Macropephaly-Cutis Marmorata: Case Report and Review of Literature
Received: 04-Mar-2017 / Accepted Date: 22-Mar-2018 / Published Date: 27-Mar-2018 DOI: 10.4172/2476-2024.1000136
Abstract
Macrocephaly - capillary malformation (M-MC) is a rare genetic disorder initially described in 1997. It is associated with a spectrum of abnormalities including macrocephaly, cerebral and body asymmetry, cutaneous vascular malformations and digital anomalies. It is one of several overgrowth syndromes known as the hypertrophic spectrum related to PIK3CA. Children with M-MC syndrome would also have a high cancer risk. Recent recommendations advocate regular abdominal ultrasounds up to eight years of age to detect Wilms tumor. There is no cure for this disease. Care is supportive care and varies depending on the symptoms and their severity. Physiotherapeutic and psychomotor care as well as orthopedic reinforcement can help young children in their overall motor development. Follow-up of an orthopedic surgeon may be necessary for differences in leg length due to hemi hypertrophy and body asymmetry. We report the first observation observed in pediatric medical emergencies of Rabat Children's Hospital with a review of the literature on the clinical, genetic and therapeutic aspects of this syndrome.
Keywords: Hypertrophy; Macrocephaly-capillary malformation; Cutis marmorata; PIK3CA gene
Introduction
Macrocephaly - capillary malformation (M-MC) is a rare genetic disorder initially described in 1997. It associates a spectrum of abnormalities including macrocephaly, cerebral and body asymmetry, cutaneous vascular malformations and digital anomalies. This polymalformative syndrome is also known as megalencephalycapillary- polymicrogyric malformation (M-CAP) or macropephalycutis marmorata telangiectatica congenita (M-CMTC). We report the first observation observed in pediatric medical emergencies of Rabat Children's Hospital with a review of the literature on the clinical, genetic and therapeutic aspects of this syndrome.
Case Report
We describe the observation of a 9-month-old infant, only one of his families from a poorly followed pregnancy from nonconsanguineous parents. He consulted at the age of 6 months for hypotonia.
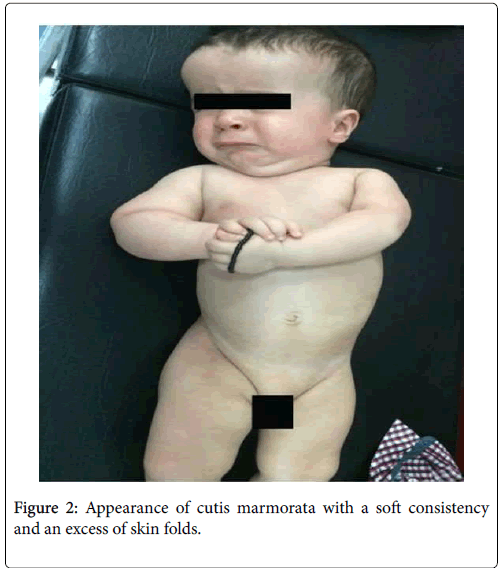
The clinical examination found an axial and peripheral hypotonia with a hemi hypertrophy of the right hemi-body, a macrocephaly with projection of the frontal bumps (53 cm +3 DS) (Figure 1), an appearance of cutis marmorata, a bodily asymmetry with soft consistency hemi-hypertrophy of the right body without underlying vascular abnormalities and excess of skin folds (Figure 2). The osteotendinous reflexes were present and the Babinski was bilateral.
The MRI showed cortical atrophy. Abdominal echocardiography and the urinary shaft revealed hepatomegaly and nephrenomegaly. The fundus examination was normal outside of a hyperemia. There was had no abnormalities on echocardiography and the biological assessment was normal (blood glucose, renal and hepatic function without abnormalities with chromatography of organic acids in the urine) and the karyotype is in progress. In front of this clinical picture: macrocephaly, vascular anomaly and hemi-hypertrophy of the body. The diagnosis of macrocephaly-capillary malformation syndrome was retained.
Discussion
Macrocephaly - capillary malformation (M-MC) was first described by Moore et al. [1], and Clayton-Smith et al. [2]. In 1997 as macrocépahlie-cutis marmorata telegiectasia congenital syndrome (MCMTC) respectively, in 9 and 13 children, all patients had cutis marmorata telangiectatica congenita (CMTC), hypotonia and / or psychomotor retardation, macrocephaly, capillary malformations, 2 to 3 syndactylies of the toes, and connective tissue abnormalities [1,2].
In 2007 this genodermatosis was renamed M-MC by Toriello and Mulliken [3], because the cutaneous lesions were neither cutis marmorata nor CMTC, but a type of capillary malformation in a paricular grid pattern that never improves or ulters and which is sometimes associated with hypertrophic changes [3,4].
Mirzaa et al. [5] suggested the use of the term M-CAP rather than M-CM to reflect the very large brain size (megalencephaly), the importance and frequency of perisylvian polymicrogyria rather than the large size of the head (macrocephaly), which characterizes this syndrome [5].
