reaction often occur at or above ankle level.
We therefore change the test and starting with the jaw bone. To see what the reaction was. This reaction was great; all individuals move away and look with great eyes to us. That was a strange feeling and then we test the legs again and often again the reaction was only giving when we were at ankle level, no reaction when the fork was placed on the bone part of the foot. And they often expressed that this was nothing, comparing with the fork on the jaw bone. This difference was also there by the other group but this difference wasn’t so big and this entire group felt also the foot sole, heel and hallux bone. But the heel part was the part with the lowest sensation by all older people with and without dementia. Article: “Differences in foot sensitivity and plantar pressure between healthy young and elderly [14] 2015. The heel by elderly is less sensitive and therefore more pressure of the body to the mid and front of the foot (Figure 7).
Gnostic sense disturbances mean that the possibility to control the surface on his quality isn’t possible with the feet. The eyes say that it can be slippery but the individual isn’t capable to control that and that will lead to a different walking pattern. Scuffle is the best way to copy with a surface that is slippery and give the less change of falling.
When there are also problems in the nerves at the end and in the transport to the brain, these symptoms will be having an influence on the brain. The perception will change and the muscle pattern will be changes and adapt.
But not only will the muscle pattern change also the brain will adapt and that brain is lesser through the disease. That will have also a reaction on their behaviour, fear etc. Some will go to an inactive modus and walk only, when it is necessary and with great caution, others will doing the opposite and that we see back in the developmental of the power of the muscle pattern. That means, that loss of perception can lead to an decrease of muscle power and that has an negative influence on the balance. And that can only be change or slowing down by giving muscle strengthens exercises. Not only the centre for memory and language are damaged but also the cortical areas where lies the somato-sensor cortex and the motor cortex of the whole body. The cortical control is therefore also lesser (Figure 8). That means that the perception in the brain is changing, but also the possibilities of the motoric system. The selectivity is changing and decreasing and we see “paratonia”. According to Dr. H. Hobbelen [20] are the individuals with dementia, who have in this phase symptoms of paratonia and that is when the arm or leg are passive move faster as the speed of the MAS [21] (As worth) (MAS-P [22]). Tonus that is alter, will have an great influence on the balance and the balance reactions because when the possibilities to react with speed is decreasing than also the possibilities to make the right movement get lesser. And of course the possibilities to get a higher level by exercising are more difficult, because this centre is damaged. The only possibility is task- specific resistance treatment because that has an effect on the power of the muscle (power=Speed × strength) but also on the coordination and coordination is by tone increasing very important.
Muscle strengthening
To get a better treatment to slowing down that balance problems this treatment is necessary but will this treatment give an effect on the cognition. According the investigation of Prof. Erickson [4] was only the aerobe group capable to increase the cognition by growing the hippocampus and when power treatment is necessary has that only a benefit for the balance and can increase the possibilities of the individual with dementia to move in his own house. This question is investigated by a lot of scientist, but two of them we will discuss here.
- In 2015-2016 two articles were published in which this question was investigated
A. A 9-week aerobic and strength training program improves cognitive and motor function in patients with dementia (RCT) from W. Bossers [2] and co.
B. The effect of physical activity on cognitive function in patients with dementia: A Meta - analysis of randomized control trials from C. Groot and co [3]. Important because here the aerobe training was done by individuals with dementia.
- Another investigation from 2015 : Long –term effects of an 12 weeks high- intensity functional exercise program on physical function and mental health in nursing home residents; an single blind randomized controlled trial from E. Telenius [23] and co. give an picture that exercising with an high intensity (heavy load) but functional ( that means walking, standing up, make squats etc. has an effect on both and in this program the R.M. was so high as possible and was the number of rehearsal therefore minimal. In this program there was a very strong muscle training part but also a strong aerobe part and both give an increase from the balance and show effects on mental health especially on agitation and apathy.
Both the investigation confirms that the aerobe part of the training is very important and that this part will be has the greatest effects on the cognition. But resistance treatment with an aerobe component as in the second investigation (the HIFE- High Intensity Functional Exerciseprogram) will be lead to a combination of effects.
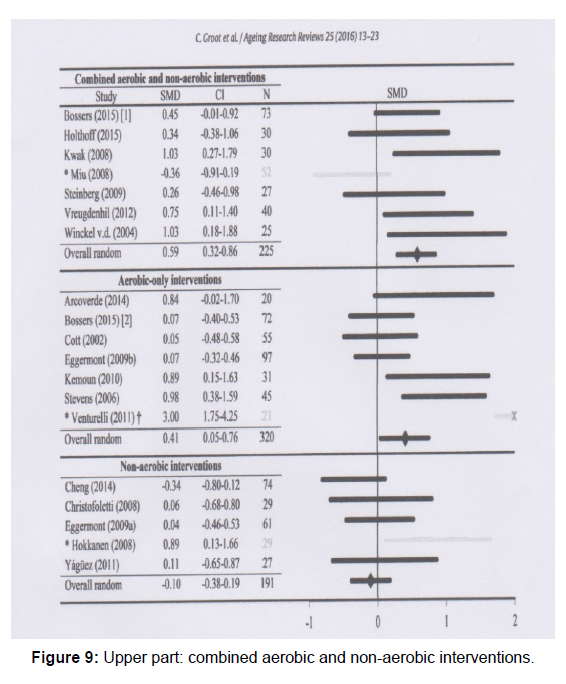
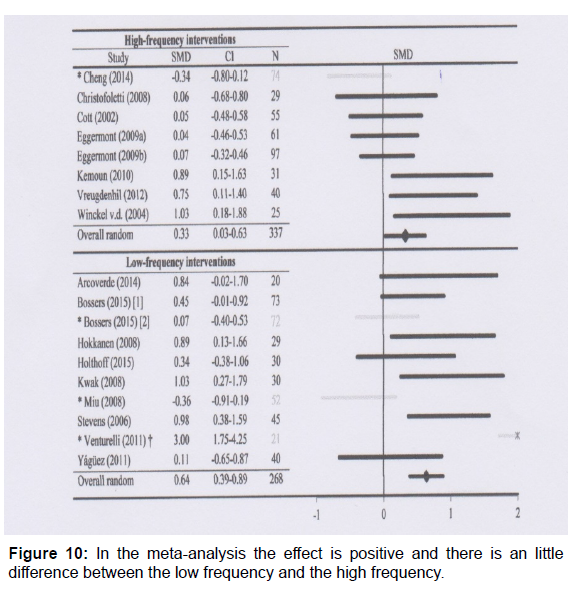
From the first investigation (the meta-analysis B) came this outcome: Another element that was investigated in this meta- analysis was (1B); How often must this therapy be given? Frequency and the RCT that where included the lowest frequency was 2 times a week for 40 minutes. Upper part: A combined aerobic and non-aerobic interventions (muscle strengthening) the effect on the cognition was clear. Middle part: an aerobic –only intervention the effect was clear only a little bit lesser than the intervention with strengthening (Figure 9). Lower part: Non-aerobic interventions, this where not only strengthening exercises with an often modest intensity, but the reaction on the cognition is very clear. In the meta-analysis [3] the effect is positive and there is an little difference between the low frequency and the high frequency. The low frequency scores even better than the high frequency!! The lowest frequency that was done in the included investigation was 2 times an week for 40 minutes (Figure 10). Therefore this meta-analysis cannot give another solution than that 2 times an week is more than sufficient to get the results (Tables 1-5).
