Research Article Open Access
Increased Autism Incidence: Is there a Single Cause?
Sarah Crawford*
Department of Biology, Southern Connecticut State University, USA
- *Corresponding Author:
- Sarah Crawford
Department Biology, Southern Connecticut
State University, 501 Crescent Street, Room
311c Academic Science Laboratory
New Haven, Connecticut 06515, USA
Tel: +1-203-392-6215
E-mail: crawfords2@southernct.edu
Received Date: January 06, 2016; Accepted Date: February 09, 2016; Published Date: February 12, 2016
Citation: Crawford S (2016) Increased Autism Incidence: Is there a Single Cause?. J Child Adolesc Behav 4:273. doi:10.4172/2375-4494.1000273
Copyright: © 2016 Crawford S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Child and Adolescent Behavior
Abstract
The Quantitative Threshold Exposure (QTE) hypothesis proposes that Autism Spectrum Disorder (ASD) is triggered by the cumulative effects of high-level exposure to endogenous and environmental factors that act as antigens to impair normal immune system (IS) and associated central nervous system (CNS) functions during critical prenatal and early childhood developmental stages. The hypothesis predicts that the greater the number of risk factors and the quantitative amounts of each to which a child is exposed prenatally and in early postnatal life, the greater the likelihood the child will develop some form of ASD as a result of their effects on critically integrated IS and CNS pathways active during prenatal, neo-natal and early childhood brain maturation. These risk factors have been identified in extensive epidemiological studies to include genetic predisposition, maternal fetal exposure to infectious disease, inflammatory and autoimmune phenomena, as well as exposure to antigenic and proinflammatory environmental factors. The incidence rates of several potential risk factors for ASD correlates with observed increases in ASD incidence over the past several decades, including increased incidence of pediatric infectious disease, increased obesity/ diabetes type-2 in parents of child-bearing age and Increased use of tetrahydrocannabinol (THC) during childbearing years. This model may be useful even when the individual contributions of specific risk factors cannot be quantified, as it proposes that the combined quantitative level of exposure to risk factors for ASD rather than exposure to any one risk factor per se defines threshold occurrence rates. The model has important predictive value, as it suggests that, rather than attempting to identify a specific causative agent linked to ASD, the combined risk factor profile should be evaluated in population studies in order to specify more accurately the limits of pre- threshold exposure.
Keywords
Autism; Diabetes; Obesity; Childhood
Introduction
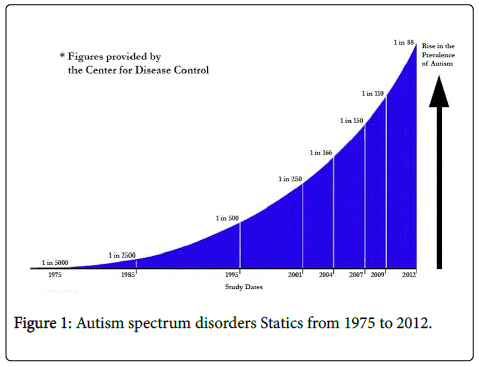
The dramatic increase in the incidence of autism spectrum disorders (ASDs) over the past several decades has provoked widespread attention to potential causes of this disturbing trend. Two decades ago, autism was detected in 1 in 1000 children; as of 2014 an estimated 1 in 88 children has been identified with ASD [1] (Figure 1).
Most importantly, this increase cannot be fully accounted for by the refinement of detection and diagnostic procedures. Recent statistics indicate that only about 50% of the observed increase in autism incidence can be accounted for by changes in diagnostic criteria, public awareness or other non-causal parameters. Given these alarming statistics, it is essential to identify the causes of this trend that is approaching epidemic proportions affecting many countries worldwide. Kanner was the first to identify the neurological disorders associated with language and social impairments defined as “autism” [2].
The term is somewhat ambiguous, since the neurological disorder covers a broad-spectrum group of symptoms that range in severity from mild dysfunction, characterized by Asperger’s Syndrome, to classic autism, that, in its extreme form, causes severe cognitive and developmental deficits. The sheer diversity of symptomtology linked to ASD further complicates issues of cause, effect, diagnosis and prevention.
