Flummoxing Paradox of Pleural Effusion: Contralateral Effusion with Different Cytobiochemical Features Evolving on Anti-tubercular Chemotherapy
Received: 09-Nov-2017 / Accepted Date: 15-Nov-2017 / Published Date: 30-Nov-2017
Abstract
Paradoxical phenomenon is known to occur in cases of tubercolous lymphadenopathy and intracranial tuberculomas during treatment. This is not so common in cases of pleural effusion due to tuberculosis. Case of young immmunocompetent female is described who developed pleural effusion on opposite side within 10 days of anti-tubercular treatment being taken for pleural effusion on one side. Cytobiochemistry of the subsequent fluid was different from the former effusion. Ultimately both resolved on continuation of same treatment.
Keywords: Paradoxical; Pleural effusion; Tuberculosis; Antitubercular chemotherapy
Introduction
Tuberculosis is the most common cause of pleural effusion (PE) in our country. Tuberculous pleurisy is self-limiting and therefore, is considered as an example of protective immunity [1]. Paradoxical response is referred to an unusual expansion of existing lesion or formation of a new lesion during successful anti-tubercular chemotherapy. Paradoxical worsening of the tuberculous lesions has been frequently described to occur weeks or months after the start of anti-tuberculous therapy in the case of lymphadenopathy or intracranial tuberculoma [2-8]. Similarly, paradoxical response has been observed during treatment of pulmonary tuberculosis which can lead to an adult respiratory distress syndrome [9-11]. On the contrary, paradoxical worsening of tuberculous pleural effusion is mentioned only in rare case reports [3].
A case young female is discussed who developed symptomatic right side pleural effusion with ten days of anti-tubercular treatment which she had been taking for pleural effusion on the left side. Moreover pleural fluid characteristics of either side were distinct but finally responded to continuation of same anti tubercular chemotherapy.
Case Presentation
Thirty four year old female presented with right side chest pain associated with fever for last 3 days.
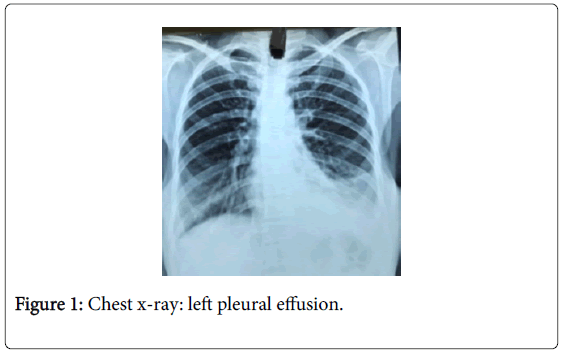
Patient was under treatment of her family physician. She was taking anti tubercular treatment (ATT) for last 10 days for left side pleural effusion detected on chest X-ray (Figure 1) and confirmed by ultrasound thorax. As per records, pleural fluid aspirated before starting ATT was exudate, lymphocytic predominant and with high adenosine deaminase (ADA) level.
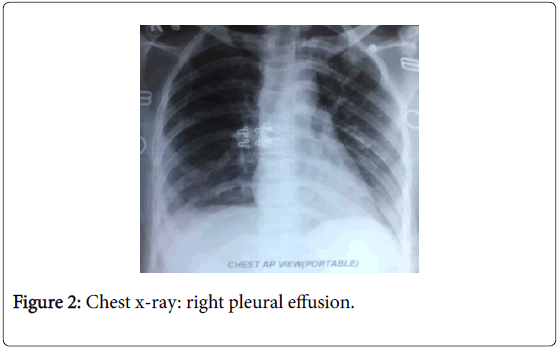
Chest X-ray (Figure 2) was repeated. It was suggestive of pleural effusion on right side. Ultrasound of chest confirmed right side pleural effusion. There was no collection in the left pleural space. Total white cell count was 7400/cc P78L12E1M8B1. Liver and renal biochemistries were normal.