| Independent | Supervision | Assistance/ facilitation | Not possible | Clinometric | |
|---|---|---|---|---|---|
| Which attitudes are possible in lying position? | |||||
| Supine | X | ||||
| Lie on the affected side Left/Right | X | ||||
| Lie on the not-affected side | X | ||||
| Left /Right | |||||
| Can the patient move in lying position. | |||||
| Sideway on the back left. | X | ||||
| …………………………….right | X | ||||
| ………………………Up in bed | X | ||||
| ………………..down in bed | X | ||||
| In side lying (the affected side or left /Right) move back or to the front | X | ||||
| The same on the other side | X | ||||
| Turn from supine to the affected side | X | ■ 25 | |||
| Left/ Right | |||||
| T.C.T.= 0/12/25 | |||||
| Turn from supine to the not- affected side Left/ Right | X | ■25 | |||
| T.C.T. = 0/12/25 | |||||
| From supine to long sit | X | ||||
| From side lying to sit on the edge of the bed –affected side Left/Right T.C.T. = 0/12/25 | X | ■ 12 | |||
| From side lying to sit on the edge of the bed not -affected side Left/Right T.C.T. = 0/12/25 | X | ■ 25 | |||
| Sit ; which attitudes are possible | |||||
| Sit in an wheelchair | X | ||||
| Sit on the edge of the bed. | X | ■25 | |||
| T.C.T. = 0/12/25 BBS 3 = 0 t/m 4 | ■ 4 |
■ Measurement moment
Table 1: What can the patient = Activity possibilities.
| Independent | Supervision | Assistance/ facilitation | Not possible | Clinometric | |
|---|---|---|---|---|---|
| Transfer from and back to the bed. Over the not-affected side Left/Right BBS 5 = 1 t/m 4 | X | ■ 3 | |||
| Transfer from and back to the bed. Over the affected side Right/Left BBS 5 = 1 t/m 4 | X | ■ | |||
| Possibilities to stand up | |||||
| Standing up from an chair or wheelchair BBS 1 = 1 t/m 4 | X | ■ 3 | |||
| Sitting down in an chair or wheelchair BBS 4 = 1 t/m 4 | X | ■ 3 | |||
| Move in sit; transfer the chair in sitting position to or from the table. | X | ||||
| Possibilities to hold standing position. | |||||
| Standing Position BBS 6 (eyes closed = 1t/m 4) BBS 8 (reach = 1 t/m 4) | X | ■ 1 | |||
| Capable to place an foot Back, side front left and right | X | ||||
| Standing with closed feet BBS 7 = 1 t/m 4 | X | ■ 3 | |||
| Bend and pick up an shoe BBS 9 = 1 t/m 4 | X | ■ 2 | |||
| Look back in standing position BBS 10 = 1 t/m 4 | X | ■ 2 | |||
| In standing position turn 360ᵒ Left and right BBS 11 = 1 t/m 4 | X | ■ 2 | |||
Table 2: What can the patient = Activity possibilities.
| Possibilities to walk | Independent | Supervision | Assistance/ Facilitation | Not possible | Clinometric |
|---|---|---|---|---|---|
| Walk in house. FAC = 0 t/m 5 Barthel H = 0 t/m 3 | X | ■ | |||
| Walk and answer question the same time. Double tasks SWWT | X | ■ | |||
| Walk outdoor. | X | ||||
| Walk speed. 10 meter Walking test | X | ■ 14 sec | |||
| Standing position with one foot for the other. BBS 13 = 1 t/m 4 |
X | ■ 2 | |||
| One leg standing. BBS 14 = 1 t/m 4 One leg standing time / eyes. |
X | ■ 2 | |||
| Walk distance | 100 m | ||||
| Walk aids | |||||
| Different substrate sidewalk, oblique. Etc.) | X | ||||
| Possibilities to walk on the stair. | |||||
| Placing the foot on the first step of the stair and with changing legs. BBS 12= 1 t/m 4 | X | ■ 1 | |||
| Up the stair. Barthel J = 0 t/m 3 | X | ■ | |||
| Down the stair. Barthel J = 0 t/m 3 | X | ■ | |||
| The patient is capable to take something with him and going up and down the stair. | X |
Table 3: What can the patient = Activity possibilities.
| What are the possibilities of his arm / hand? | Independent | Supervision | Assistance/ Facilitation | Not possible | Clinometric |
|---|---|---|---|---|---|
| The patient has attention for his affected arm/hand. | X | ||||
| Capable to nurse his arm / hand. | X | ||||
| He is capable to move his arm spontaneously and arbitrary. | X | ||||
| Abduction of the shoulder from 0ᵒ to 90 ᵒ | X | ■ | |||
| M.I. (Arm) = 0 t/m 33 | |||||
| Flexion elbow, complete flexion elbow. | X | ■ | |||
| M.I.(arm) = 0 t/m 33 | |||||
| He is capable to move his hand spontaneously and arbitrary. | X | ||||
| Capable to use the arm /hand as support. | |||||
| Support forward | X | ||||
| …..side way | X | ||||
| ……. Back ward | X | ||||
| The patient can hold something in his hand. | |||||
| An orange or an tennis ball. | X | ||||
| an banana (cylinder grip about 3 cm.) | X | ||||
| an glass and drink. | X | ||||
| An tweezers grip (pincer) | X | ■ | |||
| M.I.(arm) = 0 t/m 33 | |||||
| The patient is capable to manoeuver something in his hand. | X | ||||
| Wash and dry his hand with towel. | X |
Table 4: What can the patient = Activity possibilities.
| Independent | Supervision | Assistance/ Facilitation | Not possible | Clinometric | |
|---|---|---|---|---|---|
| Wash | X | X | |||
| Dry | X | X | |||
| Dress on | X | ■ | |||
| Barthel i = 0 t/m 2 | |||||
| Un dress | X | X | |||
| Make up etc. | ■ | ||||
| Barthel c = 0-1 | |||||
| Going to the bathroom Barthel d = 0 t/m 2 | X | ■ | |||
| Moving over long distances? | X | ||||
| Walking | X | ||||
| With the wheelchair | |||||
| Bicycle | |||||
| What are the possibilities with his head? | |||||
| Rotation to left and right. | X | ||||
| Lateroflexion to left and right. | X | ||||
| Tongue movements | X | ||||
| Slallowingᶣ² | X | ||||
| Eat and drink | X | ■ | |||
| Barthel F = 0 t/m 2 |
Table 5: What can the patient = Activity possibilities.
That gives the following picture:
The other investigation (B) had a program with high intensity and functional exercises. The effects were there on the balance and also on cognition. Not all aspect of cognition was significant but well clinic relevant.
