Case Report Open Access
Hazards of Using Guiding Elastics for Maxillo Mandibular Fixation (MMF) after Open Reduction and Internal Fixation (ORIF) of Upper Mid Face Fracture: A Case Report
Nidarsh B Hegde1*, Mithra N Hegde2, Freddy Kersi Mistry3 and Saurabh M Gohil3
1Department of Oral and Maxillofacial, Mangalore, India
2Department of Conservative Dentistry and Endodontics A.B. Shetty Memorial Institute of Dental Sciences, Mangalore, India
3Department of Oral and Maxillofacial Surgery, Mangalore, India
- *Corresponding Author:
- Freddy Kersi Mistry
Post Graduate Department of Oral and Maxillofacial Surgery
Mangalore, India
E-mail: drfreddymistry@gmail.com
Received date: April 19, 2015; Accepted date: August 02, 2016; Published date: August 06, 2016
Citation: Hegde NB, Hegde MN, Mistry FK, Gohil SM (2016) Hazards of Using Guiding Elastics for Maxillo Mandibular Fixation (MMF) after Open Reduction and Internal Fixation (ORIF) of Upper Mid Face Fracture: A Case Report. Cosmetol & Oro Facial Surg 2:108. doi: 10.4172/jcofs.1000108
Copyright: © 2016 Hegde NB, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Cosmetology & Oro Facial Surgery
Abstract
In the view of current literature there is no need for Maxillo Mandibular Fixation (MMF) after Open Reduction and Internal Fixation (ORIF) of midfacial fracture. But in order to achieve primary bone healing across fractured segments many surgeons still put the patients on MMF postoperatively for a period of time depending on the extent of fracture in order to achieve primary bone healing. There are various methods in the literature for MMF. We present a case report of a patient undergoing MMF with arch bar and guiding elastics after ORIF of midfacial fracture in order to achieve primary bone healing and the disadvantages we faced post operatively in relation to the occlusion along with its management.
Keywords
Maxillo mandibular fixation (MMF); Open reduction and internal fixation (ORIF); Lefort I fracture; Zygomatic complex fracture; Guiding elastics; Stainless steel wire
Introduction
The management of fractures of the maxillofacial complex remains a challenge for the oral maxillofacial surgeon, demanding both skill and expertise [1]. The anatomy of the head is complex; skin, bone and brain have very different physical properties, in view of the fact that the facial skeleton components articulate and interdigitate in a complex fashion, it is difficult to fracture one bone without disrupting its neighbor. The incidences, demographic distribution, of the fractures vary depending on the geographical area, socioeconomic trends, road traffic accidents, alcohol and drug abuse and seasons [2]. Fractures of the facial skeleton vary in the pattern of presentation, depending on the etiology of injury. Common causes of facial bone fractures are traffic accidents (include motorcycle, automobile, bicycle, pedestrian hit), assault, fall from a height, stumbling, sports, industrial/work related accidents and others/miscellaneous (gunshot injuries, train accidents, pathological fractures) [3]. According to WHO Global Status Report on Road Safety, 2015 Road Traffic Accidents (RTA) is the leading cause of deaths in the world for persons aged 15-29 years. According to this report 1.25 million deaths occurred in the world due to RTA in 2013 [4]. According to a multi-center study in Karnataka, India the common cause for the facial fractures was found to be traffic accidents (72.7%) with a male preponderance and peak incidence during 20-30 years of age. Isolated mandibular fractures were most frequent (41.7%) followed by isolated mid face fractures (21.2%). Among mid face fractures, zygomatic bone and arch were most frequently involved [3].
Case Report
A 50 years old male came with alleged history of RTA. He was admitted in local hospital where primary management was done and was referred to our hospital for further management.