About 170 cases have been reported in the literature with no predominance of one sex. The estimated prevalence of less than 1/1,000,000m was observed [6].
Riviere et al. [7] reported that the M-MC syndrome is caused by de novo germline mutation or postzygotic mutations in the PIK3CA gene (Figure 1). Positioned on chromosome 3, PIK3CA provides instructions for the formation of the p110 alpha protein (p110α). This protein is a subunit of the anenzyme called phosphatidylinositol 3- kinase (PI3K), which plays a role in chemical signaling in cells. PI3K signaling is important for many cellular activities, including growth and cell division (proliferation), cell movement (migration) and cell survival. These functions make PI3K important for tissue development throughout the body, including the brain and blood vessels (angiogenesis). Mutations in the PIK3CA gene involved in the M-MC syndrome alter the p110α protein. The impaired subunit PI3K is abnormally active, which allows the cells to grow and divide continuously. Increased cell proliferation leads to proliferation of the brain, blood vessels, and other organs and tissues characteristic of MMC syndrome.
M-MC syndrome is one of several overgrowth syndromes known as the hypertrophic spectrum related to PIK3CA [7].
The detection of the PIK3CA anomaly is difficult because of the mosaicism and requires sensitive detection techniques with biopsies of the skin in the affected area, by a smear or a saliva sample.
The diagnosis of M-MC syndrome is clinical and can be supported by the appearance of brain MRI. Several authors have proposed clinical diagnostic criteria. In 2000 Franceschini et al. [8] suggested the least restrictive diagnostic criteria associating macrocephaly with at least two of the following criteria: gigantism, capillary malformation, polydactyly/syndactyly and asymmetry [8].
The last diagnostic criteria were proposed in 2012 by Mirzaa et al. [5]. The symptoms grouped into 5 major classes of developmental abnormalities: Group I progressive megalencephaly and dysregulation of brain growth relative to the body, including selective brain hypertrophy and somatic asymmetry. In this first class two others must be associated. Group II: Capillary malformation of the face and mediocorporelle. Group III: Anomalies of the distal limbs: syndactyly (2-3, 3-4, 2-3-4, toe or finger). Group IV: Cortical malformations: polymicrogyria. Group V: Connective tissue dysplasia: hyperelasticity of the skin, joint hypermobility and thick, pasty subcutaneous tissue [5].
Table 1 summarizes the recently proposed criteria for this diagnosis. In our observation, the diagnosis could be retained by considering one or other of the definitions.
| Diagnostic Criteria | Wright et al. [9]. | Martinez-Glez et al. [10]. | Mirzaa et al. [5]. |
|---|---|---|---|
| Major | 2 criteria required | 3 criteria required | |
| I- Macrocephaly* | I- Macrocephaly* | I- Early growth (brain> somatic tissues). Progressive megalencephaly*. | |
| II- Capillary malformation* | II- Capillary malformation*. | II- Capillary malformation: face and medio-corporal*. | |
| II- Hypertrophy/asymmetry*. IV- Anomaly of neuroimaging: ventruculomegaly, spinal/cerebellar asymmetry, hernia brain tonsils, cavum septum pellucidum or cavum vergae. | III- Abnormalities of the distal limbs. Syndactyly (2-3, 3-4, 2-3-4, toe or finger). | ||
| IV- Cortical brain malformations: Polymicrogyria. | |||
| V- Connective tissue dysplasia*: hyperelasticity of the skin, joint hypermobility and thick, pasty subcutaneous tissue. | |||
| Minor | At least 2 criteria | At least 2 criteria | |
| 1- Medio-facial capillary malformation. | 1- Medio-facial capillary malformation. | 1- Selective overgrowth of the brain: | |
| 2- Developmental delay*. | 2- Developmental delay*. | ventriculomegaly / hydrocephalus. | |
| 3- Neonatal hypotonia*. | 3- Neonatal hypotonia*. | Cerebellar ectopia of the tonsils. | |
| 4- Poly or Syndactylia. | 4- Syndactyly or polydactyly. | Callous (mega) body abnormally thick. | |
| 5- Frontal bumps. | 5- Frontal bumps*. | 2- Somatic and cranial dysplasia*: somatic or cranial asymmetry. | |
| 6- Hydrocephalus. | 6- Hydrocephalus. | ||
| 7- Abnormalities of the connective tissue*. | 7- Abnormal connective tissue*: hypermobility or hyperelastic skin | ||
| 8-Asymmetry/macrosomia. |
*: sign present in our observation
Table 1: Main diagnostic criterias for M-MC syndrome.
Differential diagnosis arises with syndromes associating more or less asymmetric body hypertrophy and cutaneous malformations: Weidman Beckwith's syndrome includes a malio-facial capillary malformation like nevus flammeus associated with neonatal macrosomia, macroglossia, abdominal wall closure, visceromegaly and neonatal hypoglycaemia. In Proteus syndrome, skin abnormality is in the form of very diffuse flat vascular malformations and intense coloration at birth. Klippel-Trenaunay syndrome associates an extensive limb planar angioma associated with excessive development of soft tissues, bones and varicose veins.
