Research Article Open Access
Influence of Postoperative Morbidity on Longterm Cancer Survival after Esophagogastric Resection
Eltweri AM*, Sharpe D, Nyasavajjala SM, Ubhi S and Bowrey DJUniversity Hospitals of Leicester, Leicester Royal Infirmary, Leicester, UK
- *Corresponding Author:
- Amar M Eltweri
Department of Surgery
Level 6 Balmoral Building
Leicester Royal Infirmary
Leicester, LE1 5WW, UK
Tel: (+44) 0116 258 5247
Fax: (+44) 0116 258 6083
E-mail: amar.eltweri@nhs.net
Received date: July 06, 2014; Accepted date: August 28, 2014; Published date: September 05 2014
Citation: Eltweri AM, Sharpe D, Nyasavajjala SM, Ubhi S, Bowrey DJ (2014) Influence of Postoperative Morbidity on Longterm Cancer Survival after Esophagogastric Resection. J Gastroint Dig Syst 4:216. doi: 10.4172/2161-069X.1000216
Copyright: © 2014 Eltweri AM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: Previous studies have shown that postoperative adverse events after colorectal resection predict a poor prognosis with early cancer relapse. The aim of this study was to report the outcome of patients undergoing esophagogastric resection to assess the influence of in-hospital factors on long-term cancer survival. Specifically, a standardized definition of complications was applied to this cohort and mortalities within the first 90 days were excluded from the analysis in order to remove any bias this would have.
Methods: Retrospective review of 304 patients undergoing curative esophagogastric resection for carcinoma during the period May 2003 to August 2011 at our institution. Minimum follow-up of 12 months was required; patients not surviving 90 days were excluded from the multivariate analysis.
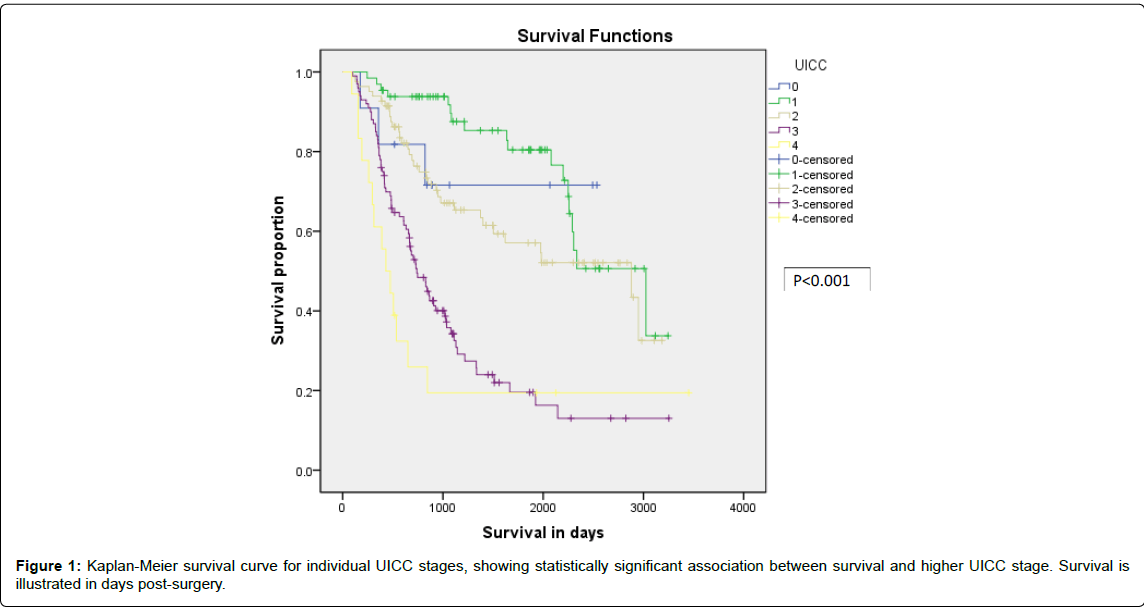
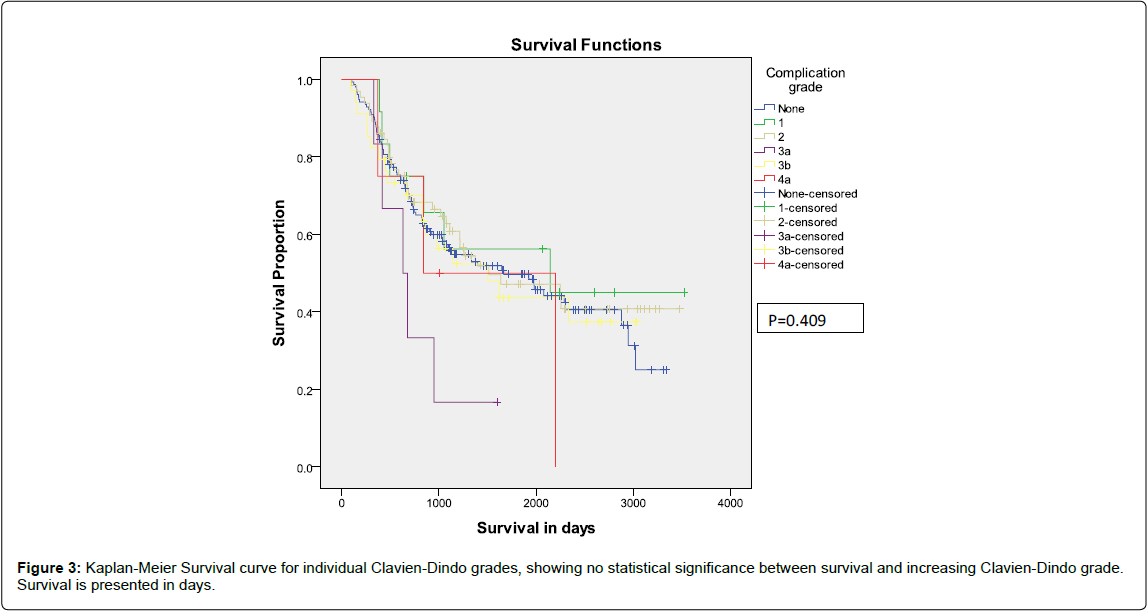
