Case Report Open Access
Management of Impacted 2nd Premolar Impaction by Buccal Approach: A Case Report
Dipti Shastri*, Pradeep Tandon, Gyan P Singh and Alka Singh
Department of Orthodontics and Dentofacial Orthopaedics, King George’s Medical University, Lucknow, Uttar Pradesh, India
- *Corresponding Author:
- Dipti Shastri
Department of Orthodontics and Dentofacial Orthopaedics
Faculty of Dental Sciences, King George’s Medical University
Lucknow, Uttar Pradesh, India
Tel: 9235768813
E-mail: drdiptishastri@gmail.com
Received date: April 14, 2014; Accepted date: May 30, 2014; Published date: June 06, 2014
Citation: Dipti Shastri, Pradeep Tandon, Gyan P Singh, Alka Singh (2014) Management of Impacted 2nd Premolar Impaction by Buccal Approach: A Case Report. J Interdiscipl Med Dent Sci 2:124. doi:10.4172/2376-032X.1000124
Copyright: © 2014 Shastri D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
This case report presents treatment of a distally impacted mandibular 2nd premolar having a 90° tilt to the long axis of the tooth. In this 16 year old girl radiological finding described that horizontally impacted mandibular second premolar was positioned below the roots of the mandibular first molar. Due to the abnormal position of impacted premolar, it was planned to be removed surgically. Finally, the horizontally impacted mandibular second premolar was extracted without any injury to the mental nerve.
Keywords
Impacted premolar; Surgical removal; Buccal approach; Mental nerve
Introduction
An impacted tooth is one that is embedded in the alveolus and not erupted in scheduled time, and its eruption is prevented or the tooth is locked in position by bone or the adjacent teeth [1]. Mandibular second premolars rank third, after third permanent molars and maxillary permanent canines, in frequency of impaction [2]. The prevalence of impacted premolars has been found to vary according to age.3 The overall prevalence in adults has been reported to be 0.5% (the range is 0.1% to 0.3% for maxillary premolars and 0.2% to 0.3% for mandibular premolars) [3,4].
Mandibular second premolars alone account for 24% of all dental impactions excluding molars [5,6]. Premolar impactions may be due to local factors e.g. mesial drift of teeth by premature loss of primary molars, ectopic positioning of premolar buds; or pathology e.g. dentigerous cyst [2,7]. Various treatment methods have been suggested including observation, interceptive orthodontics, surgical exposure with orthodontic intervention, auto-transplantation and extraction depending on position of impacted tooth, relationship with adjacent teeth and need for orthodontic treatment [1,5,6].
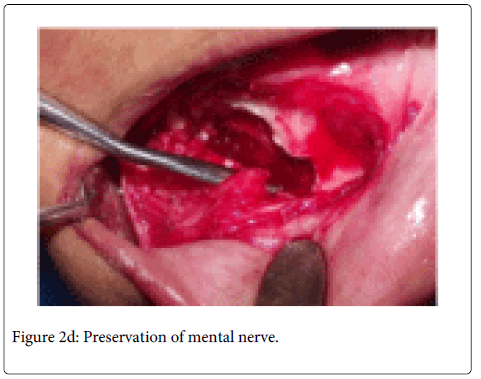
Based on the clinical findings where palpation by fingers suggested thin layer of cortical bone over the impacted premolar and orthopantomogram was used to locate the impacted tooth. The described case presented with the most unfavourably placed buccally impacted mandibular premolar due to presence of crowding and the impacted premolar crossing more than half of the mesial root of mandibular right 1st molar. Had we attempted to correct the impacted tooth it might have led to resorption of the adjacent root. The only option left was simply extracting the impacted premolar. The extraction of impacted premolar was done via buccal approach to prevent the injury of mental nerve as the mental foramen is situated just apical to the mandibular second premolar. Anterior loop of the mental nerve is generally present mesial to the mental foramen [8] and needs to be considered before the extraction of impacted second premolar else, even mild compression may lead to parenthesia or dysaesthesia of lip and chin region [9] whereas if the nerve is completely severed then permanent paresthesia can results [10].
