Intraoral Dermoid Cyst-How Common are they in a Paediatric Population? A Retrospective Case Series
Received: 09-Sep-2019 / Accepted Date: 17-Oct-2019 / Published Date: 24-Oct-2019 DOI: 10.4172/2161-119X.1000382
Abstract
Oral dermoid cysts are rare especially in the paediatric population. They can rapidly enlarge causing dysphagia and airway compromise. We present a case series of paediatric oral dermoid cysts in our centre over the past 5 years and suggest a predisposition to tongue tie procedures. All our cases required surgical intervention and we suggest that all clinicians consider this important diagnosis when presented with a child with an intraoral swelling.
Keywords: Paediatric; Oral cavity; Dermoid cyst
Introduction
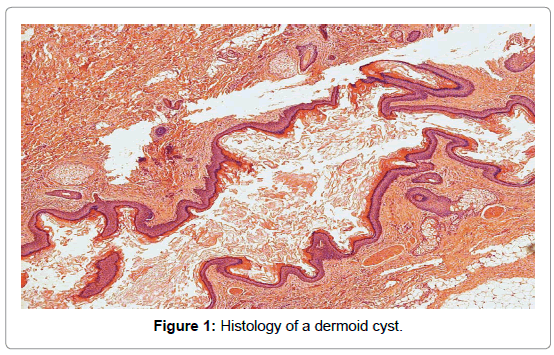
Dermoid cysts are benign developmental cysts lined by epidermislike epithelium, typically containing dermal adnexal structures such as hair follicles and sebaceous glands [1]. They are histologically differentiated from epidermoid cysts which lack adnexal structures, and teratoid cysts, which contain tissue from all three germinal layers [2] (Figure 1).
Dermoid cysts may be congenital or acquired. Postulated theories for pathogenesis include entrapment of dermal elements during midline fusion of the first and second branchial arches, variants of thyroglossal duct cysts, and cysts arising from the tuberculum impar of his. Acquired cysts are thought to occur post trauma [3].
Floor of mouth dermoid cysts are rare, accounting for between 1.6 and 6.5% of all dermoid cysts, and between 23 and 34% of dermoids in the head and neck region [4]. They comprise only 0.01% of all oral lesions within the paediatric population. Over a 22-year period of study at the Mayo clinic in 2005, there were no reported cases of paediatric intra oral dermoid cysts [5]. The highest incidence occurs in the adult population, usually second and third decade of life, with no gender predilection [6].
They typically present as slow growing midline, asymptomatic masses. A sublingual cyst (52%) usually develops above mylohyoid, and may cause swelling and tongue displacement. Below mylohoid, a submental swelling (26%) may manifest as a “double chin” appearance [7]. Complications of dermoids include dysphonia, dysphagia, and dyspnoea, with airway compromise [8]. Radiologically, these lesions are difficult to diagnose.
We present a case series spanning 5 years of paediatric patients with intraoral dermoid cysts, which to our knowledge, is the first in the UK.
Retrospective Case Series
A retrospective search was conducted between 01/01/2013 and 18/10/2018, of paediatric patients with histologically confirmed dermoid cysts following excision performed at Imperial College Healthcare NHS trust, UK. Electronic patient notes were then reviewed.
The search generated 106 paediatric patients of which 3 had intra oral dermoid cysts. We outline 2 cases, details regarding our final and most recent case can be found in the references [9].
Case 1
A 15-year-old male presented with a one year history of left sided floor of mouth and submandibular swelling (level 1). He noted a left sided neck mass when tensing the muscles in his neck, and on swallowing. It slowly enlarged but never caused airway difficulties or dysphagia. No previous tongue tie release was noted. A Magnetic Resonance Imaging (MRI) scan of the neck revealed a 6 cm cystic mass within the sublingual space on the left, extending from the midline anteriorly, to the posterior border of mylohyoid, likely to be a ranula. An additional Ultrasound (US) reported the mass as a plunging ranula, likely to be from submandibular gland. During the operation, a submandibular incision was performed; the lesion was deep to the submandibular gland, the parapharyngeal space and floor of the mouth. It was superficial to the hyoglossus, but infiltrated between the geniohyoid and the genioglossus muscles. There was no breach to the floor of the mouth, and the lesion was confirmed to be a dermoid cyst.
