Leiomyosarcoma of the Breast: A Case Report
Received: 14-Sep-2021 / Accepted Date: 28-Sep-2021 / Published Date: 05-Oct-2021 DOI: 10.4172/2167-7964.1000343
Abstract
Leiomyosarcoma is a rare type of malignancy that begins in smooth muscle tissue and primarily presents in patients between the age of 24 and 86-years old. Leiomyosarcoma of the breast is a significantly unreported manifestation of stromal sarcomas, with fewer than twenty cases being reported globally. We present a case of a 45-year-old female with hepatic, left renal and multiple bone metastases that presented with a suspicious mass in the left breast following a routine mammogram. The combination of angular and speculated tumor margins warranted additional investigation in the form of an ultrasound and subsequent biopsy. When a patient has a history of leiomyosarcoma and metastatic lesions, further investigation should always be considered if suspicious findings are noted in routine examinations.
Keywords: Leiomyosarcoma; Breast; Metastases; Liver lesions; CT scan; Mammogram
Introduction
Stromal sarcomas of the breast account for an estimated 1% of all malignant tumor of the breast and less than 5% of all soft tissue sarcomas. Leiomyosarcoma are one of the most prominent subtypes of stromal sarcoma, accounting for an estimated 25% of all sarcomas, and arises from the embryonic mesoderm of patients. Leiomyosarcoma primarily originates directly from the smooth muscle; however, several cases have noted origination from the precursor mesenchymal stem cells, eventually differentiating into smooth muscle cells [1]. The typical age of presentation is between 24-86 years old, most commonly in females, with the tumor tending to exhibit as a large mass. Leiomyosarcoma of the breast are even rarer, with the current literature presenting less than twenty cases in total [2]. In these cases, tumor primarily originate from the smooth muscle of the nipple-areolar complex and present as firm, well circumscribed, lobulated masses.
Treatment for this neoplasm relies on surgical intervention, with literature detailing this to be the only curative approach available. However, recent advances in neo adjuvant therapy, including anthracycline/ifosfamide, have found these chemotherapeutics to be effective in patients with high-risk sarcomas [3,4]. A previous case report, with a similar presentation to that detailed in this report, described this neo adjuvant chemotherapy for aggressive soft tissue sarcomas [5]. However, the rarity of breast leiomyosarcoma poses a significant challenge to treatment evaluation, halting the generalized application of this approach.
We present a case of a 45-year-old female patient with a history of metastatic leiomyosarcoma, presenting with suspicious lesions in the breast tissue following a routine mammogram. Further investigation by ultrasound and biopsy confirmed a pathologic diagnosis of leiomyosarcoma of the breast.
Case Presentation
A 45-year-old female presented with a history of persistent pain in the left lumbar region, since 2010. She was found to have a 14 cm lumbar soft tissue mass in October 2013 on imaging, subsequently undergoing resection, in addition to a nephrectomy of one kidney. The patient was diagnosed with angiolymphatic invasion absent, high grade leiomyosarcoma. It is worth noting that the patient’s lymph nodes were not resected and the actual tumor dimension was 5.5 cm. Radiation treatment for this tumor was completed on February 7th, 2014
In September 2014, surveillance CT imaging demonstrated no evidence of recurrent disease. A follow-up CT scan in January 2015 revealed a 5 cm liver lesion with an adjacent 2 cm liver lesion. Her CT chest, abdomen, and pelvis findings did not note any other sites of disease. In contrast to her previous presentation, this patient was completely asymptomatic. In February 2015, the patient had a partial hepatectomy, with a post-operative CT revealing no evidence of residual disease. The pathologic diagnosis of this patient is noted in Table 1. The patient was started on gemzar/taxotere, with no evidence of disease present in a CT scan after the fourth cycle. However, after the fifth cycle, she began feeling nauseated, severely fatigued, with lower extremity edema; hence chemotherapy was stopped. A CT scan in September 2015 revealed small liver lesions, with subsequent liver MRI demonstrating these lesions to be too small for a definitive metastasis diagnosis. Bone lesions were also identified, but bone scans were negative (Table 1).
| Intervention | Pathologic Diagnosis |
|---|---|
| Gallbladder, cholecystectomy Liver, segment 7 mass, partial hepatectomy |
Chronic cholecystitis Metastatic leiomyosarcoma, resection margin focally positive |
| Liver, segment 3 mass, partial hepatectomy | Metastatic leiomyosarcoma, negative resection margin |
| Liver, new resection margin, wedge biopsy | Negative for metastasis, negative resection margin |
Table 1: Pathologic diagnosis following intervention.
The patient’s liver lesions persisted but were too small to characterize until April 2016. At that time, a larger liver lesion was observed, in addition to a new lesion superior to the previous one. In the same month, the patient was diagnosed with recurrent leiomyosarcoma and was scheduled for resection of the liver lesions. The larger mass and smaller dominant mass in segment four, as well as two 1cm masses in segments 5 and 8, was resected. The patient’s right sided lesions were treated with radiofrequency ablation (RFA), with the patient recovering well from her surgery and RFA. Following surgery, she was started on further rounds of chemotherapy, variant, in June 2016. Her dose was initially reduced to 600 mg due to hypertension before being further reduced to 400 mg for proteinuria. Liver function tests were largely elevated, warranting a two week break from chemotherapy, which was restarted once these measures improved.