Results: The study population comprised 83 female and 221 male patients. Cell type was adenocarcinoma (n=274), squamous cell carcinoma (n=26) and small cell carcinoma (n= 4). Surgery comprised of oesophagectomy (n=168) and gastrectomy (n=136). The 30 and 90 day mortality were 22/304 (7%) and 28/304 (9%) respectively. A hundred and fifty six patients (51%) experienced an uneventful postoperative recovery with no complications, while 148 (49%) experienced complications. According to the Clavien-Dindo classification, complications occurred with the following frequency: grade I (n=13/304, 4%), grade II (n=68/304, 23%), grade IIIa (n=6/304, 2%), grade IIIb (n=47/304, 16%), grade IVa (n=10/304, 3%) and grade IVb (n=4/304, 1%). One hundred and sixty eight patient received neoadjuvant treatment as an initial treatment intent. On multivariate analysis, UICC stage was the only independent predictor of survival (P<0.001). The occurrence of postoperative complications were not significantly associated with longterm prognosis (p=0.409).
Conclusions: Patients experiencing postoperative morbidity can expect the same long-term oncologic outcome as those not suffering these early setbacks.
Keywords
Esophagogastric carcinoma, Adjuvant chemotherapy, Gastrointestinal stromal tumour
Introduction
Although there have been improvements in the perioperative care of patients undergoing surgery for esophagogastric carcinoma, 50-60% will suffer postoperative complications [1]. Technical complications, in particular anastomotic leak and infectious complications, notably nosocomial pneumonia account for the majority of these postoperative adverse events. While the development of these complications is associated with a threefold increase in mortality rate, the majority of patients are managed successfully, but have a prolongation to their period of hospitalization [1].
Large studies reporting on patients with colorectal carcinoma undergoing resection have identified a deleterious effect of anastomotic problems on longterm cancer survival [2,3]. These studies reported a 20% absolute reduction in overall five year survival, from 65% to 45% for patients suffering anastomotic leak compared to those not experiencing this adverse event [2,3].
