Case Report Open Access
First Case of Liver Abscess with Endogenous Endophthalmitis due toNon- K1/K2 Serotype Hypermucoviscous Klebsiella pneumoniae Clone ST268
Yuji Hirai1,3, Sayaka Asahata-Tago1, Yusuke Ainoda1, Takahiro Fujita3, Yutaka Uzawa1, Kaori Yamamoto2, Tomohiro Iida2 and Ken Kikuchi1*1Department of Infectious Diseases, Tokyo Women’s Medical University, Tokyo, Japan
2Department of Ophthalmology, Tokyo Women’s Medical University, Tokyo, Japan
3Faculty of Medicine, Department of General Medicine, Juntendo University, Tokyo, Japan
- *Corresponding Author:
- Ken Kikuchi, M.D. Ph.D.
Department of Infectious Diseases
Tokyo Women’s Medical University
8-1 Kawada-cho
Shinjuku-ku, Tokyo 162-8666, Japan
Tel: +81-3-3813-3111
Fax: +81-3-5684-7830
E-mail: kikuchi.ken@twmu.ac.jp
Received date: December 9, 2015; Accepted date: January 22, 2016; Published date: January 29, 2016
Citation: Hirai Y, Asahata-Tago S, Ainoda Y, Fujita T, Uzawa Y, et al. (2016) First Case of Liver Abscess with Endogenous Endophthalmitis due toNon-K1/K2 Serotype Hypermucoviscous Klebsiella pneumoniae Clone ST268. J Gastrointest Dig Syst 6:383. doi:10.4172/2161-069X.1000383
Copyright: © 2016 Hirai Y, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
The hypermucoviscous (hv) Klebsiella pneumoniae (KP) can cause invasive liver abscess syndrome (ILAS) including endophthalmitis dominantly in eastern Asia. We report a 80-years old woman who diagnosed with invasive liver abscess syndrome due to K. pneumoniae (KP) non-K1/K2 hvKP multi-locus sequence type ST268 by DNA amplification methods isolated from blood culture. Soon she developed endogenous endopththalmitis and immediately right vitrectomy was performed. Although intravenous 2g of ceftriaxone (CTRX) was administrated, total enucleation of right eyeball had performed due to orbital cellulitis and necrosis of eye ball finally. To find complication (i.e. endophthalmitis) with caution and to select antimicrobial agents with sufficient penetration to CNS (i.e. ceftriaxone) is needed in a patient with severe hvKP infection. Usually ILAS is caused by K1/K2 hvKP. However, to our knowledge, this is a first report of ILAS with endophthalmitis and orbital cellulitis due to non-K1/K2 hvKP ST268.
Keywords
Klebsiella pneumonia; Hypermucoviscous type; Invasive liver abscess syndrome; Endogenous endophthalmitis; Non-K1/K2 serotype; Sequence type 268
Introduction
Dominant in Asia, the hypermucoviscous (hv) Klebsiella pneumoniae (KP) cause invasive liver abscess syndrome (ILAS) complicated with endophthalmitis, and meningitis [1]. The serotype K1 or K2 hvKP can cause such fatal infection in common, however only a few cases caused by non-K1/K2 hvKP were reported [2]. We report a first case of ILAS complicated with endophthalmitis caused by non-K1/K2 serotype KP clone ST268.