A routine CT abdomen revealed spinal lesions at L3 lesion, despite the patient experiencing no focal pain and the bone scan being negative. It is worth noting that the patient did report occasional numbness in the left gluteal region. However, in September of 2016 a follow up CT demonstrated an increase in the size of the L3 lesion, which was now sclerotic compared to scans carried out two years prior, before starting votrient. Hence, an MRI was requested, which revealed findings highly suggestive of bone metastasis with areas of healing. The patient was referred to radiation oncology to complete her radiation therapy.
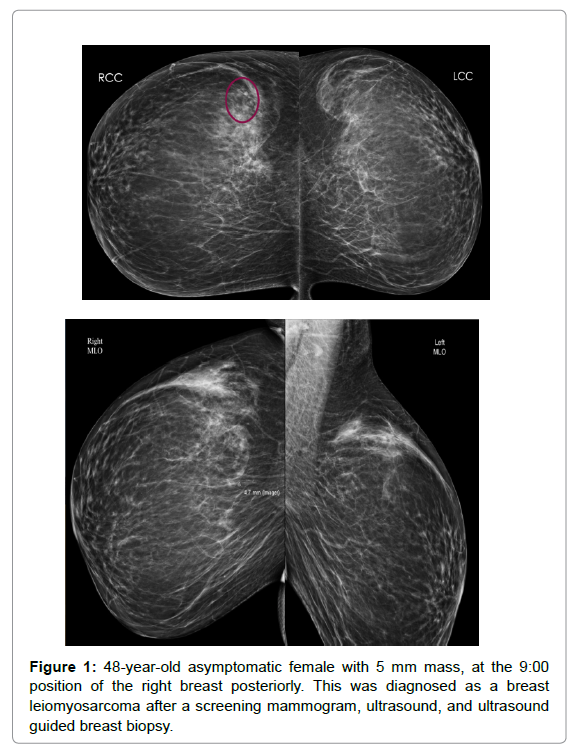
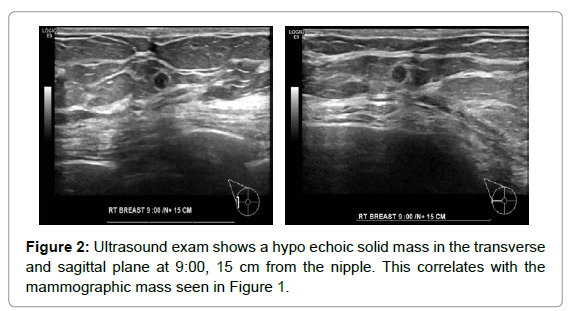
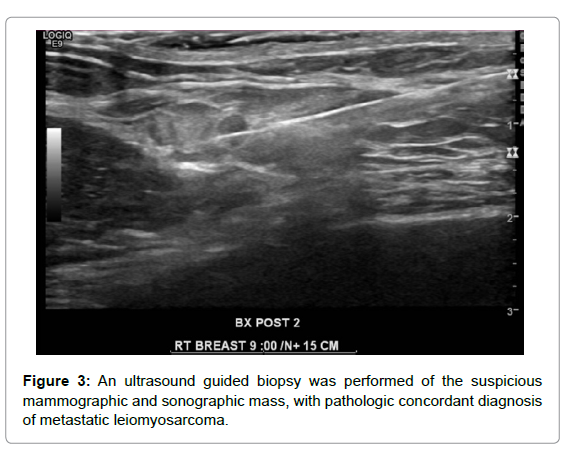
A routine screening mammogram revealed a 5 mm right breast mass (Figure 1). Diagnostic workup revealed speculated margins, warranting a biopsy recommendation (Figure 2). Pathology found the patient’s tumor to be morphologically similar to her known metastatic retroperitoneal leiomyosarcoma to the liver, corroborating a positive diagnosis for leiomyosarcoma. The patient felt well and had no new changes to her chronic lower back pain (Figures 1-3).
Discussion
Primary leiomyosarcoma of the breast is extremely rare, despite the increasing incidence of leiomyosarcoma diagnosis in practice. Diagnosis preoperatively should be made by ultrasound guided core needle biopsy. Once a preoperative diagnosis is achieved, a wide resection should be the first line of treatment. There is no need for an axillary lymph node dissection [6]. Postoperatively, there are two curative approaches; in patients with chemo sensitive tumor, additional adjuvant chemotherapy should be administered to treat any underlying micro metastatic disease; and in patients with a tumor larger the 5 cm or in those with positive surgical margins, radiation therapy should be employed to improve local control [7]. Regarding morphology and immunohistochemistry, primary and secondary breast leiomyosarcoma presentation is identical. Therefore, a thorough work-up is necessary secondary to diagnoses to exclude other organ involvement [8]. Moreover, due to the risk of late recurrence, long term follow-up is mandatory.