A number of smaller studies have examined the potential relationship between perioperative outcome and cancer relapse [4-16], in patients undergoing esophagogastric resection. The findings have been conflicting, with seven of 13 studies reporting a significantly poorer longterm survival for those suffering postoperative complications compared to their counterparts, while six studies failed to identify a significant difference in survival. Only four of the studies employed a standardized definition of complications. Further, six of the seven studies reporting significant findings included patients experiencing in hospital mortality in the analysis. There is the potential for this to confound the interpretation.
The aim of the current study was to ascertain whether the longterm survival of patients experiencing postoperative complications after esophagogastric resection differed from patients with uneventful postoperative courses. Complications were defined by applying a validated, standardized classification (Clavien-Dindo) [17]. In order to avoid the bias of potential confounding early mortality, patients not surviving the first 90 days were excluded from the analysis.
Patients and Methods
The study population was patients undergoing resection for esophagogastric carcinoma at the University Hospitals of Leicester during the time May 2003 to August 2011. Patients were identified from the prospectively maintained Multidisciplinary team meeting records. Electronic and paper patient case records were retrieved and the following information extracted: demographic characteristics, neoadjuvant and adjuvant chemotherapy, operative details, postoperative course, resection specimen histology, the need for reintervention, length of hospital and intensive care unit stay, outcome according to most recent follow up. Patient follow up was reported to date of death or February 2013, meaning that the minimum follow up interval was 18 months.
Inclusion criteria were resection of esophagus or stomach for adenocarcinoma, squamous carcinoma or small cell carcinoma. Exclusion criteria were palliative resections and patients undergoing resection for gastrointestinal stromal tumour. Although recorded, patients not surviving 90 days were excluded from the survival analysis.
Postoperative complications were graded according to the Clavien- Dindo classification [17]. UICC stage was determined from the resection specimen histology. Stage 0 denoted a complete pathological response. Institutional approval for the study was granted by the University Hospitals of Leicester Clinical Audit and Effectiveness team. Patient consent was not a requirement.
Continuous data were compared using the student’s t-test, while comparison of proportions was by the X2 test. Survival was calculated by the Kaplan-Meier method, with comparisons by the log rank test. Cox regression analysis was conducted using forward variable selection. The data analysis software package SPSS version 19.0 (Chicago) was employed. Significance was assumed at the 5% level.
Results
The selection process for study population and patient characteristics are summarized in Table 1. The 30-day and 90-day mortality rates were 22/304 (7%) and 28/304 (9%) respectively. The causes of these early deaths were taken from hospital records or death certificates for out of hospital deaths. The causes included anastomotic leak (8 patients); pneumonia (7 patients); cardiac failure, myocardial infarction or pulmonary embolism (5 patients); multi-organ failure (4 patients); non-pneumonia sepsis (3 patients), and bleeding (one patient). These patients have been excluded from the subsequent analysis.