Any reasonable hypothesis attempting to account for the origins of ASD must take into account the broad-spectrum nature of ASD as well as accounting for its increasing incidence rates. Many epidemiological studies have attempted to define a common profile linked to ASD, with limited success so far. The cited “causes” of ASD appear to be as varied as the manifestations of the disorder; no driver mutation or specific environmental culprit has yet been identified. Nevertheless, a consensus of research has shown that approximately 10% of children with ASD show genetic, neurologic or metabolic differences that may be causally linked to this disorder; the origins of the remaining majority of cases remain etiologically obscure. Neuro-structural differences in the developing brain in children with ASD have been identified. In this context, inflammation has been cited as a contributing factor responsible for these neuro-structural differences. Additional epidemiological research has also identified genetic changes, pre-natal conditions, vaccines and even the environmental milieu as contributory factors in the development of autism [3]. Nevertheless, no specific link has been established between any of these potential risk factors and the development of ASD. Rather, specific genetic profiles and epigenetic factors, such as maternal prenatal immune system dysregulation/activation, have shown a correlated increased risk for the development of autism.
A critical issue confronting parents and clinicians alike is our current inability to define which fetuses/infants and young children may be at enhanced risk for developing ASD. No prevention strategies can be implemented in the absence of a knowledge base that defines cause and effect relationships in ASD. Thus, despite important advances in our understanding of the physiological basis for ASD, it is currently impossible to predict which children will develop this disorder; one can only identify critical biological and environmental risk factors that may increase the likelihood of its occurrence in an individual.
To define a relevant hypothesis on the causation of ASD, one must incorporate the essential well-understood etiological parameters of autism. These are listed below.
Age of incidence
One of the critical epidemiological factors associated with ASD is its restricted timeframe of onset, ranging from new- born to about 3 years. Significantly, this timing of observed onset coincides with the timing of critical stages of postnatal development in both the brain and the immune system. Potential genetic and environmental factors implicated in the development of ASD must be relevant to this restricted developmental timeframe. Risk factors impinging on normal brain development may originate either in pre-natal exposure to agents and/or abnormal gene products that may disrupt the normal process of brain development, or as a consequence of post-natal exposure to exogenous factors and/or endogenous gene products important to these later stages of neurocognitive development. Chief among these is the documented association between aberrations of immune system functions and brain development. The confluence of clinical data suggesting a link between autism and dysregulated immune function and research in developmental biology that shows the integration of central nervous system (CNS) and immune system (IS) formation early in life presents a coherent model for understanding the biological basis for this disorder. Beyond these critical correlations is the necessity of identifying specific roles for genetic and environmental factors that may have etiological significance as risk factors for the development of ASD. Direct evidence of a link between abnormal brain maturation and dysregulated immune system function has been shown by research studies that have identified differences in the immunologic composition of the cerebral spinal fluid, microglia and macrophages in autistic individuals [4].
Identification of risk factors linked to abnormal brain development whose pre-and post-natal exposure levels have increased in conjunction with increased incidence rates for ASD.
