Effects of Vestibular Rehabilitation Therapy on Postural Control and Quality of Life in Patients after a Surgical Microvascular Decompression of the Cochleo-Vestibular Nerve
Received: 03-Jul-2017 / Accepted Date: 24-Aug-2017 / Published Date: 31-Aug-2017 DOI: 10.4172/2161-119X.1000318
Abstract
Introduction: The purpose of this study was to evaluate the effectiveness of a vestibular rehabilitation therapy (VRT) on the static and dynamic postural control and on the quality of life in patients after a surgical microvascular decompression of the cochleo-vestibular nerve. Method: Eight patients with a neurovascular conflict were submitted to a surgical microvascular decompression at the Hospital (France). Four patients (G1 group) benefited from VRT whereas four other patients (G2 group) returned to their daily life functions and professional activities without VRT. VRT combined exercises on both rotary chair and dynamic post-urography platform and started 7 days after surgery. Evaluation of the postural performance with (EO) and without vision (EC) and during optokinetic stimulation, was carried out in the two groups before (REF), seven days (DAYS 7) and two months (DAYS 67) after the surgery. Questionnaires on the quality of life (SF-36) were administered on DAYS 67 in both groups. Results: The statistical test performed on the posturography data collected under static and dynamic conditions did not show any significant differences between the two groups in EO, EC and during optokinetic stimulation before surgery and on DAYS 7. By contrast, the postural performance in static and dynamic conditions was significantly improved (p<0.05) in the patients who benefited from the VRT with (EO) and without (EC) vision on DAYS 67. Maintaining balance on an unstable platform with optokinetic stimulation was impossible on DAYS 67 for the patients without VRT whereas the patients with VRT succeeded in this more challenging condition. The SF-36 questionnaire was also better in the patients who benefited from the VRT compared to the patients without VRT. Conclusion: This pilot study shows that VRT improves significantly the postural control and the quality of life as well after surgical microvascular decompression. This conclusion must be confirmed on a larger group of patients.
Keywords: Syndrome of compression of the cochleo-vestibular nerve; Microvascular decompression surgery; Vestibular rehabilitation therapy; Postural control; Quality of life
256165Introduction
The syndrome of compression of the cochleovestibular nerve due to a neurovascular conflict is still a somewhat controversial clinical entity [1]. The main reason is that the eighth cranial nerve includes both cochlear and vestibular nerve components (superior and inferior branchess) and its compression can lead to complex symptomatology [2,3]. The main symptoms are intractable and incapacitating tinnitus, short attacks of spinning (or non-spinning) vertigo that generally last less than one minute and occur in a series of up to 30 per day (vestibular paroxysmia), sensory deafness, dizziness and frequent falls [4], causing significant morbidity and impaired quality of life [5].
One of the most relevant concept explaining the pathogenesis of the compression of the cochleovestibular nerve is the so-called “ephaptic discharges” theory. The human vertebrobasilar arterial system is never perfectly symmetrical [6]: the unilateral vertebral artery is more prominent if its contralateral vertebral artery is hypoplastic. A winding basilar trunk can also be observed. Then, a mechanical friction may occur at different levels when the prominent arterial trunks or their branches are in contact with different central structures in the ponto- cerebellar angle, producing over time real electrical short circuits at the periphery nerve level or in-between the fibers in the nerve. Another concept is the so-called “nuclear theory” relying on a hyperreactivity in the nuclei of the cranial nerves.
Newly, highly sensitive brain Magnetic Resonance Imaging (MRI) techniques have investigated the relationship between intracranial vessels and nerves in a non-invasive manner. De Abreu Junior et al. [7] used MRI to identify vascular loops in the anterior inferior cerebellar artery and evaluated their relationship with otologic symptoms. Their results demonstrated that the vascular loops do not appear to be associated with the otoneurological manifestations (global measurement of tinnitus, hearing loss and dizziness). According to Brandt et al. [3], vestibular paroxysmia may however manifest when arteries in the cerebellar pontine angle cause a segmental, pressure-induced dysfunction of the eighth nerve. The symptoms are usually triggered by direct pulsatile compression with ephaptic discharges, less often by conduction blocks [8-10]. MRI revealed neurovascular compression of the eighth nerve in more than 95 % of the cases (3D constructive interference in steady state and 3D time-of-flight sequences). Only blockers of the fast sodium channel such as carbamazepine or oxcarbazepine are theorically effective. The studies of Brandt et al. [11] and Best et al. [10] found that both agents were effective in low dosages ranging between 400 and 900 mg/day. Oxcarbazepine reduced the mean number of days with vertigo compared to placebo, but the drop-out rate was >50%. Finally, surgical microvascular decompression of the cochleo-vestibular nerve (MVD), that is the “ultima ratio” for medically intractable cases, is a safe and effective surgical procedure for treatment of severe tinnitus [12] and/or vertigo [13-17] in such patients.
The purpose of this study was to evaluate the effectiveness of a vestibular rehabilitation therapy (VRT) after a surgical microvascular decompression of the cochleo-vestibular nerve a) on the postural control recorded in static and dynamic conditions using post-urography, b) on the perception of vertigo and dizziness and on the quality of life by means of questionnaires. The central hypothesis is that both objective measurements and subjective evaluations should be improved in the patients receiving VRT compared to those without VRT. It is based on well-conducted clinical trials showing that VRT is safe and effective in many peripheral vestibular pathologies [18,19] and particularly if VRT follows several basic principles (cf [20] for review).
Material and Methods
Subjects
This pilot study was conducted in 2015 in accordance with the 1996 Helsinki Declaration.
Eight patients were followed at the Hospital (Conception, Marseille) in the framework of health care. At the clinic visit before the surgery, the patients reported having suffered from positional vertigo and dizziness for the past few years. The patients had previously undergone periods of vestibular rehabilitation therapy and medical management, which might include vestibular suppressant medication, but without any beneficial effect. The patients reported frequent falls. No motor facial symptom was reported. Unilateral hearing loss was present, with tinnitus, but the neurological examination was normal. Brain magnetic resonance imaging (MRI) evidenced a microvascular compression of the cochleovestibular nerve (eighth nerve). Surgical microvascular decompression of the eighth nerve was proposed as the ‘‘ultima ratio’’ for these medically intractable cases.