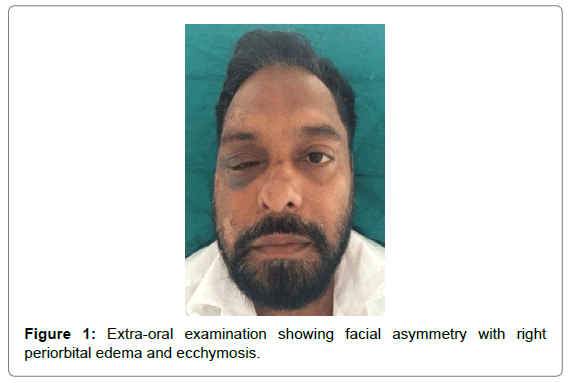
On extra-oral inspection, there was gross facial asymmetry, right periorbital edema and ecchymosis, right sub-conjunctival hemorrhage, multiple abrasions noted over right zygomatic region, supraorbital, temporal region reduced mouth opening and inability to open the right eye completely although eye movements were normal in all gazes. On palpation step deformity was elicited bilaterally over zygomatic region, right zygomatic arch region and right infraorbital rim. Tenderness was present in right zygomatic arch and malar region (Figure 1).
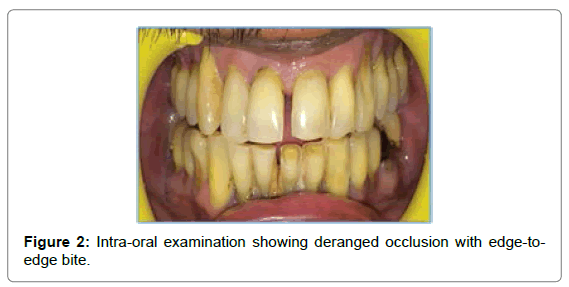
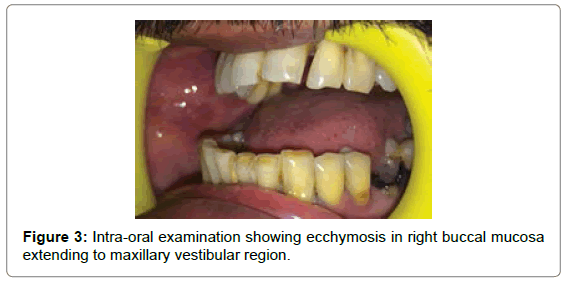
On intra-oral inspection, occlusion was deranged with edge-to-edge bite and ecchymosis was present in the right buccal mucosa. On palpation, mobility of maxilla was noted in the region of premolars and molars. Tenderness was present in the buccal vestibule in the premolar region (Figures 2 and 3).
Investigations
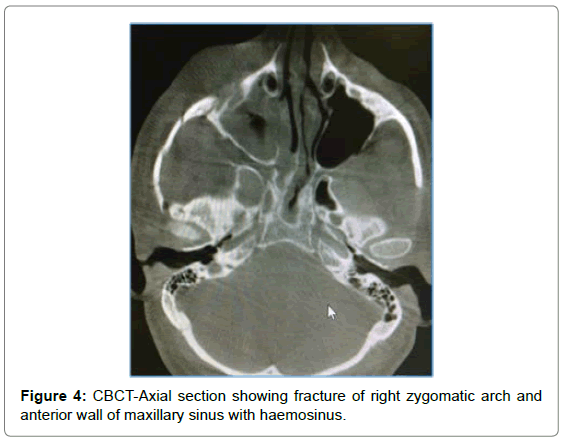
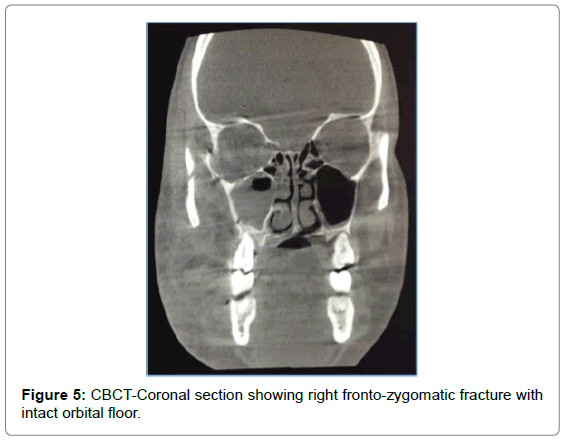
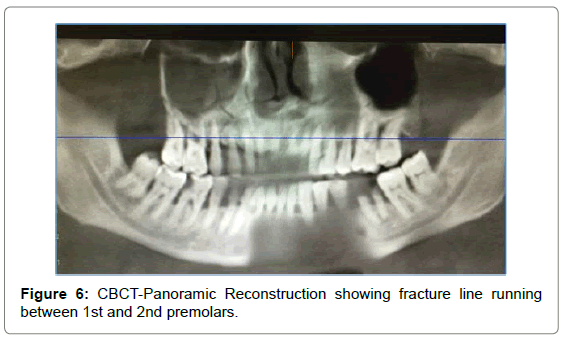
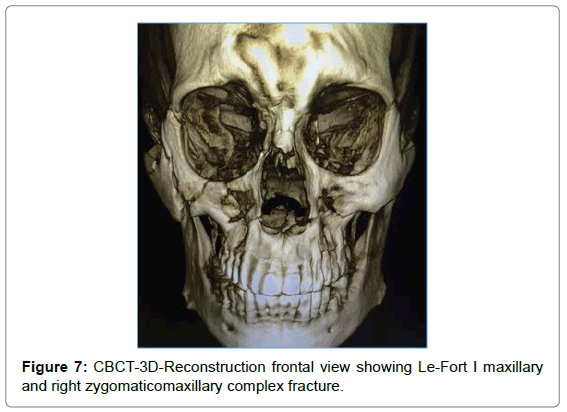
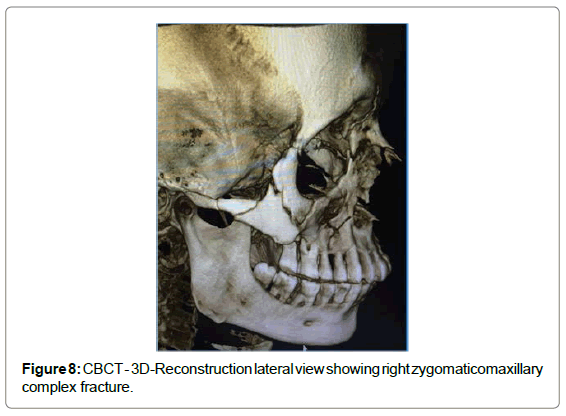