This epidemiological criterion explores the notion that it may be possible to use available epidemiological data to identify (a) potential cause(s) of ASD by defining the parameters responsible for the dramatic upswing in ASD incidence in recent years. Thus, the most important clue to the cause of ASD risk may be the statistic itself that may lead to the identification of potential risk factors based on their coincident increase with ASD. The extraordinary recent rate of increase in ASD rules out certain etiological risk factors as the primary cause of ASD. For example, the physiological role of genetic mutations as a cause of ASD, based on known mutational frequency rates, is far too low to account for the observed increase in ASD incidence. This observation essentially rules out genetic mutations as the sole cause of ASD. What we are left with, then, is the probability that a dramatic change and/or increase in exposure to etiological factors that predispose to ASD in prenatal and early postnatal years accounts, at least in part, for the observed increase in ASD incidence. An exploration of environmental changes that have occurred over the past several decades with the potential to impact brain development in utero and early in life may permit the identification of key causal factors of ASD (Table 1). In this regard, risk factors implicated in impaired brain development that have shown increased prevalence in conjunction with ASD include the following:
| Risk Factors: Quantitative Association with ASD | |
|---|---|
| Risk factor * | Calculated ASD risk ** |
| * (15%)Pre-natal obesity BMI>35 | 3 |
| *Maternal obesity and PGDM | 3.91 |
| *Maternal obesity and GDM | 3.04 |
| *Prenatal auto-immune disorders | |
| I family member | 1.9 |
| 3 family members | 5.5 |
| Vaccines (MMR)/thimerosal | 0 |
| Genetic factors | |
| Monozygotic twins | 1.8 |
| Dizygotic twins | 1.1 |
| * (10%) Maternal cannabis use | ND |
| *(13%) Infant daycare (age 1-2) | ND |
| *(15%) Infant daycare (age 0-12mos) | ND |
| * (137%) Daycare reported infectious disease | ND |
| * (239%) Infant hospitalization (bronchiolitis) | ND |
| *(11)%) Parental age | ND |
*%Significantly increased over past 30 years
**Numbers show n–fold increase above rates observed in the absence of stated risk factor ND=no data
Table 1: Risk factors weighted based on documented association with autism.
Increased incidence of pediatric infectious disease
Epidemiological data on pediatric illnesses show not only an elevated incidence of ASD over the past several decades, but also in the incidence of childhood infections, asthma and other autoimmune disorders, whose rate of increase has occurred in parallel to that of ASD [5-7]. The link between infectious disease and brain development can be found in research that has shown that immune system cytokines whose levels may be affected by infectious disease play an important role in normal brain development as well as contributing to pathological injury to the developing brain.
In support of the posited risk factor/ASD incidence rate association, clinical data suggest that the incidence rates of early childhood infections have increased significantly over the past several decades. Clinical research studies on the patterns of childhood infections have shown that rates of infant and early childhood infectious disease have been affected by changes in early childhood care practices over the past half century that have been associated with an increased incidence of pediatric infections despite the widespread availability of antibiotics and vaccines.
The cause may be related to changes in infant care practices that result in increased risk of exposure to infectious disease early in life. According to Monthly Labor Review, one of the most dramatic changes in the US society in the past 75 years has been the increasing percentage of women, including mothers of infants that work outside the home, resulting in a substantial increase in the number of infants in daycare [8]. In 2014 the percentage of US children of working mothers in daycare under a year old was 57.1%. Research has shown that incidence rates for infections in infancy are higher for babies cared for in multiple settings, particularly daycare. A study by Bell et al. in 1989 of 843 children under 36 months of age showed that children cared for at home had 2.03 infections on average during the six month study period [9]. Adjusted rates of excess infection rates were 0.09 in relatives’ homes, 0.1 in daycare homes, 0.79 in day care centers and 0.66 in multiple settings. Interestingly, the strongest predictor of early childhood illness was the number of children in a single room in a caregiving facility: the greater the number of children, the greater the infection rate. Moreover, children in daycare centers were 4.5 times more likely to be hospitalized for infections than children in other care settings.
An additional study by Hurwitz et al. showed a statistically significant increase in respiratory illness rates in infants from 6 weeks to 17 months who attended group daycare [10]. Yet another clinical study by Shay et al. showed that between 1980 and 1996 rates for hospitalization of infants suffering from bronchiolitis increased significantly, particularly among children younger than 6 months, in which the increase was 239% [11]. Moreover, the rate of hospitalization for children with bronchiolitis increased for all age groups during this time period. These infectious disease rate increases correlated with increased rates of early childhood daycare enrollment during this period. Among children of working mothers aged between 1 and 2 years, the enrollment percentage increased from 12% in 1982 to 25% in 1993. For children 0–12 months, this percentage rose from 5% to 20% during this time frame. The authors concluded that the trend of increasing childcare enrollment in group daycare may be associated with increased rates of respiratory syncytial virus (RSV) associated bronchiolitis in very young children. According to a study by Hagerhed-Engman et al., children who attended day care had an increased risk of airways infections, eczema and food allergies [12]. A total of 10,851 children, 1–6 years were assessed in this study. This increased risk was mainly seen in younger children 1–4 years.