Case 2
A 2-year-old boy presented with a left sided sublingual swelling leading to three admissions due to dysphagia. It fluctuated in size over an 18-month period following a tongue-tie release at the age of 8 months. Initially, there was posterior displacement of the tongue and a punctum in the submental region. A US of the neck revealed a 3 × 3 cm homogeneous hypoechoic well-defined mass in the floor of the mouth, suggesting infection or haemorrhage into a cyst. An MRI scan confirmed a cystic lesion in the floor of the mouth and root of tongue above the mylohyoid, suggestive of a dermoid/epidermoid cyst. A differential diagnosis included a draining sinus, due to repeated infections. Thus, surgery was planned on a semi-urgent basis and he was given antibiotics and steroids during his inpatient stay. Four months after his initial presentation, the swelling enlarged acutely over 4 days, causing dysphagia. He had a repeat US of the neck which showed further enlargement of the midline floor of mouth cystic lesion, initially thought to represent a floor of mouth sialocele, with a midline fistula to the skin and apparent transection with retraction of the geniohyoid muscles. These muscles appeared as a stump abutting the anterior inferior aspect of the swelling that was thought to be accidentally transected during previous attempted tongue-tie procedure. However, upon review and discussion in our multi-disciplinary team meeting, the cyst appeared smooth on repeat ultrasound, likely representing a dermoid/epidermoid cyst with fistulation to the submental skin. Furthermore, it was thought that the tongue tie procedure, which was performed whilst the child was in Syria, may have been performed mistakenly. The tongue was displaced by a congenital floor of mouth cyst all along rather than it appearing to be a tongue-tie. Again, he was planned for urgent planned theatre after antibiotics and steroids. During the procedure, a submental approach was used as a punctum was identified and excised with an elliptical incision, with the tract being followed in entirety to the floor of the mouth. A multi-loculated cyst was present with significant fibrosis due to the previous episodes of infection. The lesion breached mylohyoid and splayed the geniohyoid open. A breach to the floor of the mouth was necessary in order to wholly excise this lesion. He recovered well and histopathology reported a dermoid cyst.
Discussion
Over a five-year period at our tertiary paediatric ENT centre, we have diagnosed and treated, three complex paediatric cases of intraoral dermoid. Of note, two out of three had previous tongue tie release. We extended the search to find adults with intraoral dermoid cysts treated at out institution over the same period and this did not yield any cases. A literature search was undertaken to ascertain whether tongue-tie surgery predisposes to cyst or abscess development. There is no known documented link. We postulate iatrogenic inclusion of epithelial cells following tongue-tie release surgery, predisposing to the development of dermoid cysts.
Of the three intra-oral cases, the two younger patients presented with dysphagia. The youngest of the children deteriorated and developed airway compromise [9]. Due to the smaller size of the oral cavity in children, clinicians should have a higher clinical index of suspicion, and initiate definitive management promptly including surgical intervention or intubation to stabilise the airway.
Managing floor of mouth masses can be challenging due to the complex anatomy and vast array of pathological processes which can affect the area. Whilst some masses are unique to this region (eg. submandibular gland pathology or ranula), uncommon entities such a dermoid cysts can quite easily be overlooked. Furthermore, imaging alone may not be able to distinguish between lesions. Radiologically it is very difficult to differentiate between a dermoid cyst confined within the sublingual space, and a ranula [8]. This is evidenced by Diercks et al. who reported the recurrence of a dermoid cyst treated twice by marsupialisation as it was misdiagnosed previously for a ranula [10].
Differential diagnoses in our cases were a ranula or lymphovascular malformation. Ranulas are mucous extravasation cysts originating from sublingual glands. They have an estimated prevalence of 0.2 in 1000, in the paediatric population. Management is variable depending on clinical presentation/symptoms and cosmesis. Treatments include ongoing observation, aspiration and review, or formal planned surgical excision [11].
Lymphovascular malformations generally develop before the age of two. The preferred method of treatment is most commonly sclerotherapy [12]. Surgical intervention is generally reserved for cases where complications arise such as macroglossia [13]. Therefore, a thorough clinical assessment must be undertaken to prevent diagnostic delay and sequelae of incorrect treatment or future complications.
Tongue abscesses are a rare but potentially life threating clinical entity. The muscularity and abundant vascular and lymphatic supply of the tongue provides protection as well as the immunological properties of saliva [14]. Most reported cases originate from the developing world and are commonly attributed to poor oral hygiene [15]. Over the last 30 years, roughly 50 cases have been published [16]. There is no known predilection for gender, and adults between 30–50 years have most frequently been affected. Only a few paediatric cases have been reported [15]. Varghese et al. reported a tongue abscess following incisor extraction. Of note, this gentleman had a previous tongue-tie release during his childhood [17].
US is often the primary diagnostic modality of choice. Dermoid cysts appear as unilocular cysts, which are well circumscribed with anechoic, hypoechoic or multiple echogenic regions representing skin appendages [2]. MRI is considered the gold standard for diagnosing cystic masses as it characterises the anatomy of the floor of the mouth due to its multiplanar imaging capabilities and soft tissue contrast enhancement. Despite this being the case, Computed Tomography (CT) is more readily available and most commonly the go to imaging modality in the UK. The “sack of marbles” sign or intracystic floating corpuscles which may be calcified, is pathognomic for dermoid cysts. They are usually hypodense on CT and, hypo/hyperintense on T1 weighted MRI and hypointense on T2-weighted MR scans [18].