Four patients (G1 group: Mage=59.5 ± 5.8 years) benefited from vestibular rehabilitation therapy (VRT) after the surgical microvascular decompression of the cochleo-vestibular nerve, whereas four patients (G2 group: Mage=52.0 ± 3.5 years) returned to their daily life functions and professional activities without VRT. The socio-professional category of the patients, who declined the vestibular rehabilitation therapy, included self-employed workers and craftsmen.
VRT started seven days after the surgery. VRT was performed during 8 weeks, 4 weeks in a vestibular rehabilitation center (Medical center, Rhône Azur, Briançon in France) and the last 4 weeks in a private office. VRT consisted of exercises using both a rotary chair and a dynamic post-urography platform. The patient was engaged behaviourally and actively after his/her surgery. VRT included exercises with eyes open, eyes closed and eyes open with optokinetic stimulation. Intensity and duration of the exercises were adapted to the physical capacity of each patient. VRT sessions were held twice a day over the course of 2 months.
Operative technique
The patients underwent a microvascular decompression procedure using a minimally invasive retrosigmoid approach according to Guevara et al. [12]. A limited craniotomy behind and close to the sigmoid sinus was performed (approximately 1.5-2 cm in diameter). The dura was opened with a U-shaped incision after hyperventilation to diminish cerebrospinal fluid pressure. The cerebellum was depressed spontaneously and progressively without use of a retractor, helped by cerebrospinal fluid aspiration of the cerebellopontine angle cistern. A 30 degrees endoscope was then used to explore the cerebellopontine angle, allowing clear visualization of the cochleovestibular nerve and precise localization of the neurovascular conflict [17]. The site of conflict was found and a small cushion of fat was inserted between the offending vessels and the nerve. Before closure, the stability of the fat, which ensured complete decompression, was checked through the endoscope.
Clinical testing
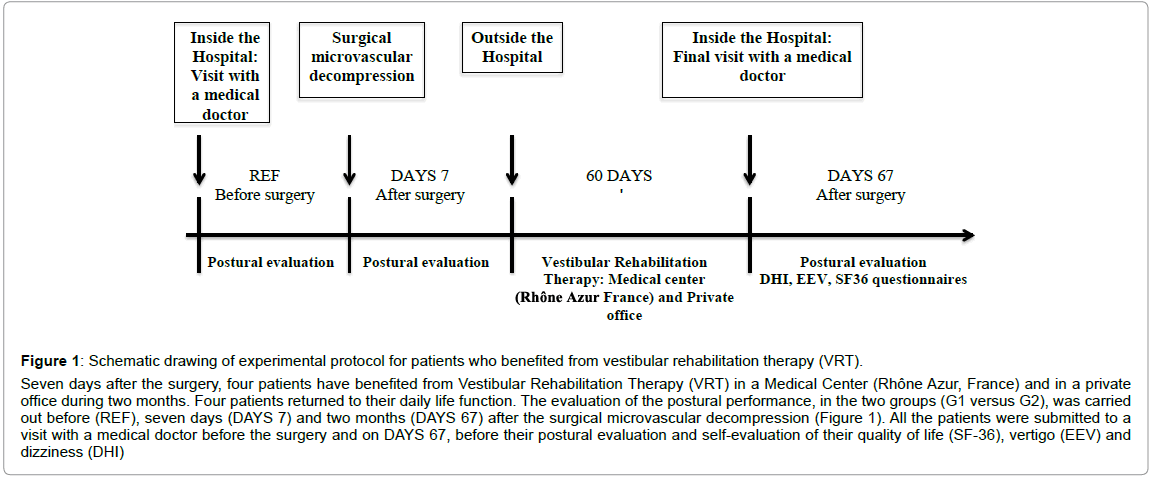
The evaluation of the postural performance, in the two groups (G1 versus G2), was carried out before (REF), seven days (DAYS 7) and two months (DAYS 67) after the surgical microvascular decompression (Figure 1). All the patients were submitted to a visit with a medical doctor before the surgery and on days 67, before their postural evaluation and self-evaluation of their quality of life (SF36), vertigo (EEV) and dizziness (DHI).
Evaluation of the postural performance: Post-urography: The post-ural recordings were performed using the ‘‘Multitest Equilibre’’ apparatus (Framiral, Cannes, France), which behaves both as a static and a dynamic post-urography platform [21]. The postural conditions were chosen so as to implicate different sensory information and different levels of task difficulty: (a) stable platform eyes open (static EO); (b) Stable platform eyes closed (static EC); (c) stable platform with optokinetic stimulation (stable optokinetic); (d) unstable platform eyes open (Dynamic EO); (e) unstable platform eyes closed (dynamic EC) (f) unstable platform with optokinetic stimulation (dynamic optokinetic). In the (c) and (f) conditions, the patient was exposed to optokinetic stimuli via a ‘‘high-tech’’ full-field visual environment rotator. The hightech stimulus (Stimulopt; Framiral, Cannes, France) provided full-field visual motion in the y- and z-axes, the direction and speed of which were servo-controlled [22]. The stimuli included 2 individual sequences of optokinetic stimulation in a clockwise and counterclockwise, vertical direction at 15°/s within a limited view field (120°). Recordings in each condition lasted 30 s, with the patient standing barefoot, without voluntary gestures, hands along the body vertical axis and gaze fixed on a real (EO condition) or virtual (EC condition) target. The patient’s postural performance was evaluated in the six postural conditions (static EO, static EC, static Optokinetic, dynamic EO, dynamic EC and dynamic Optokinetic). A resting period of 1 min was observed between each recording session to avoid muscular fatigue effects. Two trials in each condition were done. Displacements of the center of foot pressure (CoP) were sampled at 50 Hz and used to measure the velocity (mm/s) of the body sway. This traditional approach has been complemented by a more accurate non-linear analysis of CoP displacements using the wavelet transformation. The wavelet analysis software (PosturoPro, Framiral, Cannes) provides a time-frequency chart of body sway and a 3D representation of body sway under both static and dynamic conditions [23]. This method gives access to the changes in the frequency components of body sway with time, the third dimension being calculated as the decimal logarithm of the spectral power given on the 3D map by a color code. Postural performance in the static conditions was evaluated through a postural instability index (PII) derived from the wavelet plots [24]. The PII values were computed for three frequency bands (F1: 0.05 Hz-0.5 Hz; F2: 0.5 Hz- 1.5 Hz; F3: 1.5 Hz-10 Hz) corresponding to frequency domains mostly related to vision (F1) and vestibular/somatosensory (F2) contribution to posture control. As a rule, the spectral power in the high band (F3) is not present in healthy subjects during quiet standing, but it can be seen with aging, in patients with postural pathologies and of course in the dynamic postural conditions. The algorithm used to compute the PII was as follows:
PII=Sx Sy SP (F1, F2, F3)/TC (F1, F2, F3)
where SP and TC are the spectral power density (in arbitrary units) and time cancellation (seconds) of the body sway frequencies, for each of the three frequency bands. In healthy adults, the PII value recorded in the eye open condition during quiet standing is close to unity while it is significantly increased (up to 4-5) in pathological cases, in older adults during dual- tasking and even more in dynamic conditions [24].