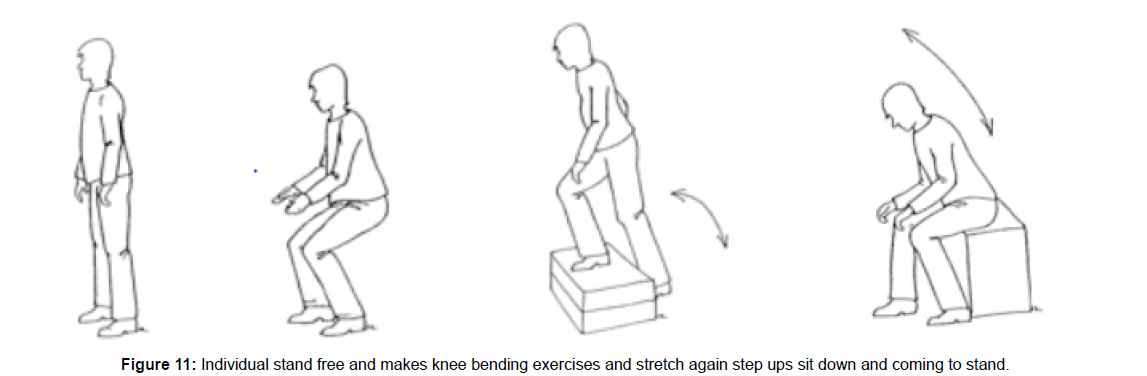
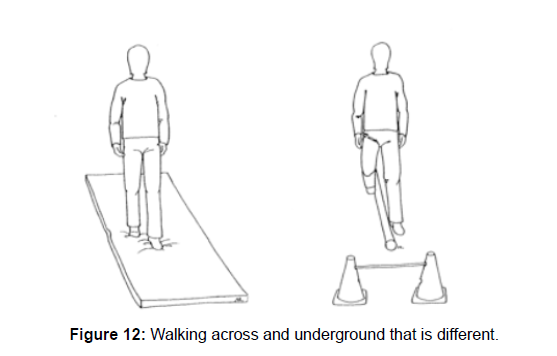
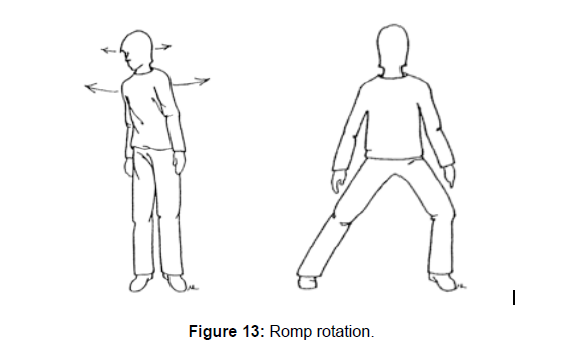
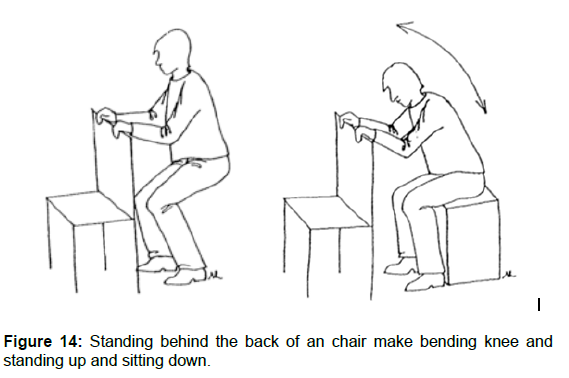
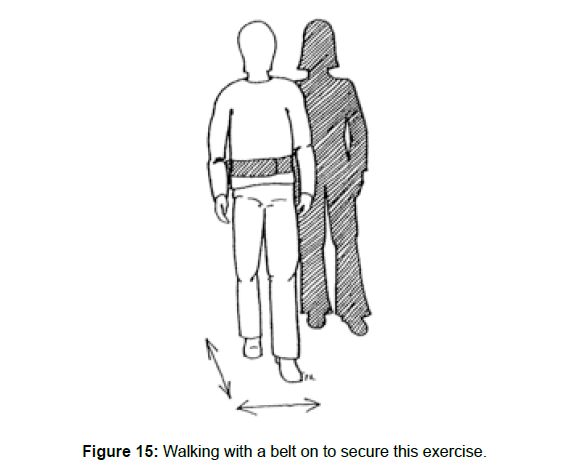
This program (HIFE [24]) has exercises that cover 5 items Individual stand free and makes knee bending exercises and stretch again step ups sit down and coming to stand In this case a mat as the instable underground. Walking and stepping over something on the floor or take and high step. And weight shifting from one leg to the other with a broad base. Standing behind the back of a chair make bending knee and standing up and sitting down (Figures 11-15).
1. Static and dynamic balance exercises in combination with strengthening exercises.
2. Dynamic balance exercises when the individual is walking.
3. Static and dynamic balance exercises in a standing position.
4. Strengthening exercises with a support for the balance.
5. Walking in different directions but with balance support.
Intensity
There were three levels of intensity:
A. High: 8-12 rehearsal of 1 R.M. This with the control of the attitude complete for the individual, no support.
B. Moderate: 13-15 rehearsal of 1 R.M. The postural control isn’t complete necessary. 2-3 times rehearsal of these exercises in one session.
C. Light: More than 15 rehearsal of 1 R.M. And a postural control isn’t necessary.
Problem with this program (HIFE) is that the intensity isn’t clear. 1 R.M. means that someone can do this 1 time and need therefore all his strength. A second time isn’t the same as the first time. From there we have 100% (1 R.M.) and we start often with 75% and then the number of rehearsal is 10 times and that 3 times on that session. And that 2-3 times a week. When the R.M. is lowering to 50% (moderate) or by light, lower than 50%, and ask that for an increasing of the number of rehearsals and the number of session and frequency through the week must be more. Even by moderate is 2-3 rehearsal pro session for strengthening to low.
The other problem is that it isn’t clear, what the intensity is for the aerobic part is of the exercises. There is through this program clear a lot of aerobic training but the intensity isn’t clear. There are no hart –rate frequency assessment par example what give an indication what the aerobe intensity must be.
This problem exist also in the article that where included in the meta-analysis. Often isn’t obvious what was ask of the individuals with dementia and what the control group did an exercises. But both programs give a very clear answer what is important to have a lowering effect on the decrease van cognition. Strengthening has an effect on muscles and not directly on cognition. Improving or holding the balance possibilities ask for a strengthening program and there it is important how this is the best achieve. Task-specific with resistance or load.
The group of individual that can do these programs is limited. That are the people that can walk and need no of little support, but when the walking problems increase that ask this an great amount of creativity and persuasion to get this people so far, to this program. That makes that the program is often against the border of the capacity and that will inhibit much individuals to active participated. That means that the effect on cognition will be possible in the individuals in this phase and that the group that cannot participated this “medicine” (aerobic exercises to improve or slowing down the cognition) cannot participated and we must search for other programs.
Another problem is: “When to start”? We all want to stay independent so long as possible and “strange” people, we hold out our houses. When there are problems, than every therapist will know how difficult it is, to change something in the home and exercises by this people at home. This at home exercising is important, but also must there be always the possibility to be part of an group and exercising outdoor to hold the social contacts. In the spring of 2005 the Nursing home starting a daily program for people with dementia to give the family caregivers more space and air on that day. The doctor had found no physical problems, therefore therapy wasn’t necessary, that was also the opinion of the doctor at home. From the 35 individuals that where invited at this program, 33 walk with a rollator frame and the remaining two walk with a cane outdoor. This is also an cultural problem, walking with an rollator frame is “normal “for old people especially when they have dementia but is isn’t normal. The assessment that was done by this people was very poor;
- No investigation about the perception
- No investigation of the tone, selectivity and power
- No investigation about the balance, no clinometric as an B.B.S.( Berg Balance Scale [24])
- No investigation about the alignment
They only rapport was an description, what the individual had on intern, neurologic and orthopaedic complaints in his live, with as last one; “Dementia”.
How convince the doctor that this people can more and that this isn’t the border of their capacity. That this must be used to slowing down the loss of cognition and also that walking with a rollator frame is a sign, that the balance is lesser and that there are possibilities to treat that. The moment that individuals hear that they have dementia, should be the moment that the program start to slowing down this process. That will be done with medicine but aerobic exercises should be part of it. Today this is still the responsibility of the individual or there must be more signs that exercising is necessary and that means that there must be also problems with the mobility in general. In the case of the 35 individuals there was no indication according the doctors to give this people aerobic or other exercises. There were in their opinion no mobility problems.
