Case Report Open Access
Incidental Finding of Cervical Vertebrae Anomaly Yields to an Undiagnosed Case of Crouzon Syndrome
Karan Nehra1*, B Jayan1, Shiv Shankar Agarwal2 and Mukul Bhatia3
1Department of Orthodontics & Dentofacial Orthopedics Army Dental Centre (Research & Referral) Subroto Park, Delhi Cantt, New Delhi, 110010, India
2Department of Orthodontics and Dentofacial Orthopaedics) Indian Army Dental Corps, India
3Department of Radiodiagnosis & Imaging Armed Forces Medical College, Pune, Maharashtra, India
- *Corresponding Author:
- Nehra K
Department of Orthodontics & Dentofacial Orthopedics Army Dental Centre (Research & Referral) Subroto Park
Delhi Cantt, New Delhi, 110010, India
Tel: +91 9560159623
E-mail: krnnehra@yahoo.co.in
Received date: August 31, 2016; Accepted date: September 24, 2016; Published date: September 29, 2016
Citation: Nehra K, Jayan B, Agarwal SS, Bhatia M (2016) Incidental Finding of Cervical Vertebrae Anomaly Yields to an Undiagnosed Case of Crouzon Syndrome. Cosmetol & Oro Facial Surg 2:109.
Copyright: © 2016 Nehra K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Cosmetology & Oro Facial Surgery
Abstract
Crouzon syndrome is an autosomal dominant, rare genetic disorder often demonstrating complete penetrance and variable expressivity. It is frequently associated with cervical vertebrae abnormalities which often remain undetected. This article reports the case of an incidental finding of cervical vertebral anomaly of atlanto-occipital assimilation in an 8.5 year old boy who reported with chief complaint of inability to eat food properly, midfacial hypoplasia and class III malocclusion. When investigated thoroughly the case was identified as an undiagnosed case of Crouzon syndrome with Arnold Chiari Type I malformation with syringomyelia and asymmetry of atlantooccipital joint. The patient’s neurological examination revealed early signs of quadriparesis and was immediately taken up for posterior cranial fossa decompression surgery. It becomes extremely imperative for an orthodontist to know the cervical vertebral anatomy and associated anomalies and to seek an appropriate referral, as he may be the first to intercept them. Further investigation are mandatory for any underlying associated disorder, as these findings can be of great importance for patients in whom these anomalies assume clinical significance necessitating early/immediate management or lifestyle changes to prevent or delay aggravation of the pathology.
Keywords
Crouzon syndrome; Cervical anomalies; Arnold chiari malformation; Syringomyelia; Craniosynostosis
Introduction
The lateral cephalogram is an important diagnostic radiograph used in clinical orthodontics and an orthodontist is often the first physician to study the skeletal craniofacial morphology of the patient when they seek orthodontic treatment. However, it is seen that cervical spine anatomy is often overlooked and omitted in the routine lateral cephalometric assessment. It is vital to study the cervical vertebrae anatomy as many cervical abnormalities do not manifest themselves symptomatically until adolescence or young adulthood and an orthodontist may be the first to detect some of these [1].
Assimilation of the atlas to occiput, basilar invagination, osodontoideum, congenital synostosis, congenital vertebral fusion, increased atlanto-dental interval are few cervical vertebrae anomalies which an orthodontist can diagnose from the lateral cephalogram [2]. These aberrations should be detected at the earliest, corroborated with clinical findings if present, referred to the appropriate specialist for detailed investigation of any underlying pathological condition, which may require immediate/early intervention.
In 1912 French Neurosurgeon Octave Crouzon first described the hereditary syndrome of craniofacial dyostosis in a mother and son [3] characterized by triad of premature craniosynostosis, midface hypoplasia and exophthalmos. Crouzon syndrome (OMIM NO 123500) is the most frequent form of syndromic craniosynostosis with anapproximate birth prevalence of 1/25,000 - 1/50,000 [4]. This condition is often associated with cervical abnormalities such as butterfly vertebrae and fusion of the bodies and the posterior elements. 18% of the cases have cervical fusion of C2-C3/ C5-C6 vertebrae [5,6] and 70% of patients with Crouzon syndrome present with Chiari malformation Type I [7,8].