To the extent that immune system responses to early childhood infectious disease may, in some (genetically predisposed?) children, affect critical windows of brain development, the incidence and severity of early childhood infectious disease rates from any cause may represent a risk for ASD.
Changes in infant/early childhood feeding practices
Modern caregiving trends increasingly have involved shorter duration of exclusive breastfeeding as the primary source of infant nutrition as well as the introduction of a variety of solid foods early in life. Earlier childrearing practices into the 20th century in the US and most parts of the developed world involved breastfeeding (often exclusively) for most of the 0–3 years critical IS/CNS developmental window associated with ASD risk.
Several important research studies have shown that specific infant feeding patterns such as early introduction of bottle feeding or solid food in place of longer periods of exclusive breastfeeding may lead to reduced lung and airway growth and increased risk of autoimmune disorders [13]. The link between breast- feeding duration and immune system function may involve components of breast milk that affect immune system stability and function. These stabilizing effects of breast milk on the immune system may also have a protective effect against ASD. The correlation between infant feeding pattern and ASD risk is particularly compelling given the documented association between gastrointestinal dysfunction in infancy and ASD [14].
Increased incidence of obesity/diabetes type-2 in parents of child-bearing age
Maternal (and possibly paternal) obesity comprises another important risk factor for altered brain development and ASD. Currently, approximately 34% of women of childbearing age in the US are obese; these numbers have increased appreciably over the past several decades. A US study of 1311 mothers and children between 2005 and 2012 showed that severely obese mothers (BMI>35) were three times more likely to have a child who develops ASD [15]. The increased risk of ASD in children of obese mothers was independent of other risk factors, including pregnancy weight gain, gestational diabetes, duration of breastfeeding, postnatal depression or infant birth weight.
Maternal gestational diabetes (GDM) is often associated with obesity and represents yet another (separate from obesity) risk factor for ASD. A study by Feig et al. conducted in Ontario, Canada showed that the incidence of GDM and pre-GDM in pregnancy doubled between 1996 and 2010 [16].
Increased use of tetrahydrocannabinol (THC) during childbearing years
In utero exposure to drugs that interact with neural pathways has been implicated as an important risk factor for ASD. Cannabis/ tetrahydrocannabinol (THC) is the most widely used psychotropic drug; its use has increased substantially over the past 20 years; moreover, more recent formulations of the drug display enhanced potency due to changes in preparation methods [17]. Currently, cannabis use during pregnancy is estimated at 10%. Recent studies by Passey et al. [18] and Shabani et al. [19] have shown that neural deficits can result from in utero cannabis exposure. Moreover, Siniscalco et al. [20] have suggested that the endocannabinoid (EC) system may play an important role in the integrated IS/CNS developmental pathway that is dysregulated in autism. Their research has shown that the cannabinoid receptor type 2(CBR2) signal pathway is upregulated in peripheral blood mononuclear cells (PBMCs) from children with ASD. This finding raises the possibility that the endocannabinoid (EC) system may be associated with ASD. In addition, the authors found reduced levels of bone marrow differentiated macrophages (BMDCs) in children with ASD that may be linked to altered CBR-2 levels.
Endogenous cannabinoids bind to type-1 cannabinoid receptors in the central nervous system (CNS) to guide neural pattern formation and network connectivity in the developing brain. Research by Cutando et al. provides evidence that THC binding of EC-1 receptors as a consequence of subchronic cannabis exposure may affect these signal pathways, at least in part, by activating microglial cells important to neural function [21]. Similar patterns of cerebellar microglial activation have been documented in the brains of autistic children, suggesting similar pathways may be involved. Tortoriello et al. [22] have recently determined that THC affects EC-1 receptor signaling in the developing fetal brain by altering fetal cortical circuitry, further implicating THC as a potential cause of autism.