Case
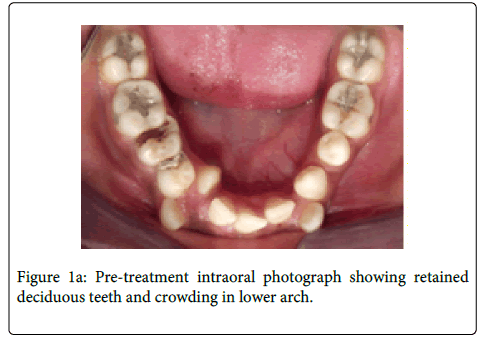
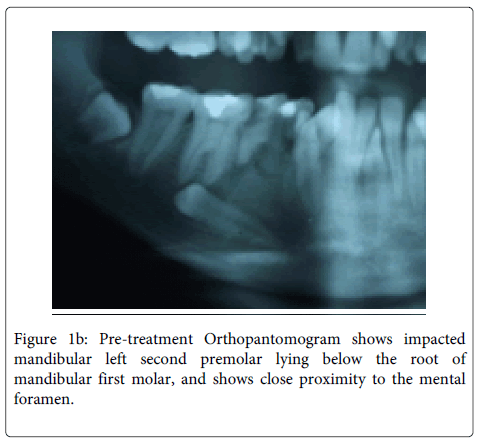
A 16-year-old female was referred to the department with multiple retained deciduous teeth. On clinical evaluation, unilateral missing mandibular 2nd premolar tooth was observed (Figure 1a) besides crowding in the mandibular arch. On radiological evaluation (OPG), it was observed that the mandibular right second premolar was impacted in horizontal position with its crown lying below the furcation of mandibular first molar (Figure 1b). Due to abnormal positioning of the impacted premolar, it was not possible to bring this tooth in the arch with conventional orthodontic traction with or without surgical intervention. The auto-transplantation was also not possible for this tooth due to its peculiar position and lack of space in the arch. So, it was decided to extract the mandibular right second premolar. Extreme care needed to be taken before its extraction due its close proximity to the mental nerve. Due to the buccal positioning of the impacted tooth it was decided to adopt buccal surgical approach for the removal of the impacted tooth.
Procedure
After achieving proper local anaesthesia, incision was made with Bard Parker blade # 15 in the gingival crevice on the buccal aspect of right mandibular second premolar
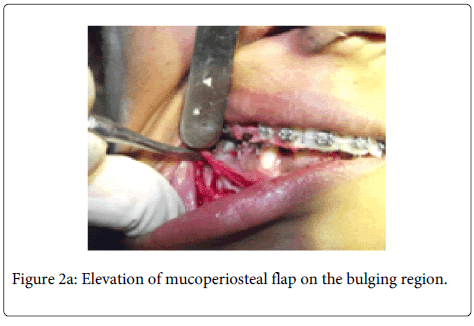
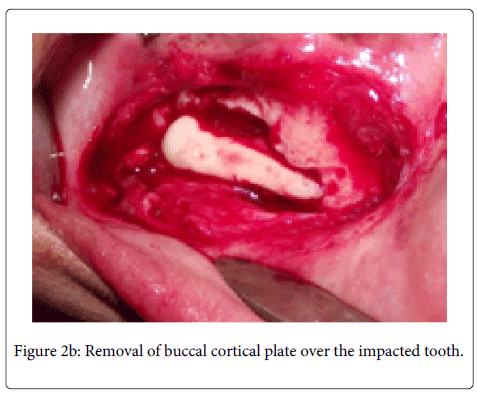
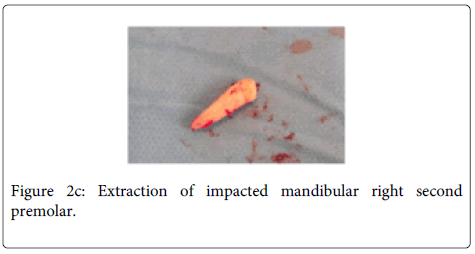
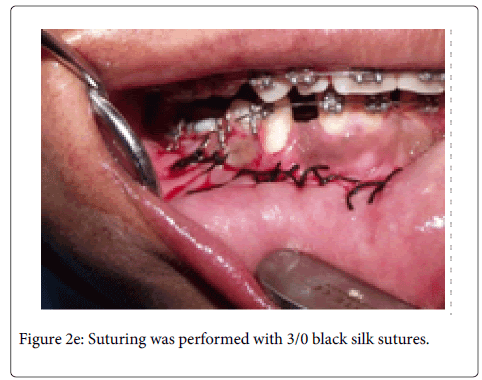
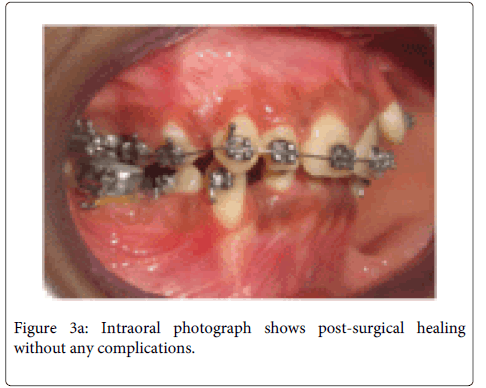
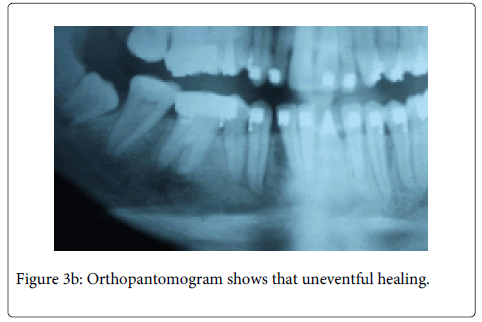
tooth. A full thickness mucoperiosteal flap was raised with Molt periosteal elevator (Figure 2a). The bone bulge on buccal cortex due to crown of impacted tooth was identified and decortication of buccal cortex was carried out with surgical hand piece & round bur under coolant irrigation. Initially we attempted to remove the tooth by sectional method, but due to the horizontal position of the impacted tooth, and a single thin layer of cortical plate over the tooth, the whole buccal cortical plate was removed over the impacted tooth (Figure 2b). Then the tooth was extracted while preserving the mental nerve (Figure 2c and 2d). The wound was irrigated with normal saline and flap was repositioned. Suturing was performed with 3/0 black silk suture. Suture was removed after seven days (Figure 2e). Post-surgical healing was good without any complications (Figure 3a and 3b).