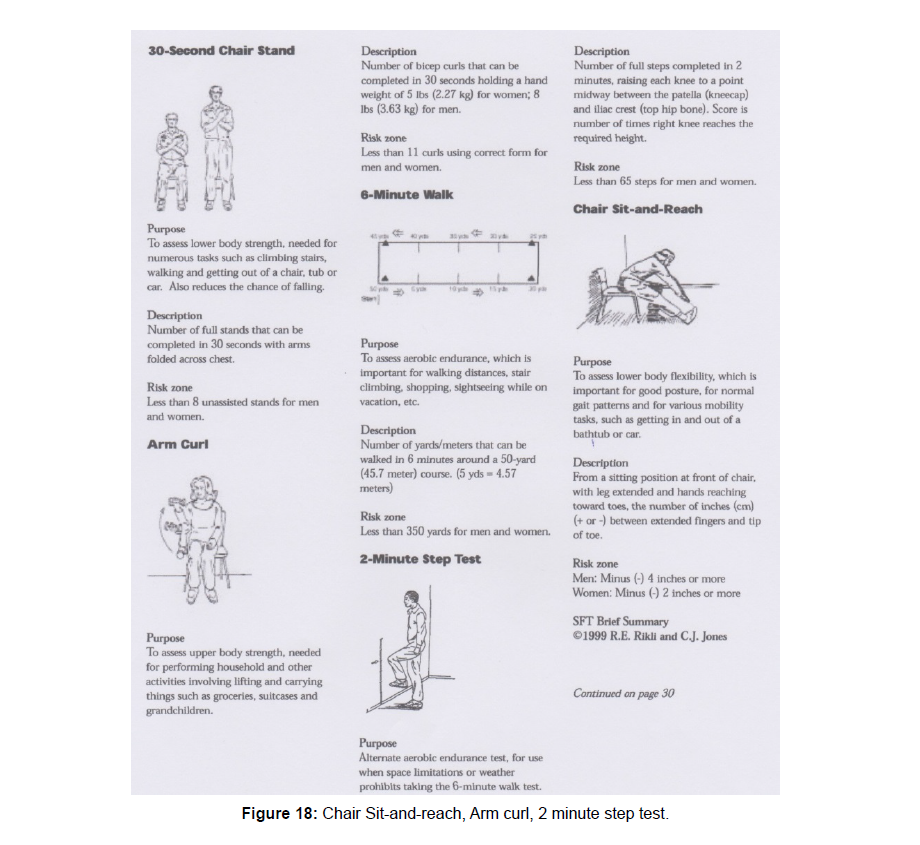
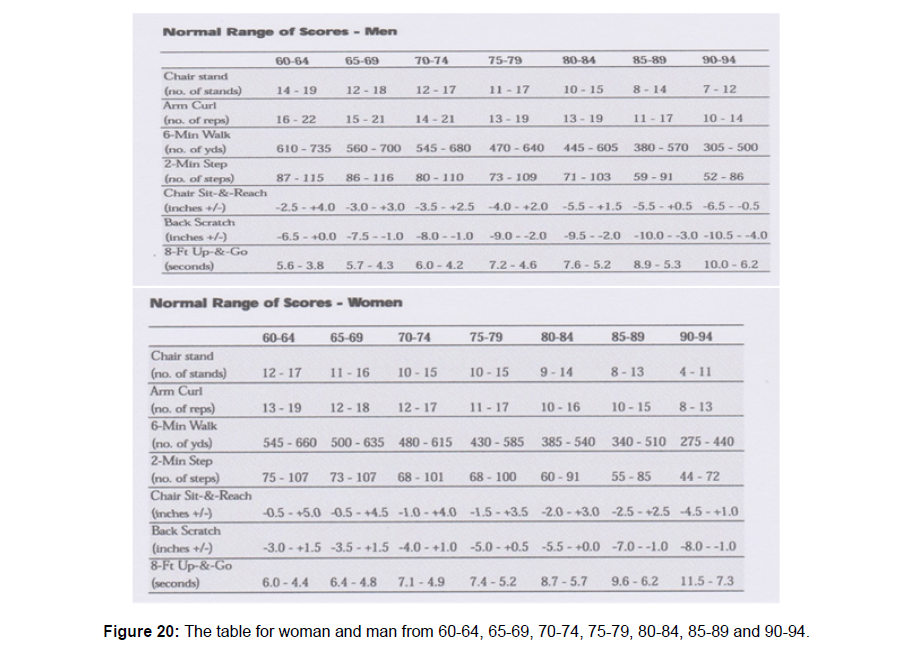
Strange: All member of this group had the indication –dementiaand almost all are walking with a rollator frame and had therefore balance problems, but there was no indication for an program including aerobic and strengthening /balance exercises. To get sure that this people are functioning lower than there age matching people without dementia, we use the Senior Fitness Test of Rikli and Jones out 2002 [25]. This test scheme has 7 items that must be test and can compare with the levels that are found by Rikli and Jones by people that has the same age. In this 7 items are test for walking capacity, balance but also power and mobility. This is chosen to be also in the area of ADL complete and give a signal that performing on such a level is needed to remain independent. Individual with dementia will be having fast problems with the ADL not directly by the mobility sec but through the loss of cognition. That aspect is always different but the other aspect is so well chosen that it is possible to assess what the greatest deficit are and give directly an indication (Figure 16) [25].
The test from Rikli and Jones are: The explanation of the whole test stand in the Figures 15 and 16. Par example the 6 minute walk test gives us details about the aerobic performance of this person (Figures 17 and 18). But we can also use the measurement technique of Toine van de Goolberg how take the heart rate frequency at the beginning and at the end. At the end you can measure after 1 minute and after 2 minute [26]. You can see than what the recovery capacity is from the individual, normal the difference after 1 minute is 25 beats per minute and after 2 minute 30 beats per minute. After 1 minute always lower than after 2 minute –normal!
This gives an indication how hard the heart must work to complete this distance, you know the distance that the individual can do and you know how his recovery possibilities are.
With these measurements you can set up a perfect aerobic exercise program to stimulate the aerobic performance. The back scratch seems not important but in the ADL this is important also the Chair Sit-and-reach, because will also give indications that the shoulders are losing mobility. What is on these photos of group’s gymnastic common problem of the most elderly? Look how height the arms get! Most shoulders are restricted in their mobility and one reason can be the amount of support that is given on the rollator frame. This damage the shoulder-joint and especially elderly with dementia has another pain sense and will complaint on different way but the loss of mobility is clear and need assessment (also echography, Rö- photos and MRI technique) and a proper treatment (Figure 19).
The last items that are testing are balance and strength. All together give this and picture, that we can compare with what age-match individuals without dementia are able of. What was the conclusion after the examining of the 35 individuals on the day – care? That no one was able to achieve the level that was according his/her age and that there were a lot of problems especially in the balance but also in the endurance. That there was an indication for a treatment and these treatments give after 7 weeks by all individuals improvements on balance, endurance, strength and mobility possibilities. That means that through the dementia and the surrounding through the family- care givers- the possibilities to hold the level was decreased and that therefore the level of body functions was to low according the possibilities they still have and that this also had an effect on the cognition. Regrettable this wasn’t tested, but the family - care givers- spoke over better night and less agitation.