Our case report details a rare presentation of leiomyosarcoma due to its presence in the breast tissue, making it a case of special interest. The patient’s history, the presence of additional sites of metastasis and the mammographic observations supported a preoperative diagnosis of leiomyosarcoma of the breast. The current literature details the challenges faced when diagnosing this neoplasm, especially in patients with no prior history of sarcoma lesions. Moreover, diagnosis and treatment have been historically non-uniform as a result [9]. A definitive diagnosis relies on the results of excisional biopsy or core needle. Table 2 provides an overview of the histological and immunohistochemical findings that aid in diagnosis. The primary origins of the malignancy are predominantly blood vessel smooth musculature, a malignant transformation from benign neoplasms, or smooth muscle of the nipple areolar complex [6,10] (Table 2).
| Histological Characteristics (10, 11) |
|
| Immunohistochemical Staining (6, 10-12) | LMS stains positive for |
|
|
| LMS stains negative for | |
|
Table 2: Overview of the histological and immunohistochemical characteristics that aid in the diagnosis of breast leiomyosarcoma.
Despite the evidence provided in this case report adding to the comprehension of this rare and heterogeneous disease, the rarity of this tumor limits the availability of current literature to small retrospective case reviews and individual case reports. Collectively, this makes clinic pathological study difficult and limits the comparable nature of our findings [11,12]. Moreover, treatment approaches were not discussed beyond diagnosis; hence, evidence cannot be provided concerning recommendations in the treatment of this neoplasm.
In conclusion, in patients presenting with breast abnormalities, a correct and thorough medical history is mandatory to support the differential diagnosis. When the patient has a history of hepatic, left renal and multiple bone metastases, in addition to a diagnosis of metastatic leiomyosarcoma, further investigation is warranted to consider a diagnosis of leiomyosarcoma of the breast, despite the rarity of the presentation of this disease.
References
- Mangla A, Yadav U (2021) Leiomyosarcoma Stat Pearls Treasure Island (FL): Stat Pearls Publishing Copyright © 2021, Stat Pearls Publishing LLC.
- UÄŸraÅŸ S, Dilek ON, Karaayvaz M, Dilek H, Peker O et al. (1997)Â Primary leiomyosarcoma of the breast. Surg Today 27:1082-1085.
- Gronchi A, Ferrari S, Quagliuolo V, Broto JM, Lopez-Pousa A et al. (2016) LBA6_PR - sarcoma Full-dose neo adjuvant anthracycline + ifosfamide chemotherapy is associated with a relapse free survival (RFS) and overall survival (OS) benefit in localized high-risk adult soft tissue sarcomas (STS) of the extremities and trunk wall: Interim analysis of a prospective randomized trial. Ann Oncol 27:587.
- Gronchi A, Ferrari S, Quagliuolo V, Broto JM, Pousa AL et al. (2017)Â Histotype-tailored neo adjuvant chemotherapy versus standard chemotherapy in patients with high-risk soft-tissue sarcomas (ISG-STS 1001): an international, open-label, randomised, controlled, phase 3, multicentre trial. Lancet Oncol 18:812-822.
- Miyazaki C, Shiozawa M, Koike R, Ogihara K, Sasaki Y et al. (2019) Neo adjuvant chemotherapy for primary sarcoma of the breast: a case report. J Med Case Rep 13:289.
- Karabulut Z, Akkaya H, Moray G (2012) Primary leiomyosarcoma of the breast: a case report. J Breast Cancer 15:124-127.
- Al-Benna S, Poggemann K, Steinau HU, Steinstraesser L (2010) Diagnosis and management of primary breast sarcoma. Breast Cancer Res Treat 22:619-629.
- Ilyas MIM, Nazir S, Xiao PQ (2020) Breast Leiomyosarcoma A Systematic Review and Recommendations for Management. Int Surg J 104:196-202.
- Amberger M, Park T, Petersen B, Baltazar GA (2018) Primary breast leiomyosarcoma with metastases to the lung in a young adult: Case report and literature review. Int J Surg Case Rep 47:34-37.
- M Rabet F, Kacemi H, Mesbahi O, Hassouni K, Gueddari B et al. (2017) Primary breast leiomyosarcoma: Case report and literature review. Health 3:620-622.
- Liang WC, Sickle-Santanello BJ, Nims TA, Accetta PA (2003) Primary Leiomyosarcoma of the Breast: A Case Report with Review of the Literature. Breast J 9:494-496.
- Amaadour L, Benbrahim Z, Moumna K, Boudahna L, Amarti A, et al. (2013) Primary Breast leiomyosarcoma. Case Rep Oncol Med 1-4.
Citation: Kavousi M, Stacy Ries DO, Dominic Semaan MD, Ahmed R (2021) Leiomyosarcoma of the Breast: A Case Report. OMICS J Radiol 10: 343. DOI: 10.4172/2167-7964.1000343
Copyright: © 2021 Kavousi M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 3070
- [From(publication date): 0-2021 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 2253
- PDF downloads: 817