Integrating the causal links to ASD: The quantitative threshold exposure (QTE) hypothesis
Author have recently proposed a new model to explain the origins of ASD and to account for its rapid rise over the past several decades, the Quantitative Threshold Exposure (QTE) hypothesis [23]. It is a model drawn from classical multifactorial genetics to explain the biological or phenotypic consequences of combined cumulative exposure levels to diverse risk factors that collectively contribute to the onset of congenital disorders with pleiotropic consequences on development. An individual will not express a multifactorial disease trait unless the quantitative effects of risk factors, of genetic and/or environmental composition, reach a critical threshold. The threshold model of disease is of particular utility in assessing multifactorial disorders involving critical developmental/exposure windows such as cleft palate and spinal bifida.
The Quantitative Threshold Exposure (QTE) hypothesis of ASD is a multifactorial threshold model that proposes that ASD is triggered by the cumulative effects of exposure to endogenous and environmental factors that act as antigens to impair normal immune system (IS) and associated central nervous system (CNS) functions during critical developmental phases. This model accounts for the cumulative effects of risk factor exposure in both the causation of ASD and its dramatic increase over the past 30 years. The model rejects the concept that a single genetic or environmental agent is the cause of most cases of ASD. Rather, the QTE hypothesis proposes that it is the quantitative exposure level to any number or combination of genetic and environmental risk factors at critical developmental stages that determines whether the threshold exposure level is sufficient to cause ASD. This model may be useful even when the individual contributions of specific risk factors cannot be quantified, as it proposes that the combined quantitative level of exposure to risk factors for ASD rather than exposure to any one risk factor per se defines threshold occurrence rates.
The hypothesis predicts that the greater the number of risk factors and the quantitative amounts of each to which a child is exposed prenatally and in early postnatal life, the greater the likelihood the child will develop some form of ASD. Taken together, the cumulative exposure level may cause an individual to cross the threshold boundary to develop ASD. The model further predicts that, once the threshold exposure level sufficient to impair CNS development to cause ASD is attained, additional increases in quantitative risk factor exposure may determine the severity of ASD, thereby accounting for the spectrum or range of neurological impairments identified in children with ASD.
The timing as well as the level of exposure to ASD risk factors may critically impact not only whether the disorder threshold is met, but also the severity of ASD. This combined quantitative/ developmental timing of exposure criteria has previously been applied to risk factors associated with congenital developmental disorders such as spinal bifida, microencephaly and cleft palate/ hare lip syndromes. The severity of each of these disorders is tightly associated with the timing of pre-natal events that interfere with programmed morphogenetic CNS development pathways. In ASD also, the level of exposure necessary to trigger an impairment of CNS development may vary significantly with the timing of exposure to determine threshold impact and the severity of ASD. Earlier prenatal exposure may impact programmed CNS pathways that occur normally during gestational growth, whereas post-natal exposure may affect stages of brain development programmed to occur in the first several years of life.
In contrast to some current hypotheses on the origins of ASD that implicate specific environmental risk factors (such as early childhood vaccines), the QTE hypothesis does not associate a specific individual risk factor with the risk of developing ASD. The QTE hypothesis is consistent with many identified etiological risk factors associated with ASD and provides a substantive explanation for its dramatic increase in incidence over the past several decades.
How does this hypothesis stand up to the epidemiological profile for ASD? First and most important, the hypothesis argues against a single environmental culprit-such as vaccines – in the causation of ASD. Rather, it argues that the sum total of antigenic exposure coupled with an at-risk genetic profile is responsible for generating a threshold boundary for ASD development. This hypothesis accounts for the failure of epidemiologists to identify a single specific risk factor for ASD or a single genetic profile that is associated with enhanced risk. Rather, the sum total of epidemiological data supports the notion of the QTE hypothesis, as it implicates a plethora of infectious disease, autoimmune phenomena linked to ASD, all of which increase the risk of ASD, but none of which has been implicated as a single agent causative factor. Thus, the QTE hypothesis integrates a diverse group of genetic and environmental factors with the timing of exposure, such that this complex and unstable environmental interface with critical periods of IS/CNS development may be responsible for the increased incidence of ASD.