Therefore the Phase 4 individuals must be treated as soon as possible and the work of Rikli and Jones is very useful to assess but also give a sign that someone is functioning under his level and that has consequences for the body performances but also for the cognition (Figure 20). A start on the right time can slow down, but often we see an increase, because the level is fall so fast through immobility. That an increase of the possibilities is possible and this individual start than on a higher level and will build more “resistance” against the disease. To get the best results of the treatment in this phase be aware that a good assessment is essential and the best result will be obtain in the home situation. There we must assess what the problems are and how the solved them without immediately using aids, that will take over mobility and strength. Sometimes this isn’t possible but be aware that aids will change the use of muscle and that means that the weaker one isn’t use very much anymore and will decrease further [27]. And start as soon as possible with this assessment because than are often the possibilities to assess properly and is our understanding growing in what dementia by that individual change on balance, perception and power. Also in this stage the alignment is often to assess and that is important because changing in the alignment is normal by older people but that group give feedback through complaints and pain but that pain-perception is altered by individuals with dementia. Often in latter phase it is difficult to exam the joint or something else and in this phase 4, it is possible often with not total normal feedback, but we get an idea what the possibilities of the joints and other tissues are.
To get a treatment on the right level, there must be an organisation that knows the people with dementia and also the people that care for them. That makes it easy to enter their home and do the job. And because most people stay at home so long as possible this treatment / assessment must be starting at home and that can be difficult.
In the Netherlands there is an investigation done what the positive effects are and the costs when the family doctor isn’t waiting in his consulting room on this people but go to this people every month to discuss what the problems are and how that can be solve. In this meeting the doctor can be assist by nurses, therapist etc. [28]. This dementia network is, for the people confronted with this disease, a great relieve because the group professional is talking and thinking with them at their one home. And the cost is much lower!
Another problem is: how can the physical therapist exercise in the home situation. This asks for an approach that gives the individual with dementia and his caregiver the opportunity to speak out their concerns and their wishes. A not an approach in which the therapist tells what there must be done. Exercises and how often and what is good and what isn’t right. In the Netherlands we use the EDOMAH – approach [29] (Ergo therapy by older with dementia and their caregivers) and this approach use a system in which the individual with dementia and the care giver let know what the problems are. Not an direct problem solving approach, also not an making of an “new” home with all kinds of adjustments, but first an identify of problems. And that is often directly related with the problems of the age, but also with coping with the disease and how much freedom both people at home give each other to live further as good as possible on the “old Way”. When that is clear, the doctor can decide which professionals are important in that case and when this is the physical therapist, he must do the same approach and listen to both people and assess their fears and wishes. When the physical therapist has a “tie” with the people in their home, he must do as quickly as possible an assessment. Of course is that often impossible in the beginning but using the senior fitness test is always an good start, but we want to know more and know what the problems are at that moment and seek out why that is an problem and which treatment is possible. Furthermore we want to know what the level is of the functioning and participation is of the individual with dementia because that is very important to get an idea what will happen in later stadia because then is an good assessment much more difficult. But this assessment by the start gives us and picture of that moment and we can learn how fast the development goes and gives us in an latter stadium more possibilities what can be the cause and how to act. Often it is possible to do part of the assessment again and see the difference and that means that the capacity of the brain is decreasing and that we can ask not so much anymore. Assessment contains 3 chapters:
1. WHAT can the individual?
2. HOW he perform?
3. WHY he does this on this way?
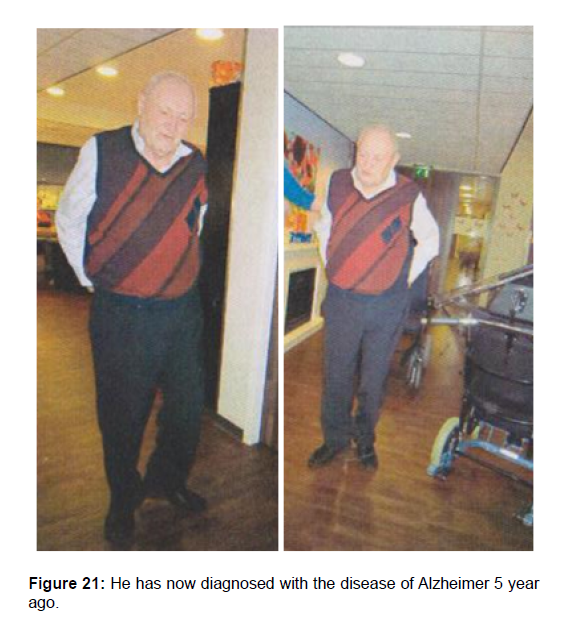
The assessment will now be explained in detail and on the same time we assess the gentlemen on Figure 21.
This makes the assessment often more clear. Mister A. is 80 years old. He has now diagnosed with the disease of Alzheimer 5 year ago. He was living with his wife in their home but his wife was becoming ill and now they are both in an nursing home. He likes sport and was in his youth a football player and till to day, he loves to exercises and get “tired” on a bicycle. He has broken his hip now 10 year ago but he was strong and healthy before he got the Alzheimer disease. Till he was 70 he works on the farm. He had a large farm with cows. He had sport and reading as his hobby. He had always, till now smoked. Reading his medical history there was almost nothing written down, only the hip fracture left after a fall from a bicycle in the mountains of Belgium. It is always good to know or individuals with dementia have interest in doing sport, because than can therapy give a pleasure recognition and the recognized often the feeling of sweet, fatigue and they likes that. That is always a difficulty by all (older) people, that when they have no connection with moving and sport, they will have more of a rest-attitude, because they are afraid that this isn’t good for them. And often is the caregiver also someone that wants to care and is afraid that movement isn’t right [30].
Be honest when we look to older people, we wandering why the all haven’t a “rollator frame “because they are walking with flexion in the hip and the balance isn’t so fast anymore. This culture will prevent people from moving and that is still today a “medicine” for well-being older and a brace on the developmental of dementia.
First part of the assessment
The WHAT part: What can this individual with dementia on this moment? X = performance of mister A.
This is a large part because we want to know what he can do and that we want to see and observe how he is doing this.
- WHAT is divided in 5 columns?
- Independent: Means total independent and it aren’t important how he performed. We use it, also as a moment for clinometric, looking or it is according the description of this test.
- Supervision: means that the person (therapist, nurse etc.) not dare let the individual alone but still he cans it on his own. The same is with the remark safe that is the decision of the therapist at that moment.
- Assistance/ facilitation: the difference is that facilitation make the movement easier and assistance takes over an part.
- Not possible
Clinometric
- Trunk Control Test: [31].
- Berg Balance Scale: [24].
- Stop Walking When Talking: [32].
- One leg standing: [6].
Be aware that individual with a vascular dementia can have a paretic side and then it is important to monitored the differences between left and right. Therefore stand by some points: affected or not-affected side, but this can be change in left or right. And when necessary left and right can be change in affected or not-affected side. This part is very important, when the individual is still living at home. Because often there are some adjustments done, to prevent walking the stairs because of the danger. On the other side, this is also because the individual and the caregiver of other family member think that this isn’t good for the individual with dementia to climb stairs. But stair climbing and especially up is a very good exercise, because it has two very important training elements:
- Aerobe and those we know had a bracing effect on the loss of cognition and of course and positive effect on the cardio pulmonary system. People are still afraid, that old people may not be tired, but that is the stimulus that this people need to get a better quality of live.
- Stair climbing is a Task specific strengthening exercise for the muscle in the leg and with load this is a perfect Task specific resistance exercise that will lead to more power in the leg.
The hand function is often not involved in the start of this disease. But H. Hobbelen [29] has found that some people with the Alzheimer Disease are having a higher tone at the be
We Must Now Ask Yourself the Question: “What Will Change the Use of The Handles”?