Arnold Chiari malformation (CM) Type I is a congenital anomaly defined as the descent of the cerebellar tonsil through the foramen magnum into the upper cervical region. Normally the cerebellar tonsils are confined within skull; however, in subjects with CM, the tonsils descend downwards to the level of the first and sometimes the second cervical vertebra. Patients with CM Type I may present with a variety of symptoms and signs such as headaches to severe myelopathy and compromised brain stem [9-11]. In 50-70% of the patients with CM, blockage of cerebrospinal fluid (CSF) leads to the formation of Syringomyelia (Syrinx=a tube; myelia from the Greek=spinal cord) which is a cyst containing fluid (normally CSF) within the substance of the spinal cord. Syringomyelia is characterized with symptoms which include muscle weakness of arms and legs, scoliosis, dissociated sensory loss, urinary incontinence, dysreflexia, male impotence etc [9,10]. It becomes extremely crucial to recognize such clinical signs and symptoms if cervical anomaly is suspected/diagnosed in the lateral cephalogram.
Herein we present an 8 year old boy who reported to our hospital for orthodontic treatment. Incidental finding of cervical vertebrae anomaly when further investigated led to an undiagnosed case of Crouzon syndrome with Arnold Chiari I malformation and syringomyelia. The patient was immediately taken up for posterior fossa decompression surgery. The purpose of this case report is firstly, to highlight importance of cervical anatomy evaluation on a lateral cephalogram. Secondly to increase the awareness of identification of cervical vertebral abnormalities and associated clinical signs and symptoms of underlying pathology if present by an orthodontist, which may well be life threatening and requires immediate appropriate referral for further evaluation and medical intervention. Thirdly to highlight the clinical signs and symptoms, morphological and radiological features associated with Crouzon syndrome.
Case Study
An 8 year old boy reported to our dental centre with the chief complaint of difficulty in eating, inability to close his mouth properly and a forwardly placed mandible. The medical history revealed no history of any congenital disorder or any long term hospitalization. There was no relevant family history; the patient’s mother had experienced anormal pregnancy and delivery. The patient complained of stiffness in the neck since last 6 months for which no medical treatment was sought. Patient presented with the history of frequent visit to ophthalmologist for recurrent infections in the eyes since last 2 years. Dental history revealed no previous visit to any dental practitioner and early eruption of both maxillary and mandibular permanent teeth at the age of 8.5 years.
Assessment
Extra-oral Assessment
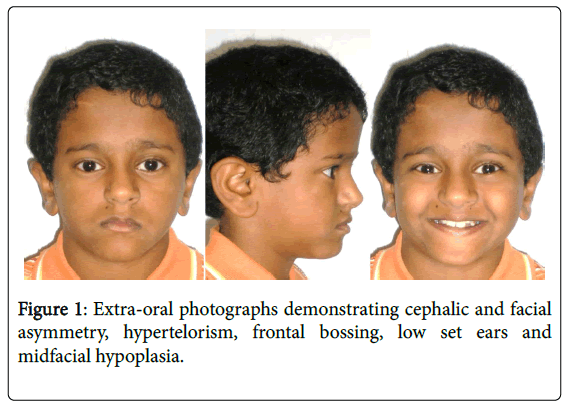
On general examination the patient had short stature and stiff upper body. Extraoral examination (Figure 1) showed frontal bossing, marked facial asymmetry with chin deviated towards the right, hypertelorism, midface hypoplasia and low set ears. Patient had short neck and difficulty in turning his neck on both right and left sides. The patient also had abnormal quality of speech and when questioned, parents noticed the change in the voice since last six months; however, no medical consultation was sought for the same.
Intra-oral Assessment
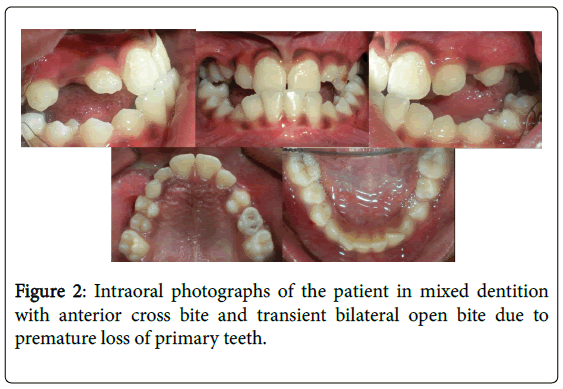
Intraoral examination (Figure 2) revealed early eruption of complete permanent dentition in the mandibular arch. Maxillary arch exhibited early eruption of premolars, decreased maxillary transverse dimension with bilateral posterior cross bite and retained upper right primary second molar and upper left primary canine. There was transient bilateral lateral open bite due to early loss of primary dentition.