CBCT showed fracture of lateral orbital wall, infraorbital rim, lateral wall of maxillary sinus, opacification of maxillary sinus on right side. Panoramic reconstruction showed fracture of floor of sinus extending interdentally till the alveolar crest between 14 and 15 (Figures 4-8).
Diagnosis
After thorough clinical and radiological examination we arrived at a diagnosis of Lefort I Fracture with Right Zygomatic Complex Fracture, Dentoalveolar Fracture w.r.t. 15-16 region.
Treatment
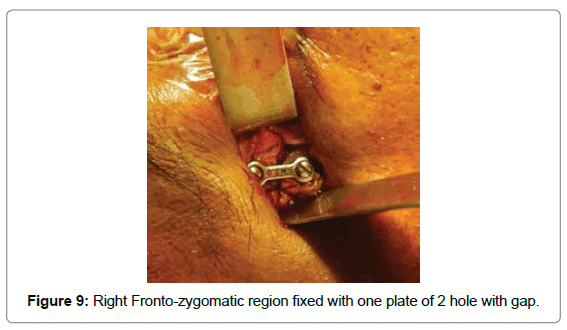
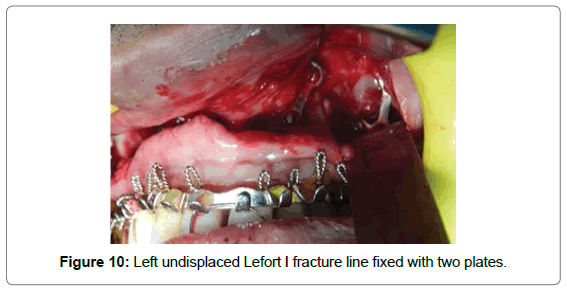
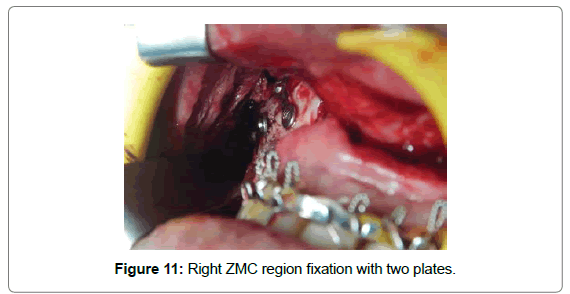
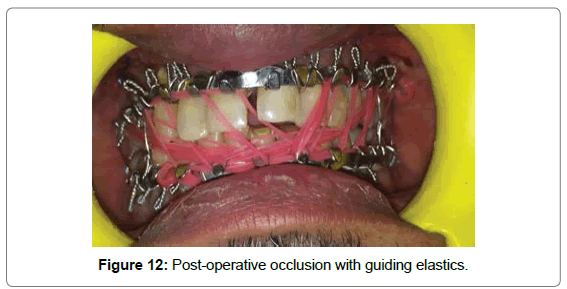
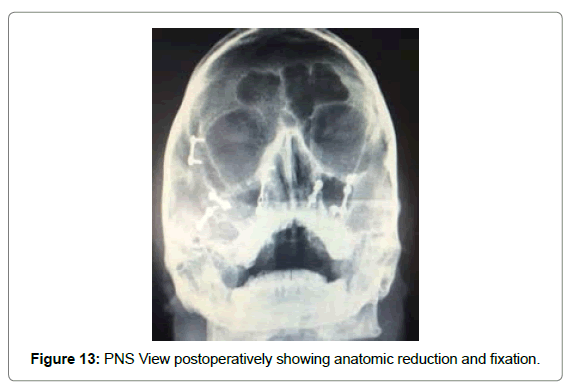
Patient underwent open reduction and internal fixation under general anesthesia. After nasotracheal intubation preparatory surgical protocol was followed by painting the patient with Betadine (10% Povidone Iodine solution) and draping with sterile drapes, arch bars were placed in both the upper and lower arches. Via lateral eye brow approach the fronto zygomatic suture was exposed to identify the fracture line. The fracture segments were reduced and stabilized with 2 hole with gap miniplate (S. K. Surgicals, Pune, India) (Figure 9). The next step was maxillary vestibular approach for reduction and fixation of Lefort I fracture. On exposure the fracture segments were undisplaced