The answer is simple, the use of the legs will be lesser and that will make the movements in bed difficult and on the moment that his power in arm gives no solution, he is dependent of others. Now it is important to search why he cannot use his legs on the right way and is this changeable with a treatment. How performed an individual the movement is very important and will give use a hint where we must search in the WHY and get a good treatment possibility. And it is very important to look how others make this movement. There is a great difference between this movement performed by young people and people above the 60. But there are a lot of variations; we must therefore see of that variations are good solutions.
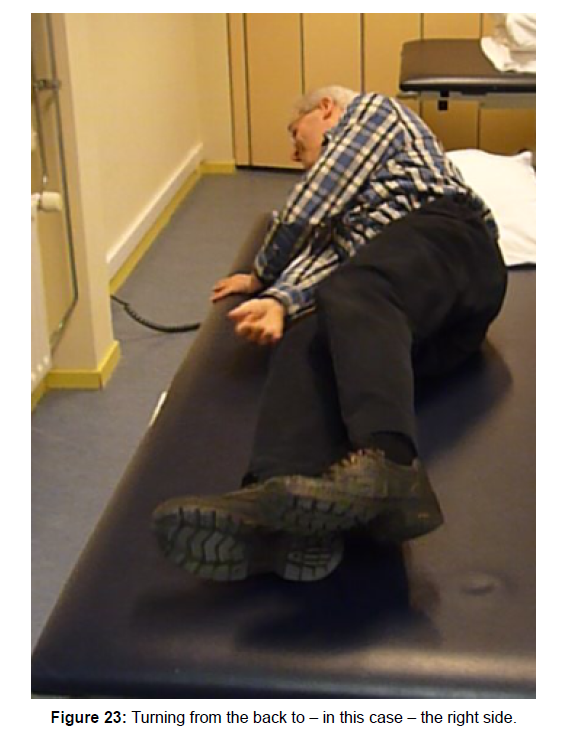
Turning from the back to-in this case-the right side. Start with the push off of the left leg. That stimulated the back diagonal of the left leg (you can still see the print in the bench). Than the front diagonal, starting in the upper trunk left and through the lift of the head is activated. And the turn movement is no almost half way. Now the left leg stop with pushing and must be lift up and mostly goes over the right leg to the other side. That requires a stabilisation through the right (leg on the bench). That is now the leg that gives the stabilisation and that is a function of the back-, front and the homolateral structures especially in the hip and the foot [36]. On this photo the whole foot isn’t on the bench but when the forefoot is there, this will together with the rotator muscle controlled the movement and created the stability (Figure 23).
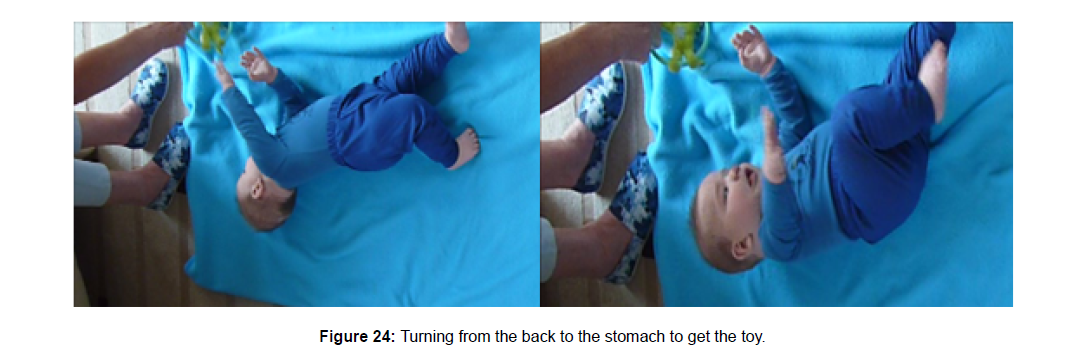
When he is almost on the end his left arm supported the movement and stability and he is in this position capable, after each other, to move his lower trunk and this upper trunk and lie in the middle of the bench. This will be very difficult for the individual on photo 9 because his legs are bend and he has the stability and lift possibilities only then when he complete lies on that side. We do this in one movement on the end, turning and going backward. When we lying on the side than is this the moment to bend our knee(s). This gives the greatest stability and will decrease the tone. Every time it is amazing how much power and selectivity this movement cost and we haven’t incorporated aspects as control over the blankets when we turn. By little children this will be one of the first movements that occur. Than the development of the diagonal is starting and will the front and back diagonal work together and will rotation be possible. But because the selectivity is still poor this is a movement with great effort. My grandchild demonstrated this by pushing with one leg (back diagonal) and at same time the front diagonal on the other side is active, we see that this leg is free. But this not enough to get to the toy and on his stomach (Figure 24). We need an action of the front diagonal, reaching with the head down gives no activation, therefore head up and leg up to get the front diagonal in action but on the same time is back diagonal also active and therefore go the reaching arm backward. The toy will be in his hand only when he turns on his stomach. Turning from the back to the stomach to get the toy. First: Push with the right leg, the arm is reaching but the head is still in extension and therefore the turn will stop. This action gives an extension in the other leg, a sign that the back diagonal is active. To get out this position and get to the toy, he must active the front diagonal. Therefore he must lifted his head but that asked for an stabilisation of an part of the back diagonal and that means that the reaching arm goes back in retraction but the turn takes placed and he get his toy.
Coming to sit
How he performed isn’t so important. Important is that he is able to do it on his own. Often we see that individuals sit up in bed and then turn the legs out of the bed and sit on the edge, mostly this is a movement that has components of long sit or turning on the side and from side lying position coming to a sit position. Figure 21 shows a strategy in which there is first and turn on the side and then a sitting up procedure. The movement to get sitting on the edge of the bed and the speed is so limited that he must search for point to push (right arm) and to pull (left). When he is stabilized in this position on his right elbow, he try to grasped the blankets and pull himself up in an sitting position on the edge of the bed. He does very much with his arms and that gives us an crucial information. All is good but an T.C.T [30] will not be 25 point when this individual don’t reach the sitting position and require assistance or when he must pull with his left hand on the blankets to reach that position, than it is 12 points. Therefore look how he performed and realize that he with pulling on the blankets or the edge of the bed, has not the full independently. Of course he may use his hand to push him up but not pull himself up. Because that is a sign that the lower trunk isn’t capable to do his job. We see that he must work more with his arms than would be necessary and that means often that his lower trunk/hip isn’t capable to create so many powers that in effort of the arms aren’t necessary. The person on Figure 25 remain this position because the photo must be made, but on Figure 21 stay in this position because this was the moment that the other arm must work (pulling on the blankets that normally lies on him) to get in an sitting position. The difference is the lower trunk, the amount of tone in the right leg ( starting point of the diagonals and an key point ) is must higher and is visible in the whole leg all away to the foot and we see that the other leg is also active and will contribute. In Figure 21 this is weaker and that is particular clear in the amount of exhortation of the right hip, the movement of the feet and opening between both legs [37]. The two lines in blue give the amount of power that is generated in the lower trunk/hip by the persons and then the difference is great. Not alone the angle in the under leg but also in the stand of the legs in the hip and the activity in the whole leg par example the feet. Photo 14 gives an base that allow this person to make an elongation in the trunk, on Figure 21 there can be no elongation because the base isn’t good enough. And that means that this person isn’t always able to get out of his bed and is on time by the toilet.
Standing up
Mister A. stand up independent but still we see that there is an X-mark by supervision.
That means that the person that assessed, wasn’t sure that this was going well.
It cans also a sign that the therapist wasn’t sure that after the standing up procedure, the standing and walking was safe. Still this is a personal interpretation and therefore is it important to look how the standing up performance takes place. Standing up is so important because, when this is gone, than will independent walking also in his start dependent from others.