The QTE hypothesis suggests a positive correlation between excessive antigenic exposure and disordered brain development when it occurs during critically sensitive periods of CNS development. The identification of a causal link requires an in-depth assessment of pertinent etiological factors that may affect brain development at these critical stages. A causal link is suggested by clinical data showing that brain development is influenced by antigenic stimuli that elicit immune activation and modulatory mech-anisms that interact physiologically with the developing brain. In this regard, the number and quantity of antigenic stimuli to which the developing brain is exposed may be critical.
The Quantitative Exposure Threshold hypothesis for ASD is consistent with our current understanding of the epidemiological risk factors and etiological mechanisms connecting immune system dysfunction with abnormal brain development seen in ASD. The model has important predictive value, as it suggests that, rather than attempting to identify a specific causative agent linked to ASD, the combined risk factor profile should be evaluated in population studies in order to specify more accurately the limits of pre-threshold exposure.
Relative contributions of risk factors to ASD incidence rates
While the QTE hypothesis proposes that the sum total exposure to ASD risk factors during critical CNS developmental windows determines the overall likelihood of developing this disorder, it cannot predict the significance of individual contributory risk factors to ASD. This assessment requires a substantive etiological assessment of the relationship between individual risk factors and quantitative measures of ASD incidence rates. With increased research, it may be possible in the future to calculate the weighted significance of risk factors with documented causal connections to ASD and generate a combined risk factor assessment profile for predictive and preventive clinical evaluations.
That said, there are certain risk factors with significant causal associations with ASD that current research suggests may have greater prognostic value than others (Figure 2). Specifically, this category includes physiologically relevant risk factors whose incidence rate increases have occurred over the past several decades in conjunction with increases in ASD incidence rates.
Among the highest weighted of these causal parameters include early childhood infections, autoimmune disorders, maternal obesity and gestational diabetes. Each of these risk factors is etiologically representative of a causal association to ASD and may be considered heavily weighted multifactorial contributors to ASD based on increased prevalence over the past thirty years. With respect to early childhood infections, this connection is suggested by epidemiological evidence showing 0.8 fold higher rate of respiratory infections in infants less than 12 months in multi-caregiver settings along with a 4.5-fold increased likelihood of hospitalization for infectious disease in young children in multi-care settings.
Extreme maternal obesity is currently estimated to be linked to a three-fold increase in ASD risk; moreover, gestational diabetes, whose incidence has increased two-fold since the mid-1990s, represents an independent risk factor for ASD. Thus, obesity and GDM are heavily weighted risk factors for ASD whose incidence has increase in parallel to autism.
Important research suggests a causal relationship between immune system and CNS development. The causal link is further substantiated by epidemiological studies showing that the risk for ASD increases substantially for every first degree relative diagnosed with autoimmune dysfunction. That the incidence of autoimmune disorders has increased significantly and in parallel with the increase in ASD incidence over the past several decades only strengthens the weighted value of this risk factor contribution to ASD. Although genetic studies have implicated over one hundred genes in ASD, no specific genetic contribution is invariably associated with this disorder; moreover, the defective genetic developmental pathways linked to ASD are very poorly understood. The absence of a defined genetic culprit makes the critical assessment of the role of genes versus environment in ASD causation uncertain.
That said, twin studies have shown an ASD recurrence rate of up to 90% in monozygotic twins, one that is significantly higher than for dizygotic twins, thereby directly implicating a causal genetic component to ASD. That the recurrence rate is so high suggests that genetic predisposition may be a heavily weighted risk factor for ASD. More research needs to be done to develop a genetic profile that may be more quantitatively predictive of ASD risk. In addition, it is important to assess more carefully the impact of potential environmental mutagens in increasing the incidence of maternal and paternal mutation rates in reproductive cells that may increase the genetic predisposition for ASD.
Lower weight may be assigned to individual factors that either fail to show a demonstrated increased risk for ASD or an undocumented physiological effect that may be linked to abnormal brain development. Additional risk factors with causal links to ASD suggested by physiological parameters, including changes in infant feeding patterns associated with breastfeeding and prenatal cannabis use, are more difficult to weigh with respect to relative risk, due to the absence of sufficient epidemiological data. Research suggests an indirect link between breast feeding and immune system stabilization early in life; moreover, the high incidence of infant gastric symptoms in babies who later develop autism suggests that this may turn out to be an important contributory risk factor for ASD. Once again, more research is needed to define better the relative strength of this potential ASD risk factor.