Questionnaires after the surgical microvascular decompression: All the subjects were investigated with three questionnaires: the Dizziness Handicap Inventory (DHI), the European Evaluation of the Vertigo Scale (EEV) and the Quality of Life scale (SF-36). The DHI, EEV and SF-36 questionnaires were administered on days 67 (Figure 1).
Figure 1:Schematic drawing of experimental protocol for patients who benefited from vestibular rehabilitation therapy (VRT).
Seven days after the surgery, four patients have benefited from Vestibular Rehabilitation Therapy (VRT) in a Medical Center (Rhône Azur, France) and in a private office during two months. Four patients returned to their daily life function. The evaluation of the postural performance, in the two groups (G1 versus G2), was carried out before (REF), seven days (DAYS 7) and two months (DAYS 67) after the surgical microvascular decompression (Figure 1). All the patients were submitted to a visit with a medical doctor before the surgery and on DAYS 67, before their postural evaluation and self-evaluation of their quality of life (SF-36), vertigo (EEV) and dizziness (DHI)
The dizziness Handicap Inventory (DHI): The Dizziness Handicap Inventory Test (DHI) is a questionnaire on the consequences of vertigo and dizziness [25]. It consists of 25 items related to the physical, functional, or emotional aspects of vertigo and dizziness. Each item is evaluated on a three point scale – “yes”, “sometimes” or “no” – scored as 4, 2 or 0, respectively. The maximal scores were 28, 36 and 36 for the physical, functional and emotional items, respectively. A global score was obtained by adding all items, with a maximum of 100 points.
The European evaluation of vertigo (EEV): In contrast, the European Evaluation of Vertigo scale (EEV) is a physician- administered questionnaire that only assesses symptoms of the vestibular syndrome. It consists of five equally weighted items scored from 0 to 4 on a categorical five-point scale. The following five items are considered: “Illusion of Movement”, “Duration of the Illusion”, “Motion Intolerance”, “Neurovegetative Signs” and “Instability” [26].
The quality of Life (SF-36): The SF-36 questionnaire or “SF-36” is a generic quality-of-life scale widely used throughout the world [27]. It consists of 36 items divided among eight dimensions: “Physical Functioning” (10 items), “Physical Role” (4 items), “Bodily Pain” (2 items), “General Health” (5 items), “Vitality” (4 items), “Social Functioning” (2 items), “Emotional Role” (3 items), “Mental Health” (5 items). The higher the score, the better the patient’s health status. Global physical and mental scores were obtained by adding all physical and mental items, respectively.
Statistical analysis
The comparison between the two groups was processed through a Mann-Withney U test for all the parameters (Post-urography: CoP Velocity, Postural Instability Index (PII), Spectral Power Density; DHI: Physical, Emotional, Functional and Total scores; EEV: Illusion of Movement, Duration of the illusion, Motion Intolerance, Neurovegetative Signs, Instability; and the SF-36: Global Physical score and Global Mental score). The first level of significance was set at p<0.05.
To evaluate the vestibular rehabilitation effects on the whole set of postural parameters, the comparison between initial (REF) and post VRT or without VRT (DAYS 7 and DAYS 67) was processed through a non-parametric analysis of variance (Friedman test), the post hoc analysis being achieved through the Wilcoxon T-test. For all tests, the first level of significance was set at p<0.05.
Results
Static postural control intergroup comparison
The statistical test performed on the post-urography data collected under static conditions (CoP velocity and Postural Instability Index) did not show significant differences between the two groups G1 and G2 in all tested conditions (EO, EC and with optokinetic stimulation) before and seven days (DAYS 7) after the surgery.