The reason can be: That the balance isn’t yet required and that seem the case on photo 15. Because there is a stillness in his whole attitude. And that means that he is supporting on his arm and makes no effort to go further. The perception of his balance is stays in the arms that supporting his body and no reaction are there in his feet.
But it can also, that he cannot go further and must be sitting back in his chair. Now can this be a sign that he has experienced that this cannot work. He dear not to go further! But when he goes further without the reaction of the feet is that a clear sign that the perception about his balance surface is serious disturbed and because he isn’t aware of it is will be lead to falls. Avoid that and still give him the chance to get on his feet, place a table in front of him and he is then also working on a better balance perception when that is changeable. Back to Figure 26, there we see the reaction in the feet but we see also that they are standing too far to the front and that his upper body isn’t far enough to the front and that his upper leg stands against the bench. He makes an upper trunk forward but he try to push him against the edge of the bench to a standing position.
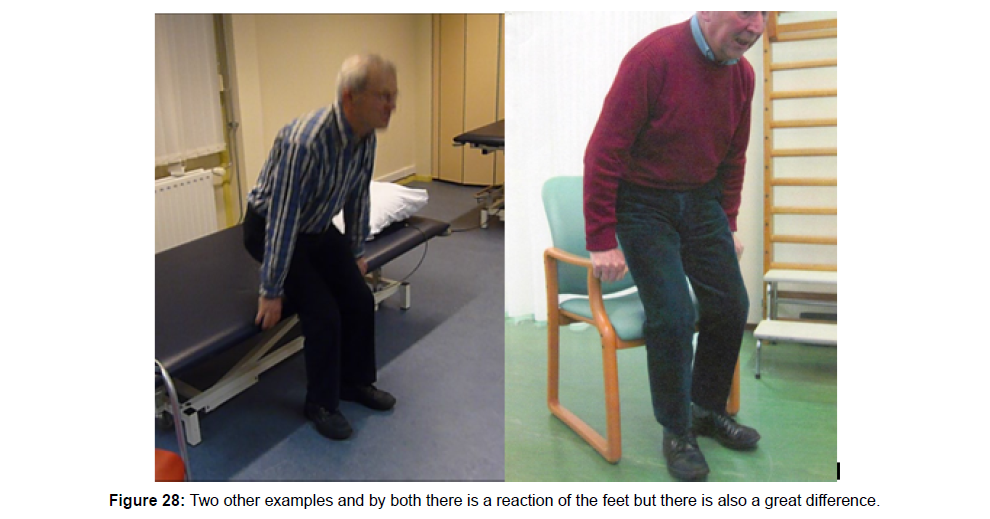
Positive is the reaction of the feet, that means that his brain are aware that the balance isn’t right and is too far behind. Here we expect a correction! Figure 26 will be search for an solution because there is no dangerous and the movement to the front can he do without more risk, the gentlemen on photo 15 will exercises standing up but will never stand stable of will frequent fall. Figure 26 a man standing up from a bench, his feet stand not precisely correct and that ask for a correction in the rest of his body. He has an erect spine thus it is a lower trunk forward movement but there is more flexion than necessary because this hand are still against the bench
Figure 27 Here we see a great reaction in the feet and that means that the system is aware that he is falling to the back when he released the support on his hands. In this position he is dependent from someone else or must try by an acceleration to get the support correct above his feet. Two other examples and by both there is a reaction of the feet but there is also a great difference [37]. But now can occur that the chair is gliding back and then this situation is very dangerous. The difference between the two photos is the support on the hand.
By Figure 26 there almost no support and the correction will done in his ankle and that makes the position safe.
The person on Figure 24 isn’t capable to make that adjustment because the support on the hand is too big and the body is too far behind his feet. This looking HOW is very important because there are many strategies to move in bed, out the bed and out a chair, toilet etc. It is therefore not directly a search, what is wrong and what is correct but how the person makes the movement and what is the result. Is the person in balance than the movement can be very strange but within his ability and we must look or he is capable that strategy to use by other chairs etc.?
When that is also in balance than we see here an adaptation that give stability and is there no reason to correct it. Interesting is WHY, he act so!! But is his strategy dangerous, than we must search WHY he perform this on this way and search for the difficulties. Often will the same strategy be used in all situations – in this case standing upand can lead in a later stage to an loss of independency. The HOW part we discuss the walking and then particularly the stand phase. But every item that isn’t independent much be look: HOW the individual performed because our treatment must be complete. Not only the walking part, but all the transfers are very important because that will stimulated him to be independent so long as possible.
Part two
- How: Selected task ( the assistance call of the patient) Common elements of this task
- How functional is the patient? Assess if the patient is safe, impulsive, scared, over active, have they considered their limitations?
- How is he orientated on his task? Is there an preparation, goal attention, spatial orientation ( the position of his body in the room, distance, direction, in handling of objects and the place and function of this object and has he eye for surrounding.
This tells us how the individual with dementia go to work, what his normal preparation is but also or he understand what we want to see. Understand him this verbally or must we let see the movement before there is a reaction. Verbal instruction is a higher brain function and often is showing a better solution because people with dementia can good imitate. But be aware that the imitated your movement!!
- How is the execution of the task? Temporal organization, initiation of the movement, the sequence, procession and the completion of this task.
- How move the patient? Is his movement fluently, coordinated, with variation and with enough power?
This is question that pointed on the execution of the task and below stand and question; is there adaptability when the situation is changing.
- Is the patient capable to adapt on changes? When the surrounding change how he reacts? On the orientation, the execution and completion of the task. What is happen when there is an increase on the task trough stress or double tasking?
- Not in details that will be done in the next page, but overall impression how acts when he is walking and particularly standing on his (right) leg.
- Selected task (How) (stand phase on the right side)
- Specific elements of the task (movement pattern)
But only Figure 27 gives a picture of the standing phase on the left leg. But on Figure 24 there is in the standing phase -right and leftmore weight on the forefoot than on the heel. That will be important to investigated in the WHY part. And we see that he makes an upper trunk sideway when he stands on his left leg. Why? And why are his arms on the back? Observe how the floor is shining, on both photo’s the shadow of his legs is visible in the floor and that will disturbed everybody and especially a person with dementia. Describe one task that is representative for his activity level. Choose a task and describe this and when it is possible make also photo(s):
- Head (Pay attention on the attitude of the head but also on the place and structure of the tongue bone/tongue and the neck muscle on the front). His head is in flexion and clearly he is concentrated on the floor and the way he must go. The flexion of his neck looks as an elongation of the cervical spine.
- Trunk (where start the movement in the trunk (upper or Lower trunk) in the upper trunk. The attitude is an upper trunk forward with flexion but this movement is restricted by the way he holds his arms. Lower trunk and little pelvis shift to the back. And left an upper trunk sideway.
- Shoulder / arm / hand: Observation of the arm isn’t possible, because both arms are behind the back in each other and that means that there is a retraction in the scapula and that inhibits the upper trunk going forward further. The position of the arms gives an upper trunk backward.
- Pelvis/leg/Foot WHY walk this person on this way and which opportunities there are to change this. We can give him an rollator frame and then will this walking pattern change, but we never have investigated, why he walk like this and by giving an aid, he will adapt his strategy and when than cost less, he will continued to use the aid.
But what will change in his perception and muscle activation and will his ability increase? In the WHY part we will use this individual as an example to explain the WHY part. The movements in the hip and knee are small, both feet stand in exhortation and the most of that exhortation comes out the hip. The feet are only very short of the ground, there is no heel-strike. The weight of his body stands more on the forefoot than on the heel (Parkinson like). The step length is short and the weight distribution on the right leg is small and not complete. He never stands complete on one leg! He walks but it looks that he can stumble every minute!!