With respect to prenatal cannabis use, although recent studies suggest an important causal link between endocannabinoid agonist/ receptor activity and early brain development, more research is needed to determine the statistical association with ASD.
The controversial category of infant vaccines such as measles, mumps and rubella (MMR) falls into this category as well. Vaccines by their very nature directly impact immune system function; combined with exposure to additional risk factors linked to ASD, infant and early childhood vaccines may have an additive effect on the threshold for ASD development. However, the absence of significant epidemiological data suggesting that vaccines per se are linked to any increase in ASD incidence rates requires the placement of this potential risk factor in the category of lesser impact multifactorial risk factors.
The potential impact of the QTE hypothesis on understanding and preventing ASD
The potential significance of the QTE hypothesis is that it may redirect the focus from a single genetic or environmental culprit responsible for autism to a broader perspective that attributes this spectrum of abnormalities in brain development to a spectrum of causes that, as a result of their additive or synergistic impact on the interface of IS and CNS development early in life, may be responsible for ASD. In this context, a paradigm shift from an individual to a combined causative model may facilitate the evaluation of multifaceted genetic and environmental connections to ASD both qualitatively and quantitatively to develop an improved risk factor profile for autism.
The model is limited in that it does not directly implicate or rule out specific risk factors for ASD, nor does it provide for a quantitative assessment of the importance of any one risk factor in the causation of ASD. The hypothesis simply serves as a foundation, a quantitative framework in which contributory risk factors can be evaluated with respect to their combined relative impact on ASD. Individual risk factors subject to evaluation by the QTE may be identified on the basis of epidemiological data showing a positive correlation with ASD and clinical research showing a cause and effect relationship between the risk factor and IS/CNS development. The ASD risk factor assessment presented in this paper were selected on this basis. In addition, the hypothesis facilitates the inclusion of risk factors whose prevalence has increased in parallel to ASD incidence rates, based on inclusion criteria that do not require the evaluation of each potential risk factor as a single causal agent but rather within the broader scope of additive and/or synergistic causal mechanisms. The assessment of the impact of social changes in childrearing practices was based on these inclusion criteria. Application of the QTE hypothesis may facilitate further research on determining the critical risk factor exposure levels associated with ASD may permit an elaboration of a quantitative threshold exposure level that mathematically evaluates the relative additive or synergistic combinations of risk factors to define a prognostic risk factor profile that can be used to calculate the odds of ASD as a predictive clinical assessment tool. Thus, the QTE hypothesis may represent a first step in defining a preventive paradigm to protect the critical stages of brain development affected in ASD.
References
- Kanner L (1943) Autistic disturbances of affective contact. Nervous Child 2:217–250.
- Division of Birth Defects (2014) National Center on Birth Defects and Developmental Disabilities 2012. Autism spectrum disorders: data and statistics. Centers for Disease Control and Prevention.
- Stoltenberg C, Schjølberg S, Bresnahan M, Hornig M, Hirtz D, et al. (2010) The Autism Birth Cohort: a paradigm for gene-environment-timing research. Mol Psychiatry 15: 676-680.
- Dietert RR, Dietert JM (2008) Potential for early-life immune insult including developmental immunotoxicity in autism and autism spectrum disorders: focus on critical windows of immune vulnerability. J Toxicol Environ Health B?Crit Rev 11: 660-680.
- Yunginger JW, Reed CE, O'Connell EJ, Melton LJ 3rd, O'Fallon WM, et al. (1992) A community-based study of the epidemiology of asthma. Incidence rates, 1964-1983. Am Rev Respir Dis 146: 888-894.
- Osman M, Tagiyeva N, Wassall HJ, Ninan TK, Devenny AM, et al. (2007) Changing trends in sex specific prevalence rates for childhood asthma, eczema, and hay fever. PediatrPulmonol 42: 60-65.
- Williams JG, Higgins JP, Brayne CE (2006) Systematic review of prevalence studies of autism spectrum disorders. Arch Dis Child 91: 8-15.