Patient had negative overjet with class III incisor relationship and non-specific molar and canine relationship bilaterally. Patient also exhibited moderate crowding in the maxillary arch and mild crowding in the mandibular arch. Dental caries was seen in relation to upper right primary second molar and upper left primary canine. Upper right primary second molar also exhibited grade III mobility indicating an early eruption of the succedaneous tooth.
Radiographic Assessment
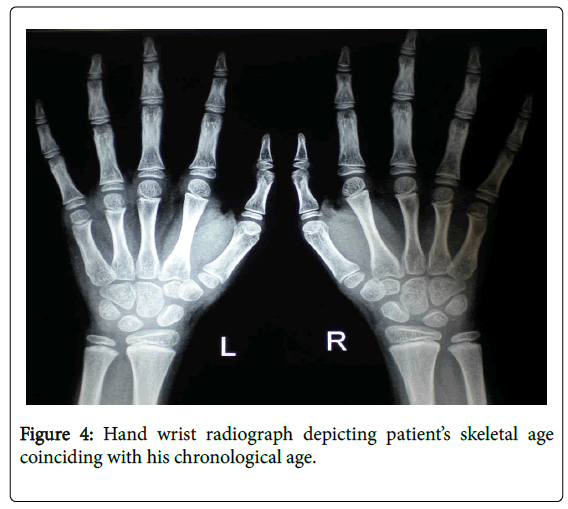
Orthopantomogram (Figure 3) revealed early eruption of permanent dentition at the age of 8.5 yrs. In order to determine the cause for premature eruption of permanent dentition patient was referred for hand wrist radiography to ascertain his skeletal age and associated blood investigations. Hand wrist radiography revealed that his bone age coincided with his chronological age (Figure 4).
Blood investigations revealed growth hormone, alkaline phosphatase, IGF1, TSH, Total T3, Total T4 levels within normal limits. Patient’s growth velocity chart showed normal growth with his stature and weight between 25th-50th percentiles for his age. The patient was diagnosed with an unexplained rare idiopathic early eruption of permanent dentition at the age of 8.5 yrs.
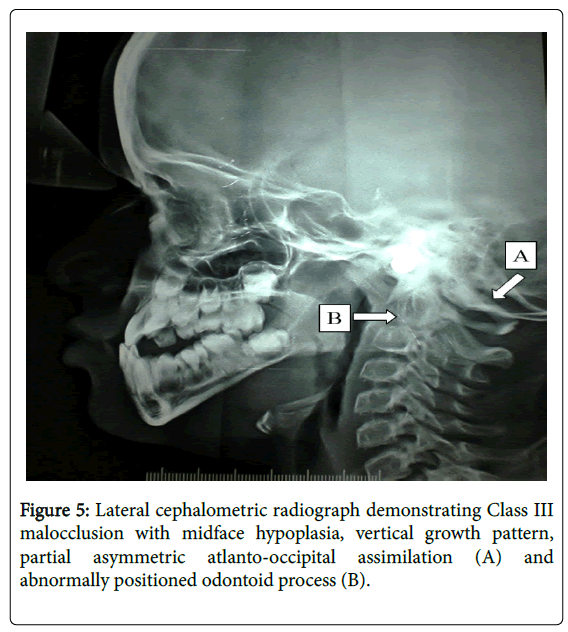
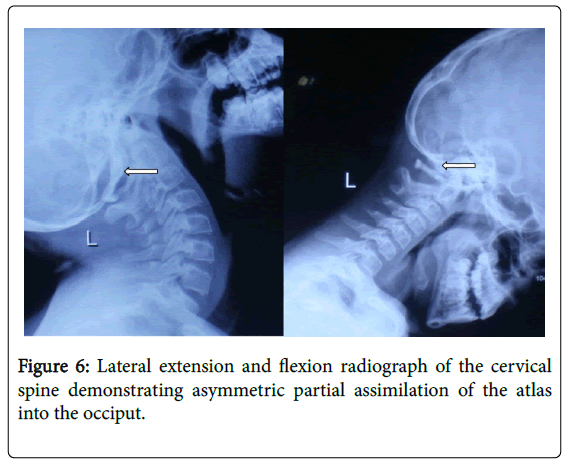
Lateral cephalogram (Figure 5) revealed midface hypoplasia, class III skeletal malocclusion with ANB=-4°C. Patient also exhibited vertical growth pattern with GoGn-SN =35°C. On careful examination cervical vertebral column showed partial atlanto-occipital assimilation and abnormally positioned odontoid process. Collaborating with clinical signs and symptoms of stiffness in the neck since last 6 months the patient was referred to the radiologist for further evaluation and opinion. Cervical extension and flexion radiographs (Figure 6) confirmed asymmetric atlanto-occipital assimilation with the lateral mass on the left partly fused with the occiput. No scoliosis of the cervical spine was seen.