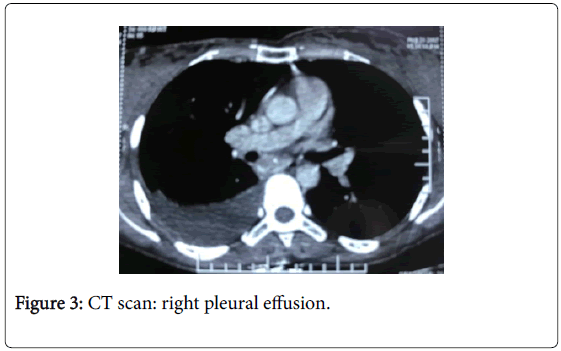
Computerized tomography of thorax (Figure 3) was also consistent with right side pleural effusion without any parenchymal lesion. Pleural aspiration from right side yielded turbid yellow fluid. Cytobiochemical examination revealed exudative fluid, high cell counts with polymorph nuclear predominance and low ADA. Injectable antibiotics were given suspecting empyema as she was running fever (ranging 101-103 F). Culture of pleural fluid yielded no growth.
Patient revealed that she had not been well for last 4 months. Initially she had pain abdomen and loss of appetite associated with mailaise. Ultrasound abdomen at that time revealed some lympnodes. She was treated for enteric fever with antibiotics for ten days. But she continued to have low appetite and general weakness. She managed herself on appetizers and diet supplements. She presented to her family physician this time with side chest pain associated with fever. Investigations, diagnosis and treatment that followed are described above.
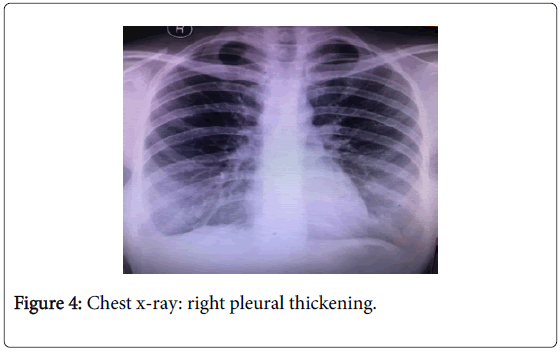
Based on history, other possible causes were speculated. Considering lupus pleuritis and collagen vascular diseases as differential diagnosis, serum antinuclear antibodies (ANA) and rheumatoid factor were requested. Serum ANA and RA factor were reported negative. Subsequently Gene Expert in pleural fluid was positive for Mycobacterium tuberculosis (MTB). She was continued on ATT. Fever subsided followed by chest pain. Follow up chest x-ray after 4 weeks of ATT. Chest x-ray (Figure 4) showed resolution of pleural effusion with mild pleural thickening on right side.
Discussion
Paradoxical events during anti-tuberculous chemotherapy such as persistent fever, newly developing and enlarging lymph nodes, choroid or brain tubercles and even acute respiratory distress syndrome which bears an immunological basis have been reported [2,10]. This response has been rarely reported in cases of pleural effusion. This paradoxical response has been documented to occur 3-4 weeks after the start of ATT [3]. The young female described in the present case developed pleural effusion on the opposite side within 10 days of starting ATT. The evolution of such imminent paradoxical effusion is rare to find in the literature [7].
A large study of 458 patients with pleural tuberculosis found paradoxical response in 16% of the patients. This is far less than 30% paradoxical reaction reported for tubercular lymphadenopathy [4,5]. Majority of the case reports have mentioned worsening on the same side of pleural effusion. In this case however, pleural effusion developed on the opposite side. Contrateral pleural paradox has precedence of very few cases (two cases to my knowledge) in the literature [6,7].
A pleural fluid characteristic of the paradoxical effusion wherever it has been mentioned is similar to that of the previous effusion. However the most interesting point in this case is that both pleural fluid biochemistries and cellular composition were different (Table 1) causing a diagnostic dilemma. The earlier occurring left effusion was predominantly lymphocytic with high ADA whereas the later occurring right side effusion was polymorph nuclear predominant with low ADA level and that was reconfirmed with repeat analysis and this is why, serum ANA was done to rule out other etiology. ANA was negative, Gram stain and aerobic culture were non-yielding, PCR for MTB was positive in the right side effusion and finally response to ATT lead to conclude that it was none else than due to tuberculosis.
| Pleural fluid | Left pleural effusion | Paradoxical right pleural effusion |
|---|---|---|
| Total cell count | 3250 | 4900 |
| Polymorphs: Lymphocytes | 40:60 | 90:10 |
| Protein | 6.20 | 5.6 |
| Sugar | 45 | 60 |
| ADA | 64 | 21 |
| LDH | Not done | 287 |
| Malignant cytology | Negative | Negative |
| Gene X-pert | Not done | Positive |
Table 1: Pleural fluid characteristics.