Case
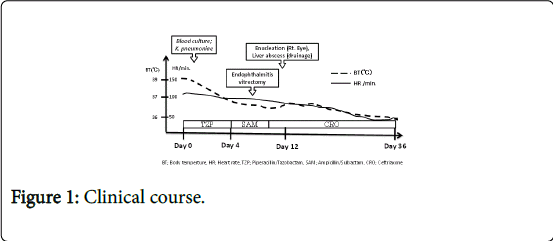
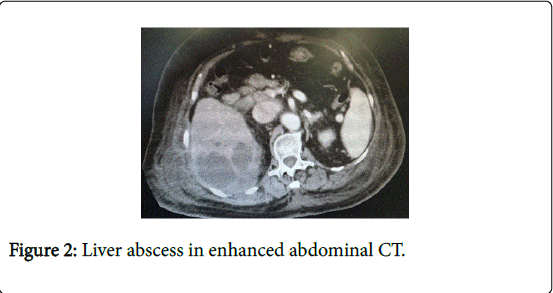
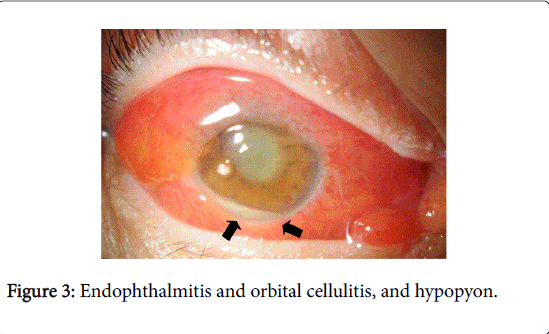
A 80-years old woman, who had pancreatico-duodenectomy due to Vater’s papilla cancer, was admitted due to sepsis (pulse 100 beats per minute, blood pressure 125/66 mmHg, respiratory rate 22 breaths per minute, Body temperature 39.3). She has dementia and resided in a nursing home. No travel history to abroad for two decades was available. She was diagnosed with cholangitis and was administrated intravenous piperacillin/tazobantam (PIPC/TAZ) initially. Blood count showed hemoglobin of 9.1 g/dL, white cell count of 9.6 × 103/μL, and platelet count of 770 × 103/μL. No abnormality was found in plain abdominal CT scan at admission. Two sets of blood culture taken at admission were positive for K. pneumoniae (KP) and 9 g of ampicillin/ sulbactam (ABPC/SBT) was administrated according to susceptibility test. On day 4, she presented right ocular hyperemia and swelling around her right eye. On day 12, right hypopyon was found significantly. She was diagnosed with endogenous endopththalmitis and immediately right vitrectomy was performed (Figure 1). Intravenous 2g of ceftriaxone (CTRX) was administrated immediately. However orbital cellulitis and necrosis of eye ball had been getting worse, total enucleation of right eyeball had performed and artificial eyeball was installed into her right orbital space on day 14. As a same time, enhanced abdominal CT scan revealed liver abscess (Figure 2). Liver drainage had performed. Vitreous culture was also positive for KP. Duration of antimicrobial therapies was 32 days. Although she was recovered and transferred to other hospital for rehabilitation, she was right-sided blindness caused by endophthalmitis (Figure 3).
Blood samples were drawn under sterile conditions and processed using BacT/Alert 3D (bioMe´rieux, Marcy l'Etoile, FRANCE).ã??The strain was identified as KP by Vitek2 (bioMe´rieux). The KP was positive for string test (>5 mm), which was confirmed to hypermucoviscous (hv) type ã??phenotypically. Antimicrobial susceptibility performed with the broth microdilution method according to the Clinical and Laboratory Standards Institute guidelines was shown in Table 1.
| Ampicillin | Piperacillin | Cefazolin | Cefotiam | Cefmetazole | Cefoxitin | SBT/CPZ | IPM/CS | LVFX | GM | ST | |
| MIC | >16 | <8 | <4 | <8 | <4 | <8 | <16 | <1 | <1 | <1 | <2 |
| String test | Serotype | Sequence Type | magA | wzy- | aerobactine gene | allS | kfu | rmpA | rmpA2 | c-rmpA | |
| Result | 12mm (positive) | non-K1/K2 | 268 | - | - | + | - | - | + | + | + |
Table 1: Antimicrobial susceptibility and phenotype/genotype testing for hypermucoviscous Klebsiella pneumoniae (hvKP).
No antimicrobial resistant exclude ampicillin was found. Multilocus sequence typing (MLST) performed according to the protocol described on the KP MLST website (http://www.pasteur.fr/recherche/ genopole/PF8/mlst/Kpneumoniae.html). MLST revealed that the isolates were of the sequence type (ST) 268.
The capsular serotype was not detectable using Klebsiella antisera Seiken (Denka Seiken, Tokyo, Japan). The K serotype-specific alleles at mag A (K1) and wzy (K2) loci, which are located in the capsular polysaccharide synthesis gene cluster, were not detectable by amplified capsular polysaccharide synthesis genotyping PCR analysis [1].
In this case, KP was demonstrated to be capsular serotype non- K1/K2. The presence of the virulence genes (rmpA+, rmpA2+, chromosomal-rmpA -, mag A-, wzy -, alls -, kfu -, aerobactin gene+, iutA+, silS+, terW+, repA+, and fimH+) was screened by PCR analysis by using relevant primers [3-5].
Discussion
To our knowledge, this is the first case report of ILAS due to non- K1/K2 serotype hvKP ST268 complicated with endophthalmitis and orbital celluritis. The KP ST268, which was originally isolated from Korea in 2008, was identified four strains from nasal, throat on the KP MLST website. Korean CDC reported that 7% out of 74 strains of K. pneumoniae which caused community acquired pneumonia was identified as ST268 [6]. In addition, ESBL-producing KP ST268 isolated from clinical settings was reported from Korea [7]. The KP ST268 strains may exist dominantly in eastern Asia including Korea and Japan. However hvKP ST268 had not been reported, except recent case, previously all over the world.