- Galley J (2014) Stay-at-home mothers through the years. Monthly Labor Rev.
- Bell DM, Gleiber DW, Mercer AA, Phifer R, Guinter RH, et al. (1989) Illness associated with child day care: a study of incidence and cost. Am J Public Health 79: 479-484.
- Hurwitz ES, Gunn WJ, Pinsky PF, Schonberger LB (1991) Risk of respiratory illness associated with day-care attendance: a nationwide study. Pediatrics 87: 62-69.
- Shay DK, Holman RC, Newman RD, Liu LL, Stout JW, et al. (1999) Bronchiolitis-associated hospitalizations among US children, 1980-1996. JAMA 282: 1440-1446.
- Hagerhed-Engman L, Bornehag CG, Sundell J, Aberg N (2006) Day-care attendance and increased risk for respiratory and allergic symptoms in preschool age. Allergy 61: 447-453.
- Dogaru CM, Nyffenegger D, Pescatore AM, Spycher BD, Kuehni CE (2014) Breastfeeding and childhood asthma: systematic review and meta-analysis. Am J Epidemiol 179: 1153-1167.
- Heberling CA, Dhurjati PS, Sasser M (2013) Hypothesis for a systems connectivity model of autism spectrum disorder pathogenesis: links to gut bacteria, oxidative stress, and intestinal permeability. Med Hypotheses80: 264-270.
- Jo H, Schieve LA, Sharma AJ (2015) Maternal prepregnancy body mass index and child psychosocial development at 6 years of age. Pediatrics 2015.
- Feig DS, Hwee J, Shah BR, Booth GL, Bierman AS, et al. (2014) Trends in incidence of diabetes in pregnancy and serious perinatal outcomes: a large, population-based study in Ontario, Canada, 1996-2010. Diabetes Care 37: 1590-1596.
- (2012) Substance abuse and mental health services administration mental health, United States12: 4681.
- Passey ME, Sanson-Fisher RW, D'Este CA, Stirling JM (2014) Tobacco, alcohol and cannabis use during pregnancy: clustering of risks. Drug Alcohol Depend 134: 44-50.
- Shabani M, Mahnam A, Sheibani V, Janahmadi M (2014) Alterations in the intrinsic burst activity of Purkinje neurons in offspring maternally exposed to the CB cannabinoid agonist WIN 55212-2. J MembrBiol 247: 63-72.
- Siniscalco D, Sapone A, Giordano C, Cirillo A, de Magistris L, et al. (2013) Cannabinoid receptor type 2, but not type 1, is up-regulated in peripheral blood mononuclear cells of children affected by autistic disorders. J Autism DevDisord 43: 2686-2695.
- Cutando L, Busquets-Garcia A, Puighermanal E, Gomis-González M, Delgado-García JM, et al. (2013) Microglial activation underlies cerebellar deficits produced by repeated cannabis exposure. J Clin Invest 123: 2816-2831.
- Tortoriello G, Morris CV, Alpar A, Fuzik J, Shirran SL, et al. (2014) Miswiring the brain: Δ9-tetrahydrocannabinol disrupts cortical development by inducing an SCG10/stathmin-2 degradation pathway. EMBO J 33: 668-685.
- Crawford S (2015) On the origins of autism: The Quantitative Threshold Exposure hypothesis. Med Hypotheses 85: 798-806.
Relevant Topics
- Adolescent Anxiety
- Adult Psychology
- Adult Sexual Behavior
- Anger Management
- Autism
- Behaviour
- Child Anxiety
- Child Health
- Child Mental Health
- Child Psychology
- Children Behavior
- Children Development
- Counselling
- Depression Disorders
- Digital Media Impact
- Eating disorder
- Mental Health Interventions
- Neuroscience
- Obeys Children
- Parental Care
- Risky Behavior
- Social-Emotional Learning (SEL)
- Societal Influence
- Trauma-Informed Care
Recommended Journals
Article Tools
Article Usage
- Total views: 16464
- [From(publication date):
February-2016 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 15384
- PDF downloads : 1080