Case Report Open Access
Mediastinal Widening: An Unusual Presentation of Achalasia Cardia
Javier Martínez-González*, Martínez-González J, Aicart-Ramos M, Tellez-Villajos L, Rodríguez de Santiago E and Albillos ADepartment of Gastroenterology and Hepatology, University of Alcalá, Madrid, Spain
- *Corresponding Author:
- Javier Martínez-González
Department of Gastroenterology and University of Alcalá
} Madrid, Spain
Tel: 34 609881580
E-mail: martinez.gonzalez.javier@gmail.com
Received date: June 24, 2014; Accepted date: October 09, 2014; Published date: October 15, 2014
Citation: Martínez-González J, Martínez-González J, Aicart-Ramos M, Tellez-Villajos L, Rodríguez de Santiago E, et al. (2014) Mediastinal Widening: An Unusual Presentation of Achalasia Cardia. J Gastroint Dig Syst 4:227. doi:doi: 10.4172/2161-069X.1000227
Copyright: © 2014 Martínez-González J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
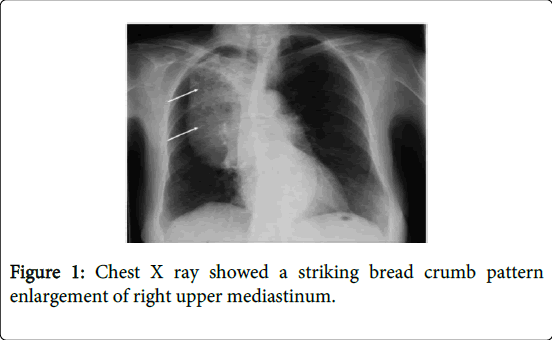
Achalasia typically presents with dysphagia and regurgitation of undigested food. Diagnosis is usually performed with esophageal manometry before macroscopic anatomical changes appear. However some patients do not consult with early symptoms. We present a 55-year old women whose diagnosis was suspected with chest-x-ray showing a striking bread crumb pattern enlargement of right upper mediastinum. Diagnosis was then confirmed with upper endoscopy and manometry. After the failiure of some previous treatments, surgery finally controlled the symptoms.
Abstract
Achalasia typically presents with dysphagia and regurgitation of undigested food. Diagnosis is usually performed with esophageal manometry before macroscopic anatomical changes appear.
However some patients do not consult with early symptoms. We present a 55-year old women whose diagnosis was suspected with chest-x-ray showing a striking bread crumb pattern enlargement of right upper mediastinum. Diagnosis was then confirmed with upper endoscopy and manometry. After the failiure of some previous treatments, surgery finally controlled the symptoms.
Keywords
Achalasia; Disphagia; Barium swallow; Heller myotomy; Pneumatic dilatation; Botulinum toxine injection
Case Report
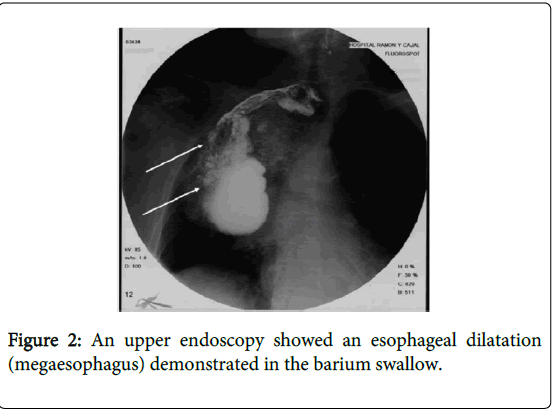
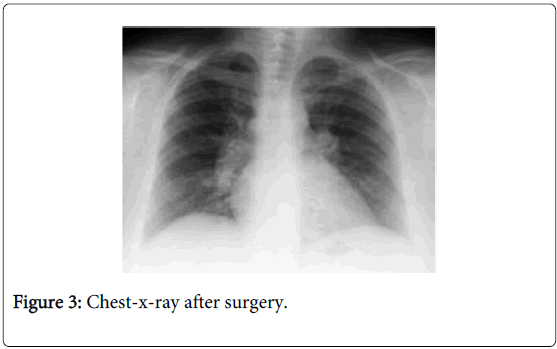
Question: A 1959 born woman first consulted in 2001 presenting progressive dysphagia and regurgitation for 1.5 years. Chest X ray showed a striking bread crumb pattern enlargement of right upper mediastinum (Figure 1) and an upper endoscopy showed an esophageal dilatation (megaesophagus) demonstrated in the barium swallow (Figure 2). These previous techniques can differentiate between diverticulum or megaesophagus anatomical presentation of achalasia. Manometry displayed low-amplitude simultaneous body contractions and failed relaxation of the lower esophageal sphincter (LES). Diagnosis of achalasia was done. Treatment began with pneumatic dilatations performed every 6 months, but they become useless in 2005. Botulinum toxin injection was performed 3 times a year until 2007, but it was also not efficacious in treating symptoms any more. Finally, surgery was performed in 2008. An open surgery with Heller myotomy was combined with a partial (180º) anterior Dor´s funduplication. Intraoperative findings consisted on distal esophagus stenosis and mild dilated and sigmoid oesophagus. The patient has remained mostly asymptomatic until now. Figure 3 shows chest-x-ray after surgery.