| No Complications (n=156) | Complications (n=148) | P value | |||
| Median Age (Years) | 66 | 66 | P=0.807 | ||
| Sex | Male | 102 | 119 | P=0.282 | |
| Female | 54 | 29 | P=0.008 | ||
| Tumour location | Oesophagus | 47 | 62 | P=0.353 | |
| OGJ | 38 | 38 | P=0.238 | ||
| Stomach | 71 | 47 | P=0.039 | ||
| Type of resection | Ivor Lewis esophagectomy | 59 | 69 | P=0.426 | |
| Transhiatal esophagectomy | 11 | 15 | P=0.556 | ||
| McKeown 3 stage Subtotal esophagectomy | 4 | 10 | P=0.180 | ||
| Gastrectomy | 82 | 54 | P=0.021 | ||
| Multivisceral resection | Spleen +/- Pancreas | 9 | 8 | ||
| Bowel | 3 | 0 | |||
| Gall Bladder | 4 | 4 | |||
| Other | 2 | 4 | |||
| UICC | Stage 0 | 5 | 6 | P=1.0 | |
| Stage I | 36 | 34 | P=0.812 | ||
| Stage II | 43 | 52 | P=0.470 | ||
| Stage III | 65 | 43 | P=0.053 | ||
| Stage IV | 7 | 13 | P=0.189 | ||
| Resection margin | R0 | 110 | 108 | P=0.892 | |
| R1 | 35 | 33 | P=1.0 | ||
| R2 | 11 | 7 | P=0.629 | ||
| LN Resection | Median LN resection (Range) | 16 (3-58) | 16 (1-64) | P=0.155 | |
| Positive | 1(1-23) | 1 (1-43) | |||
| Median operating time minutes (range) | 300 (90-540) | 345 (95-570) | P=0.194 | ||
| Median Hospital Stay in days (Range) | 13 (5-64) | 20 (3-172) | P<0.001 | ||
| Median ITU Stay in days (Range) | 2 (1-9) | 4 (1-56) | P<0.001 | ||
Table 1: Patients characteristics
One or more complications occurred in 148 (49%) of 304 patients. The most common non-surgical complications were pneumonia (n=57), cardiac arrhythmias (n=33) and acute renal failure (n=12). The most common surgical complications were anastomotic leak (n=19), chylothorax (n=12) and bleeding (n=9). Applying the Clavien-Dindo classification complications occurred with the following frequency: grade I (13 patients, 4%), grade II (68 patients, 23%), grade IIIa (6 patients, 2%), grade IIIb (47 patients, 16%), grade IVa (10 patients, 3%) and grade IVb (4 patients, 1%).
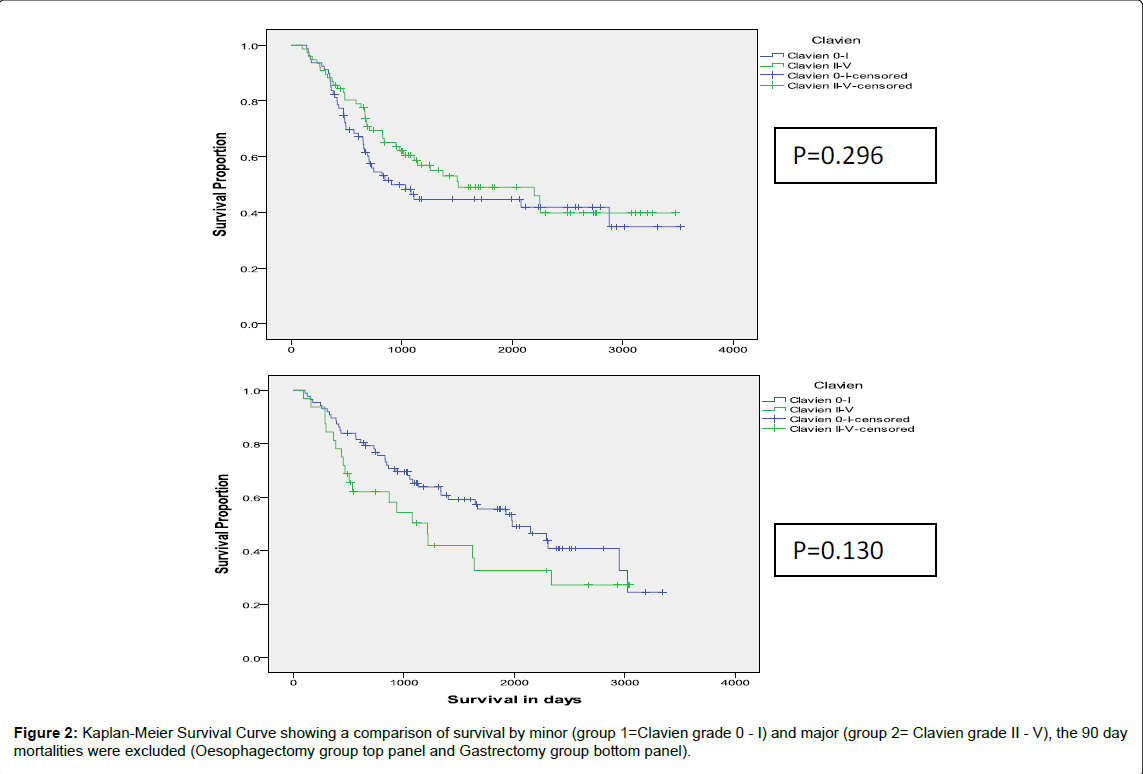
After excluding the 90 day mortalities, on multivariate analysis, UICC was the only independent factor significantly linked to survival (p<0.001), Figure 1. Neither the occurrence nor the grade of complication was significantly associated with survival after oesophagectomy and gastrectomy (Figures 2 and 3). The relative risk of mortality among the patients experiencing postoperative complications compared to those not experiencing complications was 1.0 (95% confidence interval 0.9- 1.2), p=0.41.