The reason for paradoxical response has been attributed to ‘immunological rebound’ by which the improved cell-mediated immunity (CMI) after treatment coincided with excessive antigen load (bacterial cell-wall residues) resulting from rapid bacterial lysis. This has been proposed for tubercular lymphadenitis and intracranial tuberculomas [5,8]. Rapid bactericidal drugs like Isoniazid (INH) and Rifampicin could be worse offenders than bacteriostatic drugs. The same mechanisms could be operational in the case of pleural effusion. INH is well known to induce lupus though the reported cases are rare. An elevated level of ANA and a decreased level of CH50 are found in the effusion fluids which are characteristic of lupus pleuritis [5].
Corticosteroids are known to modify the severity of the clinical manifestations of tuberculosis [11]. However, there is no data that corticosteroids could prevent the paradoxical worsening seen in various organs. In the present case, pleural effusion on either side resolved with continuation of ATT and steroid was not used.
Currently, it can be safely concluded that the development of contralateral pleural effusion during the treatment for tuberculous effusion in immmunocompetent patients is rare, and it resolves with continuation of therapy in the absence of an alternate etiology.
Conclusion
Development of pleural effusion on the opposite side during treatment of tuberculous pleural effusion is a very rare phenomenon and often prompts the clinician to consider and rule out other possible causes. However it warrants no change in treatment and responds to same chemotherapy regimen.
References
- Tsuyuguchi I (1996) Regulation of human immune response in tuberculosis. Infect Agent Dis 5: 82-97.
- Smith H (1987) Pradoxical responses during the chemotherapy of tuberculosis. J Inf 15: 1–3.
- Vilaseca J, Lopez VJ, Arnau J, Guardia J (1984) Contralateral pleural effusion during chemotherapy for tuberculous pleurisy. Tubercle 65: 209-210.
- Majed S (1996) Study of paradoxical responses to chemotherapy in tuberculous pleural effusion. Respir Med 90: 211–214.
- Campbell IA, Dyson AJ (1977) Lymph node tuberculosis: A comparison of various methods of treatment. Tubercle 58: 171–179.
- Ish P, Chakrabarti S, Bhattacharya D (2006) Flummoxing paradox of contralateral pleural effusion developing during successful drug treatment of a tubercular pleural effusion. Case In Point - Clinics In PulmonoloGY 3: 104-106.
- Chopra V, Singh U, Chopra D (2008) Contra-lateral paradoxical pleural effusion during anti-tuberculous chemotherapy. Lung India 25: 124-125.
- Smith Hillas (1983) Immunology of cerebral tuberculosis. Prog Clin Neurosci 1: 99-103.
- Hiraoka K, Ngata N, Kawajiri T, Suzuki K, Kurokawa S, et al. (1998) Paradoxical response to anti-tuberculous chemotherapy and Isoniazid induced lupus. Respiration 65: 152–155.
- Onwubalili JK, Scott GM, Smith H (1986) Acute respiratory distress related to chemotherapy of advanced pulmonary tuberculosis: A study of two cases and review of the literature. Q J Med 59: 599-610.
- Senderovitz T, Viskum K (1994) Corticosteroids and tuberculosis. Respir Med 88: 561-565.
Citation: Upadhyay S (2017) Flummoxing Paradox of Pleural Effusion: Contralateral Effusion with Different Cytobiochemical Features Evolving on Anti-tubercular Chemotherapy. J Respir Med 1: 103.
Copyright: © 2017 Upadhyay S. This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 4659
- [From(publication date): 0-2017 - Dec 01, 2025]
- Breakdown by view type
- HTML page views: 3669
- PDF downloads: 990