on left side. One L-shaped plate (S. K. Surgicals, Pune, India) was placed near the left maxillary buttress region while one 2-hole plate with gap (S. K. Surgicals, Pune, India) was placed near the left piriform region (Figure 10). For right ZMC fracture, reduction was difficult to achieve due to comminution of fractured segments, after reducing with bone holding forceps, one 4-hole plate with gap (S. K. Surgicals, Pune, India) was used near piriform region and two 2-hole plate with gap (S. K. Surgicals, Pune, India) was used each for buttress region and for body of zygoma for fixation (Figure 11). Intermaxillary fixation was done and patient was placed on guiding elastics postoperatively (Figure 12). Post-operative Paranasal Sinus View was taken to evaluate the anatomical reduction and fixation (Figure 13).
Follow-up
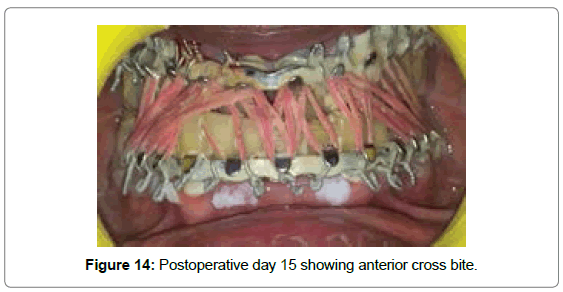
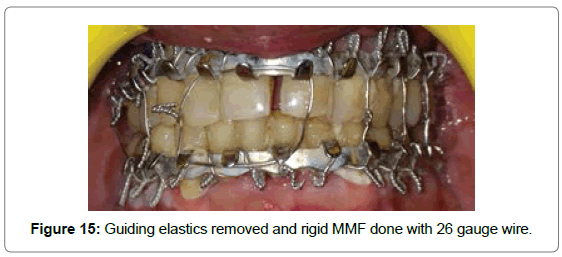
After 15 days: On first follow-up after 15 days it was observed that the patient had anterior cross bite (Figure 14). Guiding elastics were removed and patient was guided into proper occlusion and rigid MMF was done with 26 Gauge Stainless Steel Wire (Figure 15).
After 1 month: There was no mobility of the maxillary segment and proper occlusion was maintained.