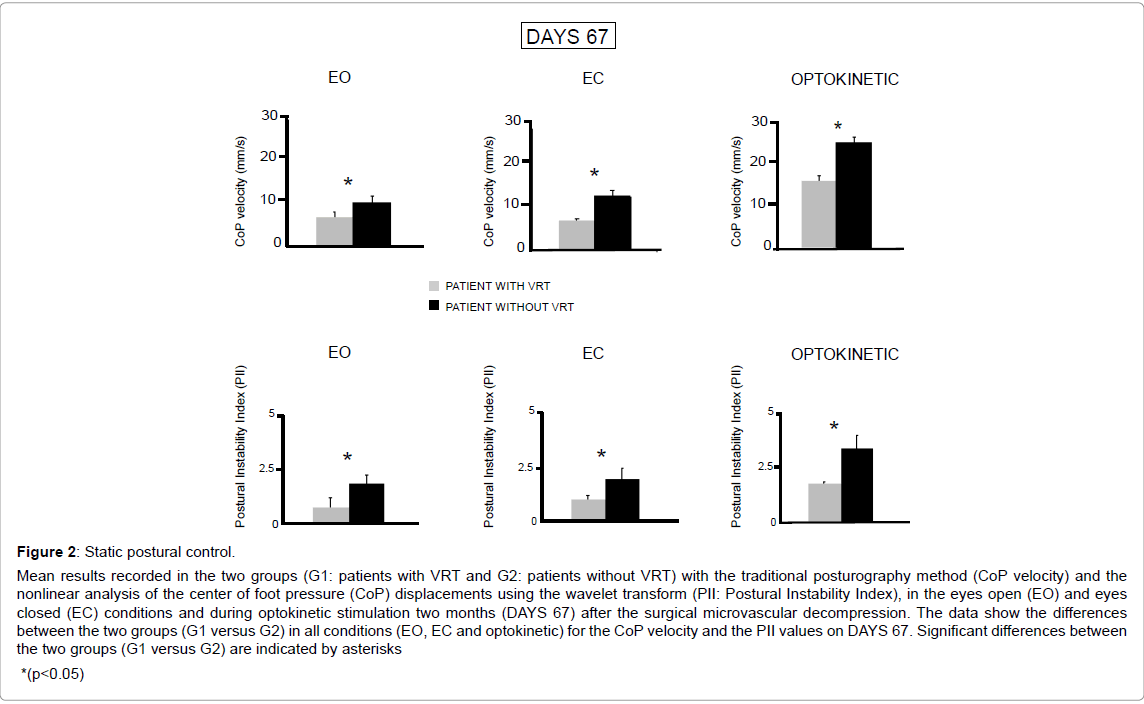
By contrast, the results demonstrated that CoP velocity and the PII values were significantly decreased in all tested conditions (p<0.05) in the G1 group of patients who benefited from the vestibular rehabilitation therapy (Figure 2). Mean CoP velocity on DAYS 67 was 6.97 mm/s, 7.38 mm/s and 16 mm/s with EO, EC and Optokinetic stimulation, respectively, compared to the G2 group of patients without VRT (EO: 10.23 mm/s ; EC: 13.40 mm/s ; Optokinetic : 25 mm/s). The postural performance of the two groups was better in the EO condition (G1: PII=0.71 ± 0.41, G2: PII=1.77 ± 0.40) compared to the EC (G1: PII=0.93 ± 0.07, G2: PII=1.82 ± 0.66) and with optokinetic stimulation conditions (G1: PII=2.06 ± 0.12, G2: PII=3.97 ± 0.65). But in all tested conditions, the postural performance of the G1 group with VRT was significantly better than that of the G2 group (p<0.05). Interestingly, the G1 group postural performances as evaluated by both the CoP velocity and PII values (EO: 0.71 ± 0.41; EC: 0.93 ± 0.07; Optokinetic: 2.06 ± 0.12) did not differ significantly from the normative data recorded in healthy controls of the same group of age (EO: 0.94 ± 0.60; EC: 1.13 ± 0.57; Optokinetic: 2.14 ± 0.82 [24]).
Figure 2:Static postural control.
Mean results recorded in the two groups (G1: patients with VRT and G2: patients without VRT) with the traditional posturography method (CoP velocity) and the nonlinear analysis of the center of foot pressure (CoP) displacements using the wavelet transform (PII: Postural Instability Index), in the eyes open (EO) and eyes closed (EC) conditions and during optokinetic stimulation two months (DAYS 67) after the surgical microvascular decompression. The data show the differences between the two groups (G1 versus G2) in all conditions (EO, EC and optokinetic) for the CoP velocity and the PII values on DAYS 67. Significant differences between the two groups (G1 versus G2) are indicated by asterisks *(p<0.05).
Intragroup comparison
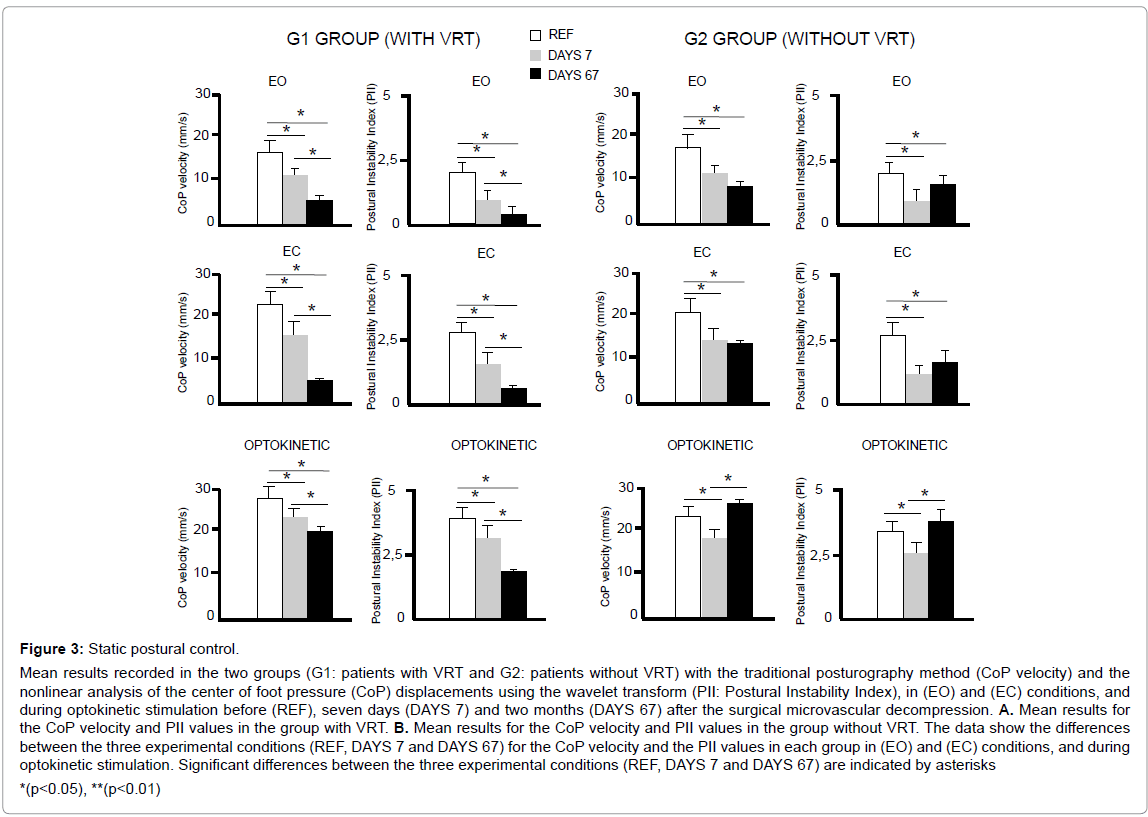
After repetitive postural evaluation with the surgical microvascular decompression and the vestibular rehabilitation therapy (VRT), G1 group showed changes in static postural control (Figure 3). The mean CoP velocity and PII values decreased on DAYS 7 after the surgical microvascular decompression and on DAYS 67 after the VRT in all tested conditions (EO, EC, Optokinetic). As shown in the bar charts of Figure 3, this feature is confirmed by the statistical tests since a modification is noticed for the CoP velocity (p<0.05) and for the PII values (p<0.05) on DAYS 7 and DAYS 67 relative to the REF condition. A significant decrease (p<0.05) is also observed for both the variables in (EO) and (EC) conditions and during optokinetic stimulation between seven days and two months after the VRT. Indeed, relative to the REF condition, the percentages of decrease of the CoP velocity and the PII values on DAYS 7 and DAYS 67 are illustrated in all tested conditions (EO, EC, Optokinetic) in the Table 1.