In this strain, although string test showed 12mm (>5mm) to confirm hv type phenotypically, but serotype K1/K2 was not determined. However rmpA and rmpA 2 which has been confirmed as a gene that regulates capsular polysaccharide synthesis was detected. Wen-Liang Yu et al reported that twelve out of 14 strains of non-K1/K2 KP which caused liver abscess expressed rmpA gene [8]. Non-K1/K2 isolates that express rmpA and aerobactin genes show a similar virulence to serotype K1/K2 KP isolates from patients with liver abscesses [8]. The identified non-K1/K2 genotypes (K5, K20, K54, and K57) of liver abscess strains were generally in accordance with a recent series from northern Taiwan [2].
The ILAS, which is known to be frequently occurred in Asia, is categorized as liver abscess complicated with endophthalmitis, and/or meningitis due to hvKP. Diabetes mellitus (29-63%), hepatobilliary disease (18-25%) were the frequently underlying disorders [1]. Although Siu et al mentioned the causable strains are limited to K1/K2 serotype hvKP [1], however non-K1/K2 serotype hvKP can also cause severe infection. According to previous report [8], we also consider that positive for any rmp gene is independent virulence factor for hvKP. For clinical settings, positive string test (>5mm) is rapid and convenient presumable method for hvKP phenotypically [1]. Although most of all hvKP strains were susceptible to first or third generation cephalospolins, ESBL-producing hvKP was reported from Taiwan [9,10] and expansion of extensively drug-resistant (QnrS1-, CTX-M- 2-, and KPC-2)-producing hvKP was reported in a tertiary-care university hospital in Brazil [11]. Multi-drug resistant with hypervirulent hvKP is already emerged.
Previous report suggested that two-thirds of complications (i.e. endophthalmitis, liver abscess) were undetectable at admission [12]. Epidemiological data of ILAS cases suggested that approximately 65% of cases had right-sided hepatic lobe liver abscess [2]. Endphthalmitis is frequently common complication in ILAS (4-11%) [1,13], and hvKP bacteremia (4.8%) [13,14]. Frequently of bilateral endophthalmitis (13-25%) had been reported [13]. Notably, the hvKP is already known, as a clinical consensus, the frequent pathogen of endophthalmitis due to Gram-Negative Strains dominantly in Asia [15]. ILAS caused by hvKP led to 4-8% of mortality regardless of appropriate antibiotic therapy [1]. However, according to recent case, high incidence (>85%) of visual disturbance was caused by endophthalmitis [2].
In this case, the patient, who had dementia with deliria due to sepsis, had hardly complaint impairment vision. The delayed diagnosis of endophthalmitis might be depending on patient's status and awareness of pathological condition for clinicians. The conjunctival congestion following bacteremia may be clinical cue for making diagnosis of endophthalmitis and orbital cellulitis to reassess its therapeutic management, and consult to ophthalmologist immediately.
The carriage rate of all KP in stool from healthy human were varied (10-19% in Europe [1], 75% in China) and 23% of healthy human carried serotype K1/K2 KP in Taiwan [16]. Thus geographical distribution may be available in carriage rate. Similar to typhoid fever, human to human transmission of serotype K1 hvKP in the family (a male infected patient to his son, daughter, and wife) as confirmed by PFGE in Japan [17]. In Asia, complications (i.e. liver abscess, meningitis, endophthalmitis) caused by KP bacteremia, whether serotype is K1/K2 or not, should be identified with caution during the clinical course. Antimicrobial agents with sufficient penetration to CSF or eye, such as 3rd generation cephalosporin (i.e. ceftriaxone), should be used immediately if hvKP is suspected as causable pathogen. Surgical intervention such as drainage is also needed.
At this time, many cases of severe infection caused by hvKP have also been reported from Europe and United States of America. To reflect globalization, the number of severe hvKP infections may be increasing all over the world even now.
In conclusion, we report the first case of ILAS with endophthalmitis and orbital cellulitis due to non-K1/K2 hvKP ST268. Clinicians and microbiologists should alert and share information about invasive and disseminate severe infection caused by hvKP regardless of its serotype, and geographic area.
Acknowledgement
The authors declare that there is no conflict of interest regarding the publication of this paper. We thanked Tsuruoka N, and Goto A, Clinical Laboratory, Tokyo Women’s Medical University Hospital, for culturing clinical KP strains.