When the analysis was repeated including the 90 day mortalities, the occurrence of a postoperative complication was significantly associated with a shorter survival with a relative risk for mortality in the group experiencing complications compared to those not experiencing them of 1.6 (95% CI 1.3-2.1), p=0.002.
Discussion
Hirai et al. were the first to report on the influence of postoperative complications on longterm survival in patients undergoing esophagectomy [9]. In a study of 205 patients, 100 experienced an uneventful course, 58 patients experienced minor complications and 47 patients experienced major complications. The authors reported that the five year survivals of the three groups were 42%, 21% and 20% respectively. The authors speculated that the mechanism for this related to hypercytokinemia and suppressed immunoreactivity.
Since then, a further 12 reports have evaluated the relationship between postoperative complications and cancer survival after esophagogastric resection [1,5-7,9-12,16,18-21] (Table 2). Many of the studies included early postoperative mortality in the analysis. In the current study, when early mortality (within 90 days) was included in the analysis, a statistical correlation was noted between complications and overall survival. The studies reporting on the association between anastomotic leak and outcome in patients undergoing colorectal resection specifically excluded early deaths. For six of the seven studies reporting significantly poorer survival included early mortality in the analysis. Of the five studies that excluded early mortality from the analysis or performed analysis with and without this subgroup, only one reported a convincing association. The one remaining study by Rutegard et al. failed to identify an association on univariate analysis, but noted a weakly positive multivariate analysis, with a hazard ratio of 1.3 [11]. This coupled with the evidence from the current study suggests that, if there is an association between postoperative complications and early cancer relapse, the magnitude of the effect is at best small. As identified in the current study, it seems likely that UICC stage is the most powerful predictor of survival and that all other factors pale into insignificance by comparison.
It is also evident from Table 2 that there are widespread differences in the reporting of postoperative mortality, in hospital mortality ranging from 1%-11%, and 90 day mortality ranging from 1%-16%. The in hospital and 90 day mortality rates of 7% and 9% respectively in the current study are in keeping with those reported in National surveys in the literature. Studies from the Netherlands identified 6 month mortality rates after esophagectomy and gastrectomy of 7% and 10% respectively [22]. Funk et al., in an analysis of US Medicare data reported an in hospital mortality rate of 7% after esophagectomy [23]. Park et al. reported critical care and in hospital mortality rates of 4% and 11% respectively after esophagectomy [24,25].