Figure 3:Static postural control.
Mean results recorded in the two groups (G1: patients with VRT and G2: patients without VRT) with the traditional posturography method (CoP velocity) and the nonlinear analysis of the center of foot pressure (CoP) displacements using the wavelet transform (PII: Postural Instability Index), in (EO) and (EC) conditions, and during optokinetic stimulation before (REF), seven days (DAYS 7) and two months (DAYS 67) after the surgical microvascular decompression. A. Mean results for the CoP velocity and PII values in the group with VRT. B. Mean results for the CoP velocity and PII values in the group without VRT. The data show the differences between the three experimental conditions (REF, DAYS 7 and DAYS 67) for the CoP velocity and the PII values in each group in (EO) and (EC) conditions, and during optokinetic stimulation. Significant differences between the three experimental conditions (REF, DAYS 7 and DAYS 67) are indicated by asterisks *(p<0.05), **(p<0.01)
| G1 GROUP (WITH VRT) | G2 GROUP (WITHOUT VRT) | |||||||
|---|---|---|---|---|---|---|---|---|
| CoP velocity (%) | PII (%) | CoP velocity (%) | PII (%) | |||||
| DAYS 7 | DAYS 67 | DAYS 7 | DAYS 67 | DAYS 7 | DAYS 67 | DAYS 7 | DAYS 67 | |
| EO | -32 | -59 | -38 | -66 | -29 | -41 | -39 | -15 |
| EC | -30 | -67 | -44 | -66 | -35 | -33 | -47 | -39 |
| OPTO | -26 | -26 | -26 | -51 | -38 | +7 | 33 | +3 |
Table 1: Percentages of decrease (-) or increase (+) of the CoP velocity and the PII values on DAYS 7 and DAYS 67 (relative to the REF condition) in the two groups (G1: patients with VRT and G2: patients without VRT) in (EO) and (EC) conditions and during optokinetic stimulation.
As indicated by the bar charts of Figure 3, significant effects are also observed for the G2 group without VRT. The mean CoP velocity and PII values decreased on DAYS 7 (p<0.05) and on DAYS 67 (p<0.05) after the surgical microvascular decompression in (EO) and (EC) conditions. In addition, the statistical test reveals a) decreases for the CoP velocity and the PII values on DAYS 7 (p<0.05) during optokinetic stimulation but b) conversely increases for both the variables on DAYS 67 (p<0.05) in the same condition. Indeed, relative to the REF condition, all the percentages of decrease or increase of the CoP velocity and the PII values on DAYS 7 and DAYS 67 are illustrated in (EO) and (EC) conditions and during optokinetic stimulation in the Table 1.
Dynamic postural control intergroup comparison
In dynamic condition, the two groups had the same postural performance with eyes open and eyes closed and with optokinetic stimulation before and seven days (DAYS 7) after the surgery.
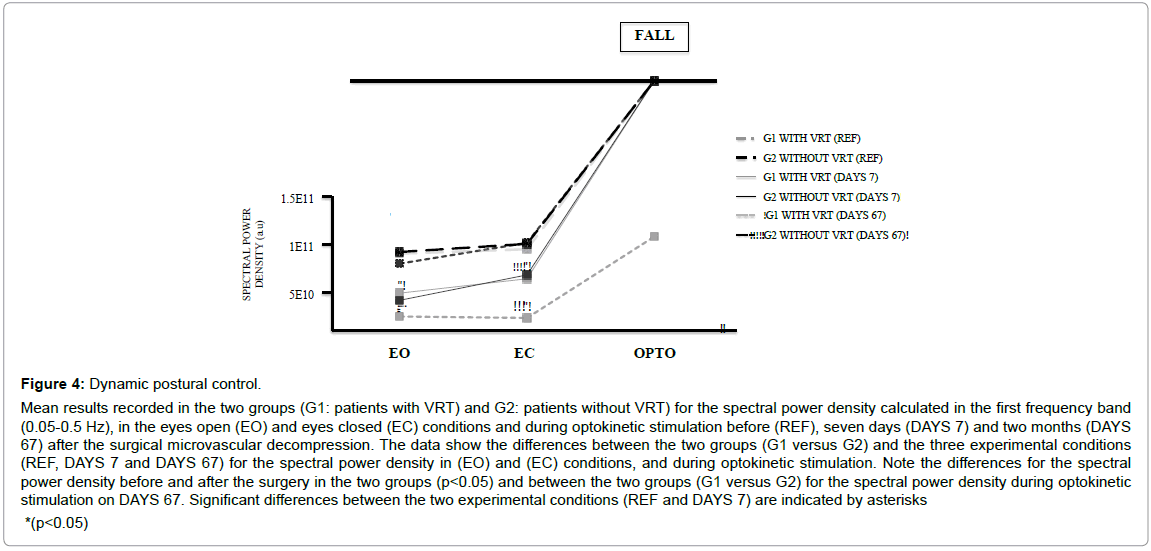
By contrast, G1 group of patients who benefited from VRT showed an improvement of dynamic postural balance compared to G2 group of patients without VRT in EO and EC conditions on DAYS 67 (Figure 4). The spectral power density values recorded in the first frequency band (0.05-0.5 Hz) were significantly lower in the G1 group with eyes open (2.00 × 109 a.u) and eyes closed (5.70 × 107 a.u) than in G2 group (EO: 6.88 × 1010 a.u; EC: 9.53 × 1010 a.u).