Discussion
As a rule, early reduction of a Lefort I fractures presents minimal difficulty. Beyond 7-10 days, increasing force has to be applied to complete reduction. A minimally displaced fracture is reduced and immobilized ideally by open reduction and immobilization carried out by appropriate plating devices. Alternatively and less ideally, 4 weeks of intermaxillary fixation is usually sufficient for healing to occur. In case of sever comminution, it may be necessary to extend the period to 6 weeks. An impacted fracture or one not easily reduced because of early fibrous union should be reduced by the use of either Rowe or Hayton-Williams disimpaction forceps. Two point fixation is minimal requirement for stability in case of unilateral Lefort I fracture [5].
The fact that so many techniques are available for reduction and fixation of zygomaticomaxillary complex (ZMC) fractures indicates that no one technique is always superior to others. It is not so much the actual technique, but the proper application of principles produces satisfactory results. Each ZMC fractures should be treated aggressively with open reduction and internal fixation of at least two of its four major processes [6].
In our case, since the Lefort 1 fracture line was undisplaced there was no need for reduction and only fixation was done with plates to improve the stability, as the zygomaticomaxillary complex was comminuted conventional reduction was not possible and anatomical reduction of the fragments was achieved by instrumental manipulation with fixation at 3 points (frontozygomatic, infraorbital and zygomaticomaxillary buttress region).
Immobilization and maintenance of the occlusion in order to facilitate primary healing are the main goals of using MMF for patients treated with ORIF. There are various studies in the literature for MMF using various techniques [7]. On doing through literature search there aren’t any studies comparing the efficiency of the guiding elastics over the stainless steel wire for immobilization after arch bar fixation. Surgeons prefer elastics over wire because of the ease of cutting elastics by the patient or the bystander in case of emesis or airway problems. Thus we would suggest that a through longitudinal trial should be carried out comparing the efficacy of the guiding elastics over stainless steel wire for immobilization after arch bar fixation.
Conclusion
From our experience with the case we would suggest not to use Guiding Elastics as the method of MMF after ORIF of mid facial fracture. If in case MMF is required it is always advantageous to use 26 gauge stainless steel wires for MMF as a method of rigid fixation.
References
- Thomas DW, Hill CM (2000) Etiology and changing patterns of maxillofacial trauma. In:Booth PW, Schendel SA, Hausamen JE (eds) Maxillofacial surgery, vol. 1.Churchill Livingstone.
- Banks P, Brown A (2001) Etiology, surgical anatomy and classification. In: Banks P, Etiology, surgical anatomy and classification. In: Banks P,Brown A (eds), Fractures of the facial skeleton. Philadelphia, USA, pp: 1-4.
- Shankar AN, Shankar VN, Hegde N, Sharma, Prasad R (2012) The pattern of the maxillofacial fractures e A multicentre retrospective study. Journal of Cranio-Maxillo-Facial Surgery 40: 675-679.
- World HealthOrgansisation (2014) Global Health Estimates.
- Fonseca RJ, Walker RV, Betts NJ, BarberHD, Powers MP (2005) Oral and maxillofacial Trauma. (3rdedn.), Volume 2,Elseiver.
- Fonseca RJ, Walker RV, Betts NJ, BarberHD, Powers MP (2005) Oral and maxillofacial Trauma. (3rdedn.), Volume 1, Elseiver.
- Mcginn JD, Fedok FG (2008) Techniques of maxillary-mandibular fixation. Operative Techniques in Otolaryngology-Head and Neck Surgey 19: 117-112.
Relevant Topics
- Blepharoplasty
- Bone Anchored Hearing Aids
- Chemical peel
- Cleft Surgery
- Congenital Craniofacial Malformations
- Cosmetic Facial Surgery
- Craniofacial Surgery
- Dental Orofacial Surgery
- Dentoalveolar Surgery
- Head and Neck Reconstruction
- Injectable Cosmetic Treatments
- Lip Reconstruction
- Mandibular Nerve Surgery
- Maxfax Surgery
- Maxillofacial Surgery
- Neck Liposuction
- Oral and Maxillofacial Surgery
- Oral Surgery Surgeon
- Orofacial Surgery Braces
- Pediatric Maxillofacial Surgery
- Rhytidectomy
- Sleep Apnea Orofacial Surgery
- Temporomandibular Joint Disorders
- Upper Jaw Surgery
Recommended Journals
Article Tools
Article Usage
- Total views: 20312
- [From(publication date):
December-2016 - Aug 03, 2025] - Breakdown by view type
- HTML page views : 19310
- PDF downloads : 1002