References
- Kristopher Siu L, Yeh KM, Lin JC, Fung CP, Chang FY (2012) Klebsiella pneumoniae liver abscess: a new invasive syndrome. Lancet Infect Dis 12: 881–887.
- Fang CT, Chuang YP, Shun CT, Hsueh PR, Liu KL, et al. (2007)Klebsiella pneumoniae genotype K1: an emerging pathogen that causes septic ocular or central nervous system complications from pyogenic liver abscess. Clin Infect Dis 45: 284-293.
- Luo Y, Wang Y, Ye L, Yang J (2014) Molecular epidemiology and virulence factors of pyogenic liver abscess causing Klebsiella pneumoniae in China. Clin Microbiol Infect 20: O818-824.
- Yu WL, Ko WC, Cheng KC, Lee HC, Ke DS, et al. (2006) Association between rmpA and magA genes and clinical syndromes caused by Klebsiella pneumoniae in Taiwan. Clin Infect Dis 42: 1351-1358.
- Hsu CR, Lin TL, Chen YC, Chou HC, Wang JT (2011) The role of Klebsiella pneumoniae rmpA in capsular polysaccharide synthesis and virulence revisited. Microbiology 157: 3446-3457.
- Sangun J (2012) Centers for Disease Control and Prevention National Health Research Institute Tuberculosis Center respiratory infectious bacteria. Multilocus sequence typing analysis of Klebsiella pneumoniae strains isolated from patients with community-acquired pneumonia and bronchitis. Weekly-Health and Diseases.
- SooKo K, Young Lee J, Baek JY, YoeunSuh J, Mi Young Lee MY, et al. (2011) Predominance of an ST11 extended-spectrum ß-lactamase-producing Klebsiella pneumoniae clone causing bacteraemia and urinary tract infections in Korea. Journal of Medical Microbiology 59:822–828.
- Yu WL, Ko WC, Cheng KC, Lee CC, Lai CC, et al. (2008) Comparison of prevalence of virulence factors for Klebsiella pneumoniae liver abscesses between isolates with capsular K1/K2 and non-K1/K2 serotypes. Diagn Microbiol Infect Dis 62:1-6.
- Lin JC, Siu LK, Fung CP, Yeh KM, Chang FY (2007) Nosocomial liver abscess caused by extended-spectrum beta-lactamase-producing Klebsiella pneumoniae . J Clin Microbiol 45: 266-269.
- Su SC, Siu LK, Ma L, Yeh KM, Fung CP, et al. (2008) Community-acquired liver abscess caused by serotype K1 Klebsiella pneumoniae with CTX-M-15-type extended-spectrum beta-lactamase. Antimicrob Agents Chemother 52: 804–805.
- Andrade LN, Vitali L, Gaspar GG, Bellissimo-Rodrigues F, Martinez R, et al. (2014) Expansion and evolution of a virulent, extensively drug-resistant (polymyxin B-resistant), QnrS1-, CTX-M-2-, and KPC-2-producing Klebsiella pneumoniae ST11 international high-risk clone. J ClinMicrobiol 52: 2530-2535.
- Lee SS, Chen YS, Tsai HC, Wann SR, Lin HH, et al. (2008) Predictors of septic metastatic infection and mortality among patients with Klebsiella pneumoniae liver abscess. Clin Infect Dis 47: 642-650.
- Yang CS, Tsai HY, Sung CS, Lin KH, Lee FL, et al. (2007) Endogenous Klebsiellaendophthalmitis associated with pyogenic liver abscess. Ophthalmology 114: 876-880.
- Shon AS, Bajwa RP, Russo TA (2013) Hypervirulent (hypermucoviscous) Klebsiella pneumoniae : a new and dangerous breed. Virulence 4: 107-118.
- Durand ML (2013) Endophthalmitis. Clin Microbiol Infect 19: 227-234.
- Lin YT, Siu LK, Lin JC, Chen TL, Tseng CP, et al. (2012) Seroepidemiology of Klebsiella pneumoniae colonizing the intestinal tract of healthy Chinese and overseas Chinese adults in Asian countries. BMC Microbiol 12: 13.
- Harada S, Tateda K, Mitsui H, Hattori Y, Okubo M, et al. (2011) Familial spread of a virulent clone of Klebsiella pneumoniae causing primary liver abscess. J Clin Microbiol 49: 2354-2356.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 11963
- [From(publication date):
February-2016 - Aug 16, 2025] - Breakdown by view type
- HTML page views : 11036
- PDF downloads : 927