Maintaining balance on an unstable platform with optokinetic stimulation was impossible on DAYS 67 for patients without VRT, but the G1 group with VRT succeeded in this task.
Intragroup comparison
After repetitive postural evaluation with the surgical microvascular decompression and the vestibular rehabilitation therapy (VRT), the G1 group showed changes in dynamic postural control (Figure 4). The spectral power density decreased on DAYS 7 after the surgical microvascular decompression and on DAYS 67 after the VRT in (EO) and (EC) conditions. As shown in the Figure 4, this feature is confirmed by the statistical tests since a modification is noticed for the spectral power density on DAYS 7 and DAYS 67 (p<0.05) relative to the REF condition. A significant decrease (p<0.05) is also observed between seven days and two months after the VRT. Maintaining balance on an unstable platform with optokinetic stimulation was impossible before and on DAYS 7 after the surgery, but the patients succeeded in this task on DAYS 67.
By contrast, the G2 group of patients without VRT showed no improvement of dynamic postural balance in EO and EC conditions on DAYS 67 relative to the REF condition (Figure 4). Nevertheless, a significant decrease is observed for the spectral power density on DAYS 7 (p<0.05) after the surgery. As indicated by the Figure 4, maintaining balance on an unstable platform with optokinetic stimulation was impossible before, on DAYS 7 and DAYS 67 after the surgery.
Figure 4:Dynamic postural control. Mean results recorded in the two groups (G1: patients with VRT) and G2: patients without VRT) for the spectral power density calculated in the first frequency band (0.05-0.5 Hz), in the eyes open (EO) and eyes closed (EC) conditions and during optokinetic stimulation before (REF), seven days (DAYS 7) and two months (DAYS 67) after the surgical microvascular decompression. The data show the differences between the two groups (G1 versus G2) and the three experimental conditions (REF, DAYS 7 and DAYS 67) for the spectral power density in (EO) and (EC) conditions, and during optokinetic stimulation. Note the differences for the spectral power density before and after the surgery in the two groups (p<0.05) and between the two groups (G1 versus G2) for the spectral power density during optokinetic stimulation on DAYS 67. Significant differences between the two experimental conditions (REF and DAYS 7) are indicated by asterisks *(p<0.05)
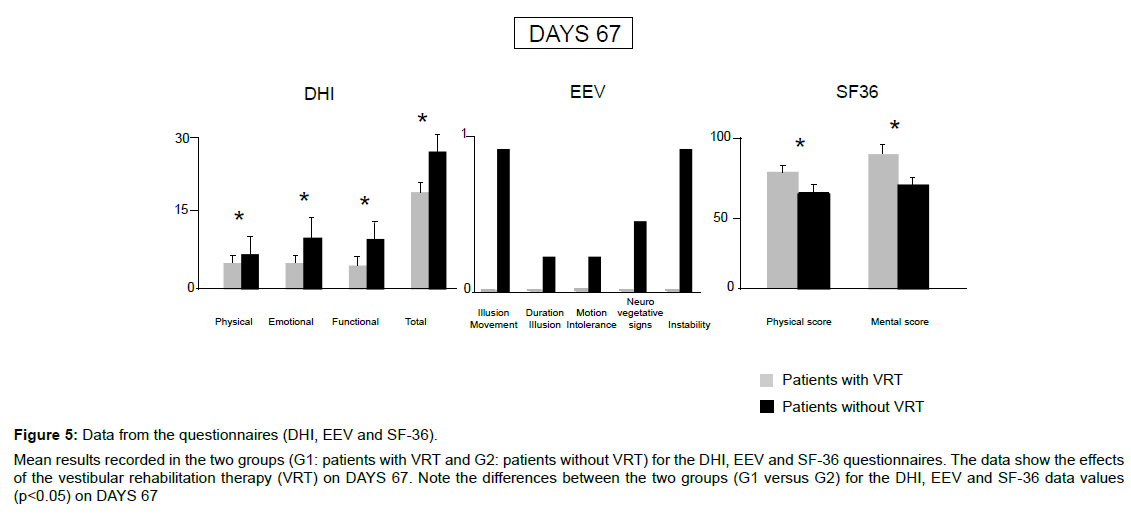
Data from the questionnaires (DHI, EEV and SF-36) on DAYS 67
The statistical test performed on the three questionnaires showed significant differences between the two groups on DAYS 67. The DHI (Physical, Emotional, Functional and Total scores) and EEV data values were significant higher (p<0.05) in patients without VRT than in patients with VRT (Figure 5).
Figure 5:Data from the questionnaires (DHI, EEV and SF-36). Mean results recorded in the two groups (G1: patients with VRT and G2: patients without VRT) for the DHI, EEV and SF-36 questionnaires. The data show the effects of the vestibular rehabilitation therapy (VRT) on DAYS 67. Note the differences between the two groups (G1 versus G2) for the DHI, EEV and SF-36 data values (p<0.05) on DAYS 67.
Although the quality of life (SF-36) was better (p<0.05) in patients who benefited from the VRT (Physical: 77.4 ± 3.75, Mental: 89.0 ± 5.06) compared to the patients without VRT (Physical: 63.5 ± 4.71, Mental: 68.9 ± 3.60), it must be mentioned that the mental and physical scores of the quality of life (SF-36) in patients with VRT were not to 100% on DAYS 67. These patients still complain of some minor problems in their day life.