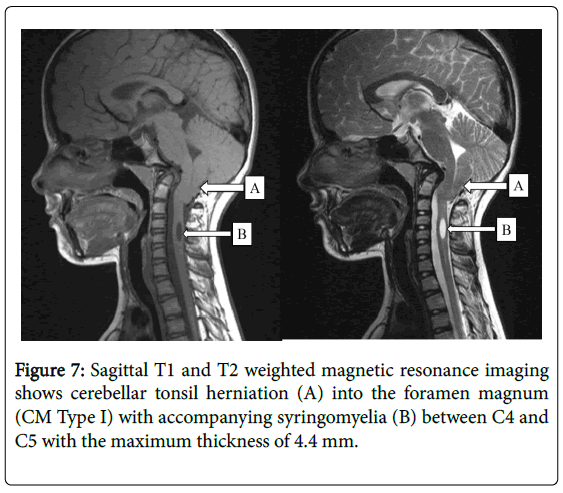
The radiologist recommended a magnetic resonance image (MRI) of the cervical spine. MRI (Figure 7) obtained showed odontoid peg projected posteriorly and superiorly into the posterior cranial fossa leading to severe compression of the medulla which was deformed and compressed against the cerebellar hemispheres. The tonsils were peg like and project 9 mm below the foramen magnum. A short segment syrinx was seen at the level of C4 and C5. The maximal width of the syrinx was 4.4 mm, the cord was expanded and the peripherally placed cord parenchyma thinned. The case was diagnosed as Arnold Chiari Malformation Type I with syringomyelia and asymmetric atlantooccipital assimilation.
Discussion
Lateral cephalometric roentgenographic examination of the cervical spine may reveal a pathologic disorder in asymptomatic as well as in symptomatic subjects. During the lateral cephalometric radiographic assessment of the patient; cervical anomaly of atlanto-occipital assimilation was incidentally diagnosed. Preliminary investigations of this incidental finding steered us to an undiagnosed case of Arnold Chiari malformation Type I with syringomyelia.
Arnold Chiari malformation Type I is generally asymptomatic during childhood and often manifests itself with headaches which are often aggravated by valsalva maneuvers such as yawning, laying, crying, coughing or sneezing. Other symptoms include dizziness, vertigo, nausea, nystagmus, tinnitus, sleep disturbances, dysphagia, impaired coordination, facial pain, dystonia and chronic fatigue, change in voice etc [9-11]. Diagnosis of CM is made through a combination of patient history, neurological examination and an MRI of cervical spine which shows a downward herniation of the cerebellar tonsils greater than 5 mm below the foramen magnum. Patient presented with a history of abnormal change in speech since last 1.5 years however, no medical attention was sought for the same. In the CM patients blockage of cerebrospinal fluid (CSF) generally causes a syrinx to be formed which eventually leads to syringomyelia. Syringomyelia present with a variety of symptoms ranging from neck and arm pain through to fairly severe disability, with muscle weakness and paralysis [9,10]. Syringomyelia was diagnosed in our patient with a syrinx segment at the level of C4 and C5 (Figure 7).
On further physical examination of our patient, attention was drawn towards the patient’s facial and cephalic asymmetry, class III skeletal profile, midface deficiency, frontal bossing, shallow orbits, hypertelorism, low set ears, recurrent conjunctivitis and other features resembling craniosynostosis. Further genetic investigations confirmed the diagnosis of Crouzon syndrome. Craniosynostosis involves premature fusion of cranial sutures as early as in utero thereby causing abnormal bone growth and facial deformities. The order and rate of suture fusion determine the degree of deformity and disability. CM TypeI has a tendency to accompany syndromic craniosynostosis more commonly than sporadic synostosis [12] and is seen in 70% of patients with Crouzon syndrome [7,8]. The premature fusion of these cerebral sutures especially the lambdoid suture which results in a relatively small posterior fossa has been accepted as the probable etiological cause for the development of CM Type I in patients with syndromic craniosynostosis.