There is no cure for this disease. Care is supportive care and varies depending on the symptoms and their severity. Physiotherapeutic and psychomotor care as well as orthopedic reinforcement can help young children in their overall motor development. Follow-up of an orthopedic surgeon may be necessary for differences in leg length due to hemihypertrophy and body asymmetry.
The importance of congenital brain abnormalities and the frequency of complications due to excessive and progressive brain growth i.e. hydrocephalus, tonsillary cerebral hernia (Chiari I), epilepsy and syringomyelia, requires follow-up in neurosurgery with the performing brain imaging (MRI) and spinal imaging to monitor changes caused by excessive and progressive growth of the brain [11].
Children with M-MC syndrome would also have a high cancer risk. Recent recommendations advocate regular abdominal ultrasounds up to eight years of age to detect Wilms tumor [12]. Cardiac monitoring with electrocardiogram and echocardiography is often recommended. Arrhythmias or cardiac abnormalities may require surgical treatment [5].
Conclusion
Potential complications of MMC syndrome demonstrate the interest of making the diagnosis as early as possible. The association in neonatal period of skin abnormalities with a macrocephaly and a macrosomia should do evoke and seek out other stigmas for the purpose to program an adapted surveillance.
Conflict of Interest
The authors declare no competing interest.
References
- Moore CA, Toriello HV, Abuelo DN (1997) Macrocephaly-cutis marmorata telangiectatica congenita: a distinct disorder with developmental delay and connective tissue abnormalities. Am J Med Genet 70: 67-73.
- Clayton-Smith J, Kerr B, Brunner H (1997) Macrocephaly with cutis marmorata, haemangioma and syndactyly - a distinctive overgrowth syndrome. Clin Dysmorphol 6: 291-302.
- Toriello HV, Mulliken JB (2007) Accurately renaming macrocephalycutis marmorata telangiectatica congenita (M-CMTC) as macrocephaly-capillary malformation (M-CM). Am J Med Genet A 143A: 3009.
- Wright DR, Frieden IJ, Orlow SJ (2009) The Misnomer “Macrocephaly- Cutis Marmorata Telangiectatica Congenita Syndromeâ€. Report of 12 new cases and support for revising the name to macrocephaly – capillary malformations. Arch Dermatol 145: 287-93.
- Mirzaa GM, Conway RL, Gripp KW, Lerman-Sagie T, Siegel DH, et al. (2012) Megalencephaly-capillary malformation (MCAP) and megalencephaly-polydactyly-polymicrogyria-hydrocephalus (MPPH) syndromes: two closely related disorders of brain overgrowth and abnormal brain and body morphogenesis. Am J Med Genet A 158A: 269-91.
- (2018) Prévalence des maladies rares: Données bibliographiques. Les Cahiers d’Orphanet
- Riviere JB, Mirzaa GM, O'Roak BJ, Beddaoui M, Alcantara D, et al. (2012) De novo germline and postzygotic mutations in AKT3, PIK3R2 and PIK3CA cause a spectrum of related megalencephaly syndromes. Nat Genet 44: 934-40.
- Franceschini P, Licata D, Di Cara G (2000) Macrocephaly-cutis marmorata telangiectatica congenita without cutis marmorata? Am J Med Genet 90: 265-269.
- Wright DR, Frieden IJ, Orlow SJ, Shin HT, Chamlin S, et al. (2009) The misnomer "macrocephaly-cutis marmorata telangiectatica congenita syndrome": report of 12 new cases and support for revising the name to macrocephaly-capillary malformations. Arch Dermatol 145: 287-293.
- Martinez-Glez V, Romanelli V, Mori MA, Gracia R, Segovia M, et al. (2010) Macrocephaly-capillary malformation: analysis of 13 patients and review of the diagnostic criteria. Am J Med Genet A 152A: 3101-3106.
- Segal D, Robert F, Sabharwal S, Barry MT, Ming X (2016) Severe holocord syrinx in a child with megalencephaly-capillary malformation syndrome. J Neurosurg Pediatr. 18: 79-82.
- Peterman CM, Vadeboncoeur S, Mulliken JB, Fishman SJ, Liang MG (2017) Wilms tumor screening indiffuse capillary malformation with overgrowth and macrocephaly-capillary malformation: Aretrospective study. J Am Acad Dermatol. 77: 874-878.
Citation: Laaraje A, Mekaoui N, Karboubi L, Dakhama BSB. (2018) Macropephaly-Cutis Marmorata: Case Report and Review of Literature. Diagn Pathol Open 3: 136. DOI: 10.4172/2476-2024.1000136
Copyright: © 2018 Laaraje A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 6011
- [From(publication date): 0-2018 - Nov 22, 2025]
- Breakdown by view type
- HTML page views: 5050
- PDF downloads: 961