Discussion
Treatment options for impacted teeth include observation, intervention, relocation, and extraction. On occasions, there may be some interaction between these treatment options [6]. Mandibular 2nd premolars alone account for approximately 24% of all the dental impactions [11].
In selecting an appropriate treatment option, the underlying etiological factors, space requirements, need for extractions of primary molars, degree of impaction, and root formation of the impacted premolar should be considered. Factors such as patient’s medical history, dental status, oral hygiene, functional and occlusal relationship and attitude towards and compliance with treatment will influence choice of treatment options [11-13]. In this case, the impacted tooth positioned approximately 90° to the long axis and crown of the tooth and positioned below the root apices of the first permanent molar with complete root formation. It was close to the mental foramen, and with such a reduced level of available dentoalveolar bone monitoring was ruled out as a choice of treatment as at 16 years of age growth potential had ceased.
The position of the horizontally placed impacted right mandibular second premolar was so unfavorable that no orthodontic treatment of this tooth was envisaged, and hence extraction was planned with precaution to prevent the injury of mental nerve.
Andreasen et al. [3] suggests that surgical exposure should be confined to cases, both maxillary and mandibular with no more than 45 tilting and limited deviation from the normal position, and hence this case definitely required removal of the impacted tooth. As the crown was on the buccal aspect, the buccal approach with removal of tooth was the choice. Care should be taken as; the buccal flap would have jeopardized the mental nerve emerging from the mental foramen and the apices of the first permanent molar tooth. But due to complete removal of tooth with precise removal of buccal cortical plate over the impacted mandibular right second premolar injury to mental nerve was prevented. Careful irrigation of the surgical area to clear any bone and tooth dust in that area prevented any delay in healing and infection.
Correct knowledge of regional anatomy, careful manipulation of tissues, and correct application of mechanical principles involved in tooth extraction provided surgical success. This peculiar and rare case may contribute towards the minimal literature available regarding impacted second premolar tooth and offers buccal approach as a treatment method while preventing injury to the mental nerve.
References
- John P Friel (1974) Dorlands’ illustrated medical dictionary. (25th edn), WB Saunders company, Philadelphia, London.
- Alling CC 3rd, Catone GA (1993) Management of impacted teeth. J Oral Maxillofac Surg 51: 3-6.
- Andreasen JO, Petersen JK, Laskin DM (1997) Textbook and color atlas of tooth impactions; diagnosis, treatment and prevention.
- Oikarinen VJ, Julku M (1974) Impacted premolars. An analysis of 10 000 orthopantomograms. Proc Finn Dent Soc 70: 95-98.
- Jain U, Kallury A (2011) Conservative Management ofMandibular Second Premolar Impaction. J Scient Res 4: 59-61.
- Frank CA (2000) Treatment options for impacted teeth. J Am Dent Assoc 131: 623-632.
- Kumar Mohapatra P, Joshi N (2009) Conservative management of a dentigerous cyst associated with an impacted mandibular second premolar in mixed. J Dent Res Dent Clin Dent Prospects 3: 98-102.
- Abbott PV (1997) Lower lip paraesthesia following restoration of a second premolar tooth. Case report. Aust Dent J 42: 297-301.
- Becelli R, Renzi G, Carboni A, Cerulli G, Gasparini G (2002) Inferior alveolar nerve impairment after mandibular sagittal osteotomy. An analysis of spontaneous recovery patterns observed in 60 patients. J Craniofac Surg 13: 315-320
- Seddon HJ (1943) Three types of nerve injury. Brain 66: 237-288.
- Collett AR (2000) Conservative management of lower second premolar impaction. Aust Dent J 45: 279-281.
- Kokich VG, Mathews DP (1993) Surgical and orthodontic management of impacted teeth. Dent Clin North Am 37: 181-204.
- W. R. Proffit, Field H W (2000) Contemporary Orthodontics. (3rd edition), St. Louis, USA.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 23788
- [From(publication date):
June-2014 - Aug 24, 2025] - Breakdown by view type
- HTML page views : 18702
- PDF downloads : 5086