Discussion
Effect of vestibular rehabilitation therapy on static postural control
Several studies previously demonstrated the benefit of vestibular rehabilitation therapy on the postural control in vestibular loss patients [28,29]. The recent Cochran database of systematic reviews [18,19] have concluded that the vestibular rehabilitation therapy is a safe, effective management for patients with unilateral peripheral vestibular dysfunction and that it helps to resolve symptoms like dizziness and balance impairment. This work is the first to have investigated the effectiveness of the VRT on the static and dynamic postural control and on the quality of life in patients after a surgical microvascular decompression of the cochleo-vestibular nerve. The postural performance of the patients with VRT recorded before and seven days after the surgical microvascular decompression of the cochleo-vestibular nerve was the same than that of the patients without VRT in all tested conditions. The microvascular conflict is responsible for the related fluctuation of symptoms but the surgical microvascular decompression allows treating the electrical short circuits at the periphery nerve level in such intermittent pathology. Consequently, the observed vestibular disorders and dizziness are not intermittent but stable after the surgery and would explain that the vestibular rehabilitation therapy improves the natural spontaneous vestibular compensation and helps the recovery of balance function. Indeed, the postural performance of those patients was significantly improved after VRT compared to those patients without VRT. The Postural Instability Index values and the body sway velocity were decreased in all tested conditions. These data clearly showed that the patients with VRT had a better postural performance than the patients without VRT and this best recovery was associated to a better quality of life. Interestingly, the patients with VRT have the same postural performance than that of healthy controls of the same group of age.
Although the performance of the patients with VRT was better in all tested condition compared to those without VRT, these latter patients also improved spontaneously their postural performance two months later after the surgery (DAYS 67) with and without vision, but significantly less. And finally, the most interesting result showed that the poor static postural control under optokinetic stimulation in these patients without VRT could be due to a strong dependence on the visual motion cues, not cured by a proper rehabilitation.
Effect of vestibular rehabilitation therapy on dynamic postural control
Before and seven days after the surgery, the patients with VRT showed the same dynamic postural performance than that of patients without VRT. The spectral power density values were decreased with and without vision seven days after the surgery in the two groups, compared to the reference condition (before). These data clearly indicate that their postural performance was improved as a result of vascular decompression. While all patients maintained their balance on an unstable platform with and without vision, they were all unable to succeed the postural task with optokinetic stimulation before and seven days after the surgery. All the patients fell in this condition.
By contrast, the VRT have induced a powerful beneficial effect on the dynamic postural control when evaluated two months later (DAYS 67). The patients with VRT spent less energy to maintain their equilibrium with and without vision, compared to patients without VRT. The spectral power density values recorded in the first (0.05-0.5 Hz) frequency band were significantly lower in patients with VRT in the eyes open (2.00 × 109 a.u) and eyes closed (5.70 × 107 a.u) conditions than in patients without VRT (6.88 × 1010 a.u. and 9.53 × 1010 a.u., respectively). Two months after the VRT, the patients were able to maintain their balance during optokinetic stimulation (a postural performance they were unable to do seven days after the surgery), while the patients without VRT still fell in this condition. It is well known that training with optokinetic stimulation can help the recovery of balance function in patients with vestibular deficits. Earlier studies in individuals with a unilateral or bilateral peripheral vestibular disorder showed significant improvements in both postural stability and optokinetic nystagmus after 6 weeks of exposure to optokinetic stimulation [30,31]. The vestibular rehabilitation program the patients were submitted to is very likely responsible for this strong improvement of their dynamic balance performance two months after surgical microvascular decompression of the cochleo-vestibular nerve. In accordance with the study of Pavlou [32], VRT incorporating optokinetic stimuli is very helpful to improve dizziness and postural instability, particularly in patients with visual dependency. The poor dynamic postural control under optokinetic stimulation in the patients without VRT could be due to a strong dependence on the visual motion cues, not cured by a proper rehabilitation.
Effect of vestibular rehabilitation therapy on the perception of the vertigo, dizziness and on the quality of life
One of the main results is that the VRT improves the vertigo, the dizziness and the quality of life in patients after a surgical microvascular decompression of the cochleo-vestibular nerve. Several authors [33,34] had already observed a significant improvement in the quality of life (assessed with the DHI test) after a vestibular rehabilitation protocol, in patients with vestibular chronic vestibular dysfunction, exhibiting dizziness and imbalance, independent of age and gender. The inclusion of visual stimuli made of digital images on vestibular and body balance rehabilitation was found effective to reduce dizziness and improve quality of life in patients with peripheral vestibular disorders [35]. And finally, vestibular exercises have also beneficial effects in patients with acute vertigo [36].
Despite the fact that the quality of life was also significantly better in the patients who benefited from the VRT compared to the patients without VRT, the mental and the physical scores were not to 100% after the VRT. The patients with VRT still complained of mild physical limitation and decreased vitality. An evaluation performed at a later stage and/or a prolonged VRT, should be necessary to assess the return to an optimal quality of life. This result shows also that in spite of a good behavioural recovery as measured by the objective post-urography tests, there is not a close correlation with the subjective evaluations made by the patients themselves.
Conclusion
This pilot study is the first to show that VRT improves significantly the postural control and the quality of life as well after microvascular decompression of the cochleo-vestibular nerve. It extends to this pathology the general statement that VRT interacts with the recovery mechanisms involved after a vestibular loss [20,36]. The benefits of VRT after decompression surgery may help to avoid falls (a crucial problem in old people) and to promote independent living in patients. However, this conclusion must be confirmed on a larger group of patients.
References
- Yap L, Pothula VB, Lesser T (2008) Microvascular decompression of cochleovestibular nerve. Eur Arch Otorhinolaryngol 265: 861-869.
- Hüfner k, Barresi M, Glaser M, Linn J, Adrion C, et al. (2008) Vestibular paroxysmia: Diagnostic features and medical treatment. Neurology 71: 1006-1014.
- Brandt T, Strupp M, Dieterich M (2016) Vestibular paroxysmia, a treatable neurovascular cross-compression syndrome. J Neurol 1: S90- S96.
- Bernard-Demanze L, Lacour M (2016) The fall in older adults: Physical and cognitive problems. Curr Aging Sci 10: 185-200.
- Zhang L, Yu Y, Yuan Y, Xu J, Xu X, et al. (2012) Microvascular decompression of cochleovestibular nerve in patients with tinnitus and vertigo. Neurol India 60: 495-497.
- Chays A, Labrousse M, Bazin A, Pierot L, Rousseaux P (2010) Vasculo-neural compression syndromes in the ponto-cerebellar angle. Surgical treatment. E-mémoires de l’Académie Nationale de Chirurgie 9: 95-99.
- De Abreu Junior L, Kuniyoshi CH, Wolosker AB, Borri ML, Antunes A et al. (2016) Vascular loops in the anterio inferior cerebellar artery, as identified by magnetic resonance imaging and their relationship with otologic symptoms. Radiol Bras 49: 300-304.