Conclusion
We have presented three paediatric cases of intraoral dermoid cysts over a 5-year period. There were no adult cases emphasising the rarity. It is important to manage these patients using a multidisciplinary approach, including a review by SLT/dietetics team if indicated.
We are the first, to our knowledge, to suggest a possible predisposition to development of dermoid cysts following tongue tie procedures.
Definitive management of dermoid cysts is by formal surgical excision. An intraoral approach is employed for small cysts above the geniohyoid muscle. Those that are below the muscle or very large, require an extra-oral approach, as exemplified in our case above [1].
Acknowledgements
We would like to thank our paediatric intensive care, speech and language and dietetic team at St Mary’s Hospital for their continued support when caring for these patients. We would also like to thank the families involved in these cases for allowing us to educate the ENT community with their personal cases.
Conflict of Interest
There has been no conflict of interest within this paper.
References
- Dillon JR, Avillo AJ, Nelson BL (2015) Dermoid cyst of the floor of the mouth. Head Neck Pathol 9: 376-378.
- Patel H, Mayl J, Chandra B, Pritchett C, Chandra T (2016) Dermoid of the oral cavity: case report with histopathology correlation and review of literature. J Radiol Case Rep 10: 19-27.
- Bonet-Coloma C, MÃnguez-MartÃnez I, Palma-Carrió C, Ortega-Sánchez B, Peñarrocha-Diago M, et al. (2011) Orofacial dermoid cysts in pediatric patients: a review of 8 cases. Med Oral Patol Oral Cir Bucal 16: e200-e203.
- Pryor SG, Lewis JE, Weaver AL, Orvidas LJ (2005) Pediatric dermoid cysts of the head and neck. Otolaryngol Head Neck Surg 132: 938-942.
- Palaskar SJ, Garde J, Bartake A, Narang B (2014) Teratoid cyst of the oral cavity: a rare entity. J Oral Maxillofac Pathol 18: 469-471.
- Teszler CB, El-Naaj IA, Emodi O, Luntz M, Peled M (2007) Dermoid cysts of the lateral floor of the mouth: a comprehensive anatomo-surgical classification of cysts of the oral floor. J Oral Maxillofac Surg 65: 327-332.
- Koeller KK, Alamo L, Adair CF, Smirniotopoulos JG (1999) From the Archives of the AFIP: Congenital cystic masses of the neck: Radiologic-pathologic correlation. Radiographics 19: 121-46.
- Bhalla S, Acharya V, Ally M, Taghi A (2019) Acute presentation of an intraoral dermoid cyst causing airway compromise in a young child. BMJ Case Rep 12: e228421.
- Diercks GR, Iannuzzi RA, McCowen K, Sadow PM (2013) Dermoid cyst of the lateral neck associated with the thyroid gland: a case report and review of the literature. Endocr Pathol 24: 45-48.
- Mneimneh S, Barazi R, Rajab M (2016) A rare case of congenital ranula in an infant. Case Rep Otolaryngol 2016: 5874595.
- Lee BB, Do YS, Byun HS, Choo IW, Kim DI, et al. (2003) Advanced management of venous malformation with ethanol sclerotherapy: mid-term results. J Vasc Surg 37: 533-538.
- Lahiri A, Kok K, Sharp I, Nishikawa H (2006) Acute exacerbation of macroglossia leading to necrosis of the anterior third of the tongue. J Plast Reconstr Aesthet Surg 59: 871-873.
- Kulkarni CD, Verma AK, Kanaujia R (2013) A rare case of hemilingual abscess in a 17-year-old girl: the ease of ultrasound and the advantage of MRI. Jpn J Radiol 31: 491-495.
- Tajudeen BA, Lanson BG, Roehm PC (2011) Glossal abscess as a complication of tongue-base suspension surgery. Ear Nose Throat J 90: E15-E17.
- Kuge R, Komori K, Miyama S (2017) Recurrent lingual abscess in a child. Pediatr Infect Dis J 36: 694-695.
- Varghese L, Agarwal P, Rupa V (2013) Unusual complication of dental extraction: Lingual abscess. Indian J Dent Res 24: 772-774.
- Giarraputo L, Savastano S, D'Amore E, Baciliero U (2018) Dermoid cyst of the floor of the mouth: diagnostic imaging findings. Cureus 10: e2403.
Citation: Bhalla S, Acharya V, Ally M, Slovick A, Taghi A et al. (2019) Intraoral Dermoid Cyst-How Common are they in a Paediatric Population? A Retrospective Case Series. Otolaryngol (Sunnyvale) 9:382. DOI: 10.4172/2161-119X.1000382
Copyright: © 2019 Bhalla S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 3320
- [From(publication date): 0-2019 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 2447
- PDF downloads: 873