Crouzon syndrome is an autosomal dominant, rare genetic disorder which may demonstrate complete/incomplete penetrance and variable expressivity [13]. It may be transmitted as an autosomal dominant genetic condition or can express as a mutation with complete/ incomplete penetrance and variable expressivity. It makes up approx. 4.8% of all the cases of craniosynostosis making it the most common syndrome associated with craniosynostosis [14,15]. The disease is characterized by premature synostosis of cranial sutures which begins in the first year of life. Once the sutures become closed, growth potential to those sutures is restricted. The clinical picture may vary greatly from mild to severe midfacial and orbital anomalies; which include abnormal head shape, mandibular prognathism, midfacial hypoplasia, shallow orbits, bilateral ocular proptosis, divergent strabismus, hypertelorism, conjunctivitis or exposure keratoconjunctivitis, optical atrophy and a non-explained loss of visual accuracy [5,6]. Upper airway obstruction can lead to acute respiratory distress and increased intracranial pressure can lead to optic atrophy which may produce blindness if the condition is left unmanaged. Intraoral manifestations include V shaped maxillary arch with dentoalvoelar crowding. Occasional cleft palate, bifid uvula, oligodontia, macrodontia, and pegshaped teeth have also been reported [16]. Class III malocclusion due to maxillary hypolplasia is seen in 75% of patients with Crouzon syndrome [17]. Hydrocephaly and mental retardation may also develop due to premature closure of cranial sutures.
Crouzon syndrome is caused by mutation in the fibroblast growth factor receptor 2 (FGFR2 ) gene at the chromosomal locus 10q 25.3q 26 and more than 30 different mutations within the gene have been documented in separate families [18]. Five autosomal dominant craniosynostosis syndromes (Apert, Crouzon, Pfeiffer, Jackso-Weiss and Crouzon syndrome with acanthosis nigricans) result from mutations in FGFR genes [19]. Cervical vertebrae abnormalities associated with Crouzon include butterfly vertebrae and fusion of the bodies and the posterior elements. Cervical fusion are present in 18% of the cases with C2-C3 and C5-C6 being equally affected [5,6].
The current case is a unique example of Crouzon syndrome with rare idiopathic early eruption of permanent dentition. Despite presence of clinical features of cranial and facial asymmetry, frontal bossing, hypertelorism, recurrent eye infections, restricted neck movements and abnormal changes in speech, the patient and his family never attempted to seek professional medical help. It was only when the patient reported to seek orthodontic treatment for midface deficiency and the incidental finding of cervical vertebrae anomaly was diagnosed and investigated that a diagnosis of Crouzon syndrome with Chiari Malformation I and syringomyelia was established. The patient’s neurological examination revealed early signs of quadriparesis and was immediately operated for foramen magnum decompression. It has been shown that both craniosynostosis and CM TypeI with craniosynostosis are diagnosed at an early childhood [20]. However, our patient remained undiagnosed till the age of 8.5 years. It is assumed that the syndrome would have not been diagnosed had the incidental finding of atlanto-occipital assimilation not been identified and investigated or until the onset of severe symptoms with aggravated pathology.
Summary
The cervical spine in the lateral cephalogram is often overlooked and omitted in orthodontic cephalometric tracings. Many cervical abnormalities do not manifest themselves symptomatically until adolescence or young adulthood and the orthodontist may be the first person to detect some of these. It becomes imperative for an orthodontist to have a sound knowledge of cervical anatomy to diagnose some of these defects which not only influences the orthodontic treatment plan but also can have serious implications on the quality of the life of an individual. Progressively degenerative defects, if discerned early, may help in mitigating of the severity of their consequences.
References
- Vastardis H, Evans CA (1996) Evaluation of cervical spine abnormalities on cephalometric radiographs. Am J Orthod Dentofacial Orthop 109: 581-588.
- Soni P, Sharma V, Sengupta J (2008) Cervical Vertebrae Anomalies—Incidental Findings on Lateral Cephalograms. Angle Orthodontist 78: 176-180.