- Brandt T, Dieterich M (1994) VIIIth nerve vascular compression syndrome: Vestibular paroxysmia. Baillieres Clin Neurol 3: 565-575.
- Strupp M, von Stuckrad-Barre S, Brandt T, Tonn JC (2013) Teaching neuroimages: Compression of the eighth cranial nerve causes vestibular paroxysmia. Neurology 80: e77.
- Best C, Gawehn J, Krämer HH, Thomke F, Ibis T et al. (2013) MRI and neurophysiology in vestibular paroxysmia: Contradiction and correlation. J Neurol Neurosurg Psychiatry 84: 1349-1356.
- Brandt T, Dieterich M (1994) Vestibular paroxysmia: Vascular compression of the eighth nerve? Lancet 343: 798-799.
- Guevara N, Devèze A, Buza V, Laffont B, Magnan J (2008) Microvascular decompression of cochlear nerve for tinnitus incapacity: Pre-surgical data, surgical analyses and long-term follow-up of 15 patients. Eur Arch Otorhinolaryngol 265: 397-401.
- Moller MB, Moller AR, Jannetta PJ, Jho HD (1993) Vascular decompression surgery for severe tinnitus: Selection criteria and results. Laryngoscope 103: 421-427.
- Moller MB (1997) Selection criteria and treatment of patients with disabling positional vertigo. Stereotact Funct Neurosurg 68: 270-273.
- Okamura T, Kurokawa Y, Ikeda N, Abiko S, Ideguchi M, et al. (2000) Microvascular decompression for cochlear symptoms. J Neurosurg 93: 421-426.
- Brackmann DE, Kesser BW, Day JD (2001) Microvascular decompression of the cochleovestibular nerve for disabling positional vertigo: The House Ear Clinic Experience. Otol Neurotol 22: 882-887.
- Miyazaki H, Devèze A, Magnan J (2005) Neuro-otologic surgery through minimally invasive retrosigmoid approach: Endoscope assisted microvascular decompression, vestibular neurotomie and tumor removal. Laryngoscope 115: 1612-1617.
- McDonnell MN, Hillier SL, Miles TS, Thompson PD, Ridding MC (2007) Influence of combined afferent stimulation and task-specific training following stroke: A pilot randomized controlled trial. Epub 21: 435-443.
- Hillier SL, McDonnell M (2011) Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev 2: CD005397.
- Lacour M, Bernard-Demanze L (2015) Interaction between vestibular compensation mechanisms and vestibular rehabilitation therapy: 10 recommendations for optimal functional recovery. Front Neurol 5: 285.
- Tardieu C, Dumitrescu M, Giraudeau A, Blanc JL, Cheynet F, et al. (2009) Dental occlusion and postural control in adults. Neurosci Lett 450: 221-224.
- Pavlou M, Bronstein AM, Davies RA (2004) Randomized trial of supervised versus unsupervises optokinetic exercise in persons with peripheral vestibular disorders. Neurorehabil Neural Repair 27: 208-218.
- Lacour M, Bernard-Demanze L, Dumitrescu M (2008) Posture control, aging and attention resources: Models and posture-analysis methods. Neurophysiol Clin 36: 411-421.
- Bernard-Demanze L, Dumitrescu M, Jimeno P, Borel L, Lacour M (2009) Age-related changes in posture control are differentially affected by postural and cognitive complexity. Curr Aging Sci 2: 139-149.
- Jacobson GP, Newman CW (1990) The development of the dizziness handicap inventory. Arch Otolaryngol Head Neck Surg 116: 424-427.
- Mègnigbêto CA, Sauvage JP, Launois R (2001) The European Evaluation of Vertigo (EEV) scale: A clinical validation study. Rev Laryngol Otol Rhinol (Bord) 122: 95-102.
- John E, Ware Jr (1996) The SF-36 Health Survey. In: Spilker B (Eds.) Quality of life and pharmacoeconomics in clinical trials. Second edition. Philadelphia: Lippincott-Raven Publishers, pp: 337-345.
- Han BI, Song HS, Kim JS (2011) Vestibular rehabilitation therapy: Review of indications, mechanisms and key exercises. J Clin Neurol 7: 184-196.
- McDonnell MN, Hillier SL (2015) Vestibular rehabilitation for unilateral peripheral vestibular dysfunction. Cochrane Database Syst Rev 1: CD005397.
- Vitte E, Sémont A, Berthoz A (1994) Repeated optokinetic stimulation in conditions of active standing facilitates recovery from vestibular deficits. Exp Brain Res 102: 141-148.
- Tsuzuku T, Vitte E, Sémont A, Berthoz A (1995) Modification of parameters in vertical optokinetic nystagmus after repeated vertical optokinetic stimulation in patients with vestibular lesions. Acta Otolaryngol Suppl 2: 419-422.
- Pavlou M (2010) The use of optokinetic in vestibular rehabilitation. J Neurol Phy Ther 34: 105-110.
- Foster CA (1994) Vestibular rehabilitation. Baillieres Clin Neurol 3: 577-592.
- Patatas OH, Ganança CF, Ganança FF (2009) Quality of life of individuals submitted to vestibular rehabilitation. Braz J Otorhinolaryngol 75: 387-394.
- Manso A, Ganança MM, Caovilla HH (2016) Vestibular rehabilitation with visual stimuli in peripheral vestibular disorders. Braz J Otorhinolaryngol 82: 232-241.
- Venosa AR, Bittar RS (2007) Vestibular rehabilitation exercises in acute vertigo. Laryngoscope 117: 1482-1487.
Citation: Bernard-Demanze L, Montava M, Mattei A, Lavieille JP, Lacour M (2017) Effects of Vestibular Rehabilitation Therapy on Postural Control and Quality of Life in Patients after a Surgical Microvascular Decompression of the Cochleo-Vestibular Nerve. Otolaryngol (Sunnyvale) 7:318. DOI: 10.4172/2161-119X.1000318
Copyright: © 2017 Bernard-Demanze L, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4030
- [From(publication date): 0-2017 - Jul 01, 2025]
- Breakdown by view type
- HTML page views: 3146
- PDF downloads: 884