| Author (year) | # | Compl % | Definition of complications | Early mortality | Early mortality in analysis | +ve or –ve study | Survival interval reported | Outcome for group with no complications vs those with complications |
| Hirai (1998) (9) | 205 | 56% | Minor and major | Ns | Yes | +ve (p<0.01) | 5 yr | 42% vs 21%/20% |
| Kinugasa (2004) (10) | 118 | 50% | Pulmonary | 7% InH | Both | +ve (p=0.03) HR 2.4 | 5 yr | 54% vs 33% |
| Mariette (2004) (1) | 386 | 36% | Prolonged hosp stay | 4% InH | Yes | -ve (p=0.33) | ns | ns |
| Rizk (2004) (5) | 510 | 27% | Technical | 6% InH | Yes | +ve (p<0.001) HR 1.4 | 1 yr 3 yr |
82% vs 58% 48% vs 31% |
| Ancona (2006) (12) | 522 | 16% | Surgical | 1% InH | Yes | -ve (p=0.90) | ns | ns |
| Ferri (2006) (16) | 434 | 23% | Technical | 5% InH | Both | -ve (p=0.35) | Median | 19 vs 14 months |
| Lerut (2009) (18) | 138 | 70% | Clavien grade 1-5 | 1% 90d | Yes | +ve (p=0.01) HR 4.5 | 3 yr | 62% vs 33% |
| Takeuchi (2009) (7) | 40 | ns | Ns | 5% InH | No | -ve | ns | ns |
| An (2012) (19) | 123 | 29% | Clavien grade 1-5 | 2% InH | Yes | +ve (p=0.004) HR 2.7 | 3 yr | 57% vs 27% |
| Carrott (2012) (30) | 285 | 50% | Accordion grade 1-5 | 1% InH | Yes | +ve (p=0.03) | Median | 1954 vs 1596 days |
| D’Annoville (2012) (20) | 405 | 56% | Clavien grade 1-4 | 11% InH 16% 90d |
Both | -ve (p=0.75/p=0.90) | 5 yr | 38% vs 47%/55% |
| Nagasako (2012) (21) | 400 | 9% | Anastomotic | 1% InH | Yes | +ve (p=0.009) HR 4.4 | 5 yr | 94% vs 81% |
| Rutegard (2012) (11) | 616 | 23% | Surgical | 8% 90d | Both | -ve on univariate, +ve on multivariate HR 1.3 | Median | 24 vs 23 months |
Table 2: Summary of literature reporting influence of postoperative complications on longterm survival after esophagogastric resection
Three articles have assessed complications after esophagogastric surgery from the reverse perspective. Comparison has been made between the clinical characteristics of those patients suffering early cancer relapse and those not suffering this fate. These identified a significantly higher frequency of postoperative complications in those suffering early cancer relapse [1,8,26].
The potential mechanism by which any effect might be exerted remains unclear. The most popularised views include the assertion that complications, notably those that require further intervention result in a state of relative immunosuppression. Other theories contend that patients suffering complications are more likely to require blood transfusion and that this is known to exert an immunosuppressive effect. A further potential mechanism is that, if cancer relapses develop from bone marrow derived progenitor cells, increased local permeability and aggregation of these cells will occur at sites of any inflammatory response. Lagarde et al. identified chylothorax as carrying the greatest hazard ratio [25]. This is appealing given the potential immunological consequences of lymphocyte and protein depletion, which occur with chyle leaks. The current study did not examine the influence of specific complications, although when these were divided into Clavien grade of complication, there was no trend evident.
The classification of postoperative complications becomes increasingly important as clinical outcomes comparisons become embedded in the quality assurance of the healthcare process and system. Ensuring that analogous information is collected between centers requires robust definitions of complications. In 1992 Clavien proposed a classification system for postoperative complications based upon the level of intervention required to correct or ameliorate the complications. The same group subsequently modified the classification in 2004 and validated its applicability to a large cohort in 2009. This grouping allows meaningful comparisons to be made between centers and between different surgical specialties [17]. Six studies have employed the Clavien-Dindo classification to report complications after esophagectomy or gastrectomy [18-20,27-30] (Table 3). The reported frequency of complications range from 51-70% for esophagectomy and 25-40% for gastrectomy.
| Frequency of individual Clavien-Dindo grade complications | ||||||||||
| Author | Op | # Patients in Study | % affected by any complication | 1 | 2 | 3a | 3b | 4a | 4b | 5 |
| Lerut (2009) (18) | E | 138 | 70% | 0% | 35% | 17% | 16% | 1% | ||
| Seely (2010) (27) | E/G | 51 | 53% | 4% | 57% | 10% | 16% | 16% | 0% | 0% |
| Montenovo (2011) (29) | E | 72 | 51% | 36% | 28% | 0% | 1% | 0% | 2% | 1% |
| An (2012) (19) | G | 123 | 29% | 5% | 9% | 14% | 0% | 2% | ||
| D’Annoville (2012) (20) | E | 384 | 57% | 2% | 15% | 18% | 16% | 11% | ||
| Lee (2012) (28) | G (open) | 629 | 40% | 28% | 7% | 4% | 0.5% | 0.5% | 0% | 1% |
| G (lap) | 1002 | 25% | 18% | 5% | 2% | 0.4% | 0% | 0% | 0% | |
Table 3: Published literature of postoperative complications using Clavien-Dindo classification.