- Crouzon O (1912) Dysostose cranio-faciale hereditaire. Bull Mem Soc Med Hosp 33: 545-555
- Cohen MM Jr (1988) Craniosynostosis update 1987. Am J Med Genet 4: 99-148
- Moyen G, Mbika CA, Makosso E (2006) Formecongénitale de la maladie de Crouzon. Arch Péd 13: 395-398
- Bowling EL, Burstein FD (2006) Crouzon syndrome. Amer Optometric Assoc 77
- Cinalli G, Reiner D, Sebag G, Sainte Rose C, Arnaud E, PierreKahn A (1995) Chronic tonsiller herniation in Crouzon's and Apert's syndromes: The role of premature synostosis of the lambdoid suture. J Neurosurg 83: 575-582.
- Fogh-Andersen P (1943) Craniofacial dysostosis (Crouzon's disease) as a dominant hereditary affection. Nord Med 18: 993-996.
- Iskandar BJ, Oakes WJ (1991) Chiari Malformations. Principles and Practice of Pediatric Neurosurgery. Albright L, Pollack I, Adelson D. (eds). Thieme Medical Publisher, Inc, New York, pp:165-185.
- Levy WJ, Mason L, Hahn JF (1983) Chiari malformation presenting in adults: a surgical experience in 127 cases. Neurosurgery 12: 377-390.
- Menezes AH (1991) Chiari I malformations and hydromyelia complications. PediatrNeurosurg 7: 146-154.
- Leikola J, Koljonen V, Valanne L, Hukki J (2010) The incidence of Chiari malformation in nonsyndromic, single suture craniosynostosis. Childs Nerve Syst 26: 771-774.
- de Ravel TJL, Taylor IB, Van Oostveldt AJT, Fryns JP, Wilkie A.O.M (2005) A further mutation of the FGFR2 tyrosine kinase domain in mild Crouzon syndrome. Eur J Hum Genet 13: 503-505.
- Everett ET, Britto DA, Ward RE, Hartsfield JK Jr (1999) A novel FGFR2 gene mutation in Crouzon syndrome associated with apparent nonpenetrance. Cleft Palate Craniofac J 36: 533-541.
- Hlongwa P (2009) Early orthodontic management of Crouzon Syndrome: A case report. J Maxillofac Oral Surg 8: 74-76.
- Posnick JC (1994) The craniofacial dysostosis syndromes: current reconstructive strategies. Clin Plast Surg 4: 585-598.
- Kreiborg S, Aduss H. (1986) Pre- and postsurgical facial growth in patients with Crouzon’s and Apert’s syndromes. Cleft Palate J 78-90.
- Jabs EW, Li X, Scott AF (1994) Jackson-Weiss and Crouzon syndromes are allelic with mutations in fibroblast growth factor receptor 2. Nat Genet 8: 275-279.
- Preising MN, Schindler S, Friedrich M, Wagener H, Golan I, et al. (2003) On the effect of mutations of the fibroblast growth factor receptors as exemplified by three cases of craniosynostosis. Klin Monatsbl Augenheilkd 220: 669-681.
- Strahle J, Muraszko KM, Buchmann SR, Kapurch J, Garton HJ, et al. (2011) Chiari malformation associated with craniosynostosis. Neurosurg Focus 31.
Relevant Topics
- Blepharoplasty
- Bone Anchored Hearing Aids
- Chemical peel
- Cleft Surgery
- Congenital Craniofacial Malformations
- Cosmetic Facial Surgery
- Craniofacial Surgery
- Dental Orofacial Surgery
- Dentoalveolar Surgery
- Head and Neck Reconstruction
- Injectable Cosmetic Treatments
- Lip Reconstruction
- Mandibular Nerve Surgery
- Maxfax Surgery
- Maxillofacial Surgery
- Neck Liposuction
- Oral and Maxillofacial Surgery
- Oral Surgery Surgeon
- Orofacial Surgery Braces
- Pediatric Maxillofacial Surgery
- Rhytidectomy
- Sleep Apnea Orofacial Surgery
- Temporomandibular Joint Disorders
- Upper Jaw Surgery
Recommended Journals
Article Tools
Article Usage
- Total views: 14647
- [From(publication date):
December-2016 - Sep 02, 2025] - Breakdown by view type
- HTML page views : 13641
- PDF downloads : 1006