Answer to the Clinical Challenges and Images in GI Question: Achalasia is characterized by insufficient LES relaxation and loss of peristalsis1. It is shown in less than 0.2% of all upper endoscopies. The mean age at diagnosis is usually over 50 years. Esophageal manometry is key to diagnosis [1]. Treatment options are multiple, but randomized controlled trials are few, so decisions are based on local expertise, patient performance status and patient and physician preferences [1,2]. In those patients who fit and willing to undergo surgery either a pneumatic dilation protocol or a laparoscopic surgical myotomy with a partial funduplication as the first treatment are recommended. These techniques should be performed in high-volume centers of excellence. Laparoscopic Heller myotomy presents serious complications in <10%; surgery related death is extremely rare and over 80% of patients remain asymptomatic 5 years after surgery. Pneumatic dilation has a 2% perforation rate and a long term response rate of 67-83% [1,3,4].
There are two other alternative treatments. Botulinum toxin injection, which is recommended in patients who are not good candidates for pneumatic dilation or surgery, is a safe procedure, but over 50% relapse after 6 months, requiring multiple injections. Pharmacological treatments (calcium channel blockers, phosphodiestetase-5-inhibitor,anticholinergic agents) are the last alternative, and is employed when dilation or surgery cannot be performed and when botulinum injection has failed [2-4].
Although an excess risk of carcinoma (standardized incidence ratio: 10.5, 95 % CI 7.0-15.9) has been observed in operated and non-operated patients, making upper endoscopy a first line investigation in symptomatic relapse, guidelines do not support surveillance [2].
References
- Vaezi MF, Pandolfino JE, Vela MF (2013) ACG clinical guideline: diagnosis and management of achalasia. Am J Gastroenterol 108: 1238-1249.
- Lake JM, Wong RK (2006) Review article: the management of achalasia - a comparison of different treatment modalities. Aliment PharmacolTher 24: 909-918.
- Campos GM, Vittinghoff E, Rabl C, Takata M, Gadenstatter M, et al. Endoscopic and surgical treatments for achalasia: a systematic review and meta-analysis. Ann Surg 2009; 249:45-57.
- Rebecchi F, Giaccone C, Farinella E, Campaci R, Morino M (2008) Randomized controlled trial of laparoscopic Heller myotomy plus Dor fundoplication versus Nissen fundoplication for achalasia: long-term results. Ann Surg 248: 1023-1030.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 15492
- [From(publication date):
October-2014 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 10839
- PDF downloads : 4653