In conclusion, this study demonstrated that patients who suffer postoperative morbidity can expect the same long term survival outcome among those survived the 90 days postoperative period, and the only survival predictor was the UICC stage. Employing the Clavien- Dindo classifications of surgical complication is an ideal method of reporting postoperative complications and will allow accurate worldwide comparison of these postoperative setbacks.
References
- Mariette C, Taillier G, Van Seuningen I, Triboulet JP (2004) Factors affecting postoperative course and survival after en bloc resection for esophageal carcinoma. Ann Thorac Surg 78: 1177-1183.
- Ptok H, Marusch F, Meyer F, Schubert D, Gastinger I, et al. (2007) Impact of anastomotic leakage on oncological outcome after rectal cancer resection. Br J Surg 94: 1548-1554.
- McArdle C, McMillan DC, Hole DJ (2005) Impact of anastomotic leakage on long-term survival of patients undergoing curative resection for colorectal cancer. Br J Surg 92: 1150-1154.
- Sierzega M, Kolodziejczyk P, Kulig J; Polish Gastric Cancer Study Group (2010) Impact of anastomotic leakage on long-term survival after total gastrectomy for carcinoma of the stomach. Br J Surg 97: 1035-1042.
- Rizk NP, Bach PB, Schrag D, Bains MS, Turnbull AD, et al. (2004) The impact of complications on outcomes after resection for esophageal and gastroesophageal junction carcinoma. J Am Coll Surg 198: 42-50.
- Carrott PW, Markar SR, Kuppusamy MK, Traverso LW, Low DE (2012) Accordion severity grading system: assessment of relationship between costs, length of hospital stay, and survival in patients with complications after esophagectomy for cancer. J Am Coll Surg 215: 331-336.
- Takeuchi H, Saikawa Y, Oyama T, Ozawa S, Suda K, et al. (2010) Factors influencing the long-term survival in patients with esophageal cancer who underwent esophagectomy after chemoradiotherapy. World J Surg 34: 277-284.
- Lagarde S, de Boer JD, ten Kate FJ, Busch OR, Obertop H, et al. (2008) Postoperative complications after esophagectomy for adenocarcinoma of the esophagus are related to timing of death due to recurrence. Ann Surg 247: 71-76.
- Hirai T, Yamashita Y, Mukaida H, Kuwahara M, Inoue H, et al. (1998) Poor prognosis in esophageal cancer patients with postoperative complications. Surg Today 28: 576-579.
- Kinugasa S, Tachibana M, Yoshimura H, Ueda S, Fujii T, et al. (2004) Postoperative pulmonary complications are associated with worse short- and long-term outcomes after extended esophagectomy. J Surg Oncol 88: 71-77.
- Rutegård M, Lagergren P, Rouvelas I, Mason R, Lagergren J (2012) Surgical complications and long-term survival after esophagectomy for cancer in a nationwide Swedish cohort study. Eur J Surg Oncol 38: 555-561.
- Ancona E, Cagol M, Epifani M, Cavallin F, Zaninotto G, et al. (2006) Surgical complications do not affect longterm survival after esophagectomy for carcinoma of the thoracic esophagus and cardia. J Am Coll Surg 203: 661-669.
- Memon MA, Subramanya MS, Khan S, Hossain MB, Osland E, et al. (2011) Meta-analysis of D1 versus D2 gastrectomy for gastric adenocarcinoma. Ann Surg 253: 900-911.
- Kosugi S, Kanda T, Yajima K, Ishikawa T, Hatakeyama K (2011) Risk factors that influence early death due to cancer recurrence after extended radical esophagectomy with three-field lymph node dissection. Ann Surg Oncol 18: 2961-2967.