To summarize the WHAT part of this man: Turn in bed, he use his arms by pulling on the edge of the bed.
To come to sit on the edge he must use his arm to pull on the blankets walking is possible in home without an aid but on the way above or by holding the wall-railing. Standing up out a chair, he can do it but use the arm rest and it is a little bit grisly. Stair up no problem, down- he do it reverse. When he is walking, he cannot do something extra. Nobody must talk and he cannot take something with him (Figure 28). Outside he walks with his wife in the arm. His hands are perfect and he can in sit everything, even the smallest things. ADL washing and dressing is done by the nurse or his caregiver, only undressing is no problem swallowing no problem.
Conclusion
The WHY part starts with an investigation of the selectivity. That can be done in a lying position, but also in sit and stand. But it is wise to start with a lying position and look of he is lying down in the center of the bed/bench. No verbal instruction first watch and after that you ask or he is lying in the center. When that isn’t the case ask him to correct and observe how he is doing that.
Need he and visual correction? What is he doing with his arms etc.? This is a part of the perception but every time he is lying in bed/bench do it and observe! Also look what he does with his hands and legs. Perception assessment is very difficult but by observing we get information. Par example; Lies his arms/hand on his stomach and touch each other? Lies his legs against each other or cross over or in an exhortation with no touch? This seems all normal but when someone lies for 5 minutes than is normal that the feet cross or touch each other also the arms. When he sits on the edge of the bench/bed, place the bed higher so that the feet don’t touch the ground and observe his attitude and his legs (Figure 29). Normally his legs will move after a while and that is an sign that the brain is asking for information, where the legs are. When the perception is disturbed this information the feet are remaining still. This is signs that the feet are not well “in the brain” anymore. In this case this gentlemen lies oblique for more than 10° and his feet are still, sitting on the edge and lay the whole time in exhortation and don’t touch each other. Trunk Control Test: 25/25/12 (Coming to sitting position, pull on the blanket) 25=87. Berg Balance Scale; 33/56 especially the standing part. Stop Walking When Talking: not possible. One leg standing; 10 sec. Rikli & Jones: 80 year- 6 tests far beyond the age level only the arm curl was good. Sit to stand 8/6 minutes 100 m/Steps 50/ Reach 8 inch/Back reach 15 inch/Time up and go 14 sec.
References
- Van de Rakt J (2001) The “Raktâ€concept. physiotherapy & elderly care
- Bossers WJ, Van der Woude LH, Boersma F, Hortobagyi T, Scherder E, et al. (2016) Comparison of effect of two exercise programs on activities of daily living in individuals with dementia. J Am Geriatr Soc 64: 1258-1266.
- Groot C, Hooghiemstra AM, Raijmakers PG, van Berckel BN, Scheltens P, et al. (2010) The effect of physical activity on cognitive function in patients with dementia: A meta-analysis of randomized control trials. Ageing Res Rev 25: 13-23.
- Erickson K, Weinstein AM, Lopez OL (2012) Physical activity, brain plasticity, and Alzheimer's disease. Arch Med Res 43: 615-621.
- Van de Rakt J (2019) Support on rollator frame, negative effects! In progress. Italian Journal.
- O’Keefe J, Fam Moser, (2014) Neural representations of location.
- En Anderen (2013) Leidraad Psychogeriatrie. Houten, Bohn Stafleu Van Loghum.
- Duysens J, Bombach GD, Duysens J, Carpes FP (2015) Differences in foot sensitivity and plantar pressure between healthy young and elderly. Arch Gerontol Geriatr 63: 67-71.
- KuruAlıcı N, Zorba Bahceli P, Emiroğlu ON (2018) The preliminary effects of laughter therapy on loneliness and death anxiety among older adults living in nursing homes: A non-randomised pilot study. Int J Older People Nurs 13: e12206.
- Kraft P, Gadeholt O, Wieser MJ, Jennings J, Classen J, et al. (2009) Lying obliquely-a clinical sign of cognitive impairment: cross sectional observational study. BMJ 339: b5273.
- Karnath HO, Ferber S, Dichgans J (2000) The origin of contraversive pushing: evidence for a second graviceptive system in humans. Neurology 55: 1298-1304.
- Cahill LS, Lannin NA, Mak-Yuen YYK, Turville ML, Carey LM, et al. (2018) Changing practice in the assessment and treatment of somatosensory loss in stroke survivors: protocol for a knowledge translation study. BMC Health Serv Res 18: 34.
- Schädler S, Kool J, Lüthi HJ, Marks D, Oesch P, et al. (2006) Assessment in der Neurorehabilitation Verlag Huber.
- Hobbelen JS, Koopmans RT, Verhey FR, Van Peppen RP, de Bie RA, et al. (2006) Paratonia: a delphi procedure for consensus definition. J Geriatr Phys Ther 29: 50-6.
- Hobbelen JSM, de Bie RA, van Rossum E (2003) The effect of passive movement on the degree of paratonia. A Partially Blinded Randomized Clinical Trial 6: 132-137.
- Hobbelen JS (2010) Paratonia enlightened Defenition, diagnosis, course, riskfactors, and treatment.
- Bohannon RW, Suith MB (1987) Interrater reliability of a modified Ashworth scale of muscle Phys Ther 67: 206-207.
- Waardenburg H, Elvers JWH, Vechgel FV, Oostendrop RAB (1999) Is paratonie betrouwbaar te meten? Nd Tijdsch v Fysio.
- Telenius E, Engedal K, Bergland A (2015) Long-term effects of a 12 weeks high-intensity functional exercise program on physical function and mental health in nursing home residents with dementia: a single blinded randomized controlled trial. BMC Geriatr.
- Nielsen J, Willerslev-Olsen M, Christiansen L, Lundbye-Jensen J, Lorentzen J, et al. (2015) Science -based Neurorehabilitation : Recommendations for Neurorehabilitation from basic science. J Motor Behaviour.
- Graff M, Melick MV, Thijssen M, Verstraten P, Zajec J, et al. (2010) Occupational therapy in the elderly with dementia and their informal caregivers.
- Hyndman D, Ashburn A (2004) Stops walking when talking as a predictor of falls in people with stroke living in the community. J Neurol Neurosurg Psychiatry 75: 994-997.
- Bautmans I, Demarteau J, Cruts B, Lemper J-C, Mets T, et al. (2008) Dysphagia in elderly nursing home residents with severe cognitive impairment can be attenuated by cervical spine mobilisation. J Rehabil Med 9: 755-760.
- Bishop M, Brunt D, Pathare N, Koo M, Marijama-Lyons J, et al. (2005) Changes in distal muscle timing may contribute to slowness during sit to stand in Parkinsons disease Clin Biomech Journ 20: 112-117.
- Robinovitch SN, Feldman F, Yang Y, Schonnop R, Luen PM, et al. (2012) Video capture of the circumstances of falls in elderly people residing in long-term care: an observational study. Lancet 381: 47-54.
- Yang Y, Mackey DC, Liu-Ambrose T, Feldman F, Robinovitch SN, et al. (2015) Risk factors for hip impact during real life falls captured on video in long term care Osteoporos Int 27: 537-547.
Citation: de Rakt JV, McCarthy-Grunwald S (2018) Dementia Part One: A Physical Treatment of Individuals with Dementia. J Dement 1:107.
Copyright: © 2018 de Rakt JV, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 5147
- [From(publication date): 0-2018 - Dec 21, 2025]
- Breakdown by view type
- HTML page views: 4090
- PDF downloads: 1057