- Karl RC, Schreiber R, Boulware D, Baker S, Coppola D (2000) Factors affecting morbidity, mortality, and survival in patients undergoing Ivor Lewis esophagogastrectomy. Ann Surg 231: 635-643.
- Ferri LE, Law S, Wong KH, Kwok KF, Wong J (2006) The influence of technical complications on postoperative outcome and survival after esophagectomy. Ann Surg Oncol 13: 557-564.
- Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, et al. (2009) The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg 250: 187-196.
- Lerut T, Moons J, Coosemans W, Van Raemdonck D, De Leyn P, et al. (2009) Postoperative complications after transthoracic esophagectomy for cancer of the esophagus and gastroesophageal junction are correlated with early cancer recurrence: role of systematic grading of complications using the modified Clavien classification. Ann Surg 250: 798-807.
- An JY, Kim KM, Kim YM, Cheong JH, Hyung WJ, et al. (2012) Surgical complications in gastric cancer patients preoperatively treated with chemotherapy: their risk factors and clinical relevance. Ann Surg Oncol 19: 2452-2458.
- D'Annoville T, D'Journo XB, Trousse D, Brioude G, Dahan L, et al. (2012) Respiratory complications after oesophagectomy for cancer do not affect disease-free survival. Eur J Cardiothorac Surg 41: e66-73.
- Nagasako Y, Satoh S, Isogaki J, Inaba K, Taniguchi K, et al. (2012) Impact of anastomotic complications on outcome after laparoscopic gastrectomy for early gastric cancer. Br J Surg 99: 849-854.
- Dikken JL, Dassen AE, Lemmens VE, Putter H, Krijnen P, et al.(2012) Effect of hospital volume on postoperative mortality and survival after oesophageal and gastric cancer surgery in the Netherlands between 1989 and 2009. Eur J Cancer 48 : 1004-1013.
- Funk LM, Gawande AA, Semel ME, Lipsitz SR, Berry WR, et al. (2011) Esophagectomy outcomes at low-volume hospitals: the association between systems characteristics and mortality. Ann Surg 253: 912-917.
- Park DP, Welch CA, Harrison DA, Palser TR, Cromwell DA, et al. (2009) Outcomes following oesophagectomy in patients with oesophageal cancer: a secondary analysis of the ICNARC Case Mix Programme Database. Crit Care 13 Suppl 2: S1.
- Lagarde SM, Omloo JM, de Jong K, Busch OR, Obertop H, et al. (2005) Incidence and management of chyle leakage after esophagectomy. Ann Thorac Surg 80: 449-454.
- Sierzega M, Kolodziejczyk P, Kulig J; Polish Gastric Cancer Study Group (2010) Impact of anastomotic leakage on long-term survival after total gastrectomy for carcinoma of the stomach. Br J Surg 97: 1035-1042.
- Seely AJ, Ivanovic J, Threader J, Al-Hussaini A, Al-Shehab D, et al. (2010) Systematic classification of morbidity and mortality after thoracic surgery. Ann Thorac Surg 90: 936-942.
- Lee JH, Park do J, Kim HH, Lee HJ, Yang HK (2012) Comparison of complications after laparoscopy-assisted distal gastrectomy and open distal gastrectomy for gastric cancer using the Clavien-Dindo classification. Surg Endosc 26: 1287-1295.
- Montenovo MI, Chambers K, Pellegrini CA, Oelschlager BK (2011) Outcomes of laparoscopic-assisted transhiatal esophagectomy for adenocarcinoma of the esophagus and esophago-gastric junction. Dis Esophagus 24: 430-436.
- Carrott PW, Markar SR, Kuppusamy MK, Traverso LW, Low DE (2012) Accordion severity grading system: assessment of relationship between costs, length of hospital stay, and survival in patients with complications after esophagectomy for cancer. J Am Coll Surg 215: 331-336.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 14138
- [From(publication date):
August-2014 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 9522